Clinical and Pathological Features of Riedel’s Thyroiditis
Lin Lu ,Feng Gu *,Wei-xin Dai ,Wu-yi Li ,Jie Chen ,Yu Xiao ,and Zheng-pei Zeng
1Department of Endocrinology,Key Laboratory of Endocrine and Metabolic Diseases of Ministry of Health,
2Department of Otorhinolaryngology,
3Department of Pathology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
RIEDEL’S thyroiditis(RT),also called chronic fibrous thyroiditis or woody thyroid it is,was first described by Bernhard Riedel in 1896,characterized by extension of fibrous tissue and destruction of normal thyroid tissue.RT typically presents with solid enlargement of the thyroid gland (described as stonehard consistency),and is often tightly adhered to surroundding tissues,causing dyspnea,dysphagia,repetitive recurrent laryngeal nerve paralysis,and hypothyroidism.1The etiology of this disease is still elusive,and it is often difficult to differentiate RT from undifferentiated thyroid carcinoma,lymphoma,or fibrous variant of Hashimoto’s thyroiditis (HT)in physical examination.2-4In addition,this disease has rarely been reported,with one of the largest relevant studies having found only 37 RT cases in 57 000 thyroidectomies reviewed.5Women are four times more likely to be affected than men,and RT most commonly occurs in population between 30 and 50 years of age.6In this study,we reviewed five RT cases and the relevant literature to identify the clinical and pathological features of this rare disease.
PATIENTS AND METHODS
Patients’ data collection
We retrospectively search the term“chronic fibrous thyroiditis”,“Riedel’s thyroiditis”,or“woody thyroiditis”in the database of Peking Union Medical College Hospital which was introduced in 1985.From the data between 1985 and 2009,five cases of RT were identified based on the findings from surgery and pathological examinations in the hospital.The clinical and pathological features of the five cases were compared with those reported in literature.
Immunohistochemical staining
It has been suggested that immunohistochemical profiles of RT has unique features,7,8which is helpful in distinguishing RT from other thyroiditis.For instance,the ratio of kappa to lambda light chain in fibrous variant of HT is similar to that in normal circulation (2∶1),while in RT tissue the proportion of lambda-containing cells is markedly higher.Therefore,the tissues from the 5 cases were processed by immunohistochemical staining of kappa and lambda light chains.The experiments were performed using the labeled streptavidin-biotin-peroxidase complex method with DAB as chromogen.Four-μm-thick sections of each formalin-fixed,paraffin-embedded tissue block was deparaffinized by dimethylbenzene,and then incubated in 3% H2O2ethanol to block endogenous peroxidase activity.After washing in phosphate buffered saline (PBS),the sections were incubated with the primary antibody to kappa chain (1∶200,Dako,Denmark) or lambda chain (1∶200,Dako) for 30 minutes at room temperature.It was followed by incubation with goat anti-rabbit serum for 30 minutes at room temperature.The sections were counterstained with hematoxylin.As a control for the immunostaining,PBS was used instead of the primary antibody.Three samples were examined for each tissue of all the cases.
RESULTS
Clinical features
The identified five patients were all middle-aged (45-55 years) females with enlarged thyroid glands (grade II-III)and a disease course ranging from 0.5 to 30 months.The cases were numbered in sequence of the date of their hospitalization.Serious neck pain accompanying tracheal compression occurred in two patients (cases 2 and 3),and recurrent laryngeal nerve paralysis and dysphagia were evident in one patient (case 3).Notably,case 3 exhibited hypothyroidism prior to surgery and received oral thyroxin.
Serum levels of antithyroid antibodies were normal in four patients (cases 1,2,4,and 5) while elevated in case 3.In the two patients (cases 1 and 3) who underwent thyroid iodine uptake examinations,the uptake rate was found decreased.In the three patients (cases 1,3,and 4) who received thyroid Tc99 scanning,single or multiple cold nodules were detected.
Partial thyroidectomy was carried out in all the 5 patients to identify the diagnosis or to relieve compressive symptoms.One patient (case 3) was found hypothyroid whereas the other four were euthyroid before surgery.Only one patient (case 3) was detected with moderately elevated antithyroglobulin (TGAb) and antimicrosomal antibodies (TMAb).No fibrous sclerosis was observed beyond the thyroid in any of the 5 patients.In all the five patients,we found that leucocytes in peripheral circulation were at normal levels and erythrocyte sedimentation rate was mildly elevated.
The general information and results of examinations are listed in Table 1.Pathological findings identified the diagnosis of RT in all the 5 cases.
Pathological features
Microscopic evidence of RT included destruction of thyroid follicles,hyperplasia of fibrous connective tissue,and infiltration of lymphocytes.It was also found that inflammatory cells and fibrous tissue extended into surrounding fatty tissue,skeletal muscle,and nervous tissue,resulting in occlusive vasculitis (Figs.1A-D).For compareison,the most common pathological features of HT,as shown in Figure 1E,include small/atrophic thyroid follicles,dense or absent colloid tissue,and lymphoplasmacytic infiltration,with well-developed germinal centers in nodules and atrophic follicles,and variable degrees of interlobular fibrosis.In addition,mononuclear cells aggregated in the perivascular spaces in the HT tissue.As the clinical symptoms were more prominent in case 3,we compared her pathological features with the other 4 patients.More occlusive vasculitis and more organizing vasculitis were found in the RT tissue of case 3,indicating the particularity of her pathological features and severity of her condition.
The result of immunohistochemical staining showed that an average of 16.4% cells contained kappa chains and
30.8% cells contained lambda chains in RT tissues,the latter proportion moderately increased (Fig.2).
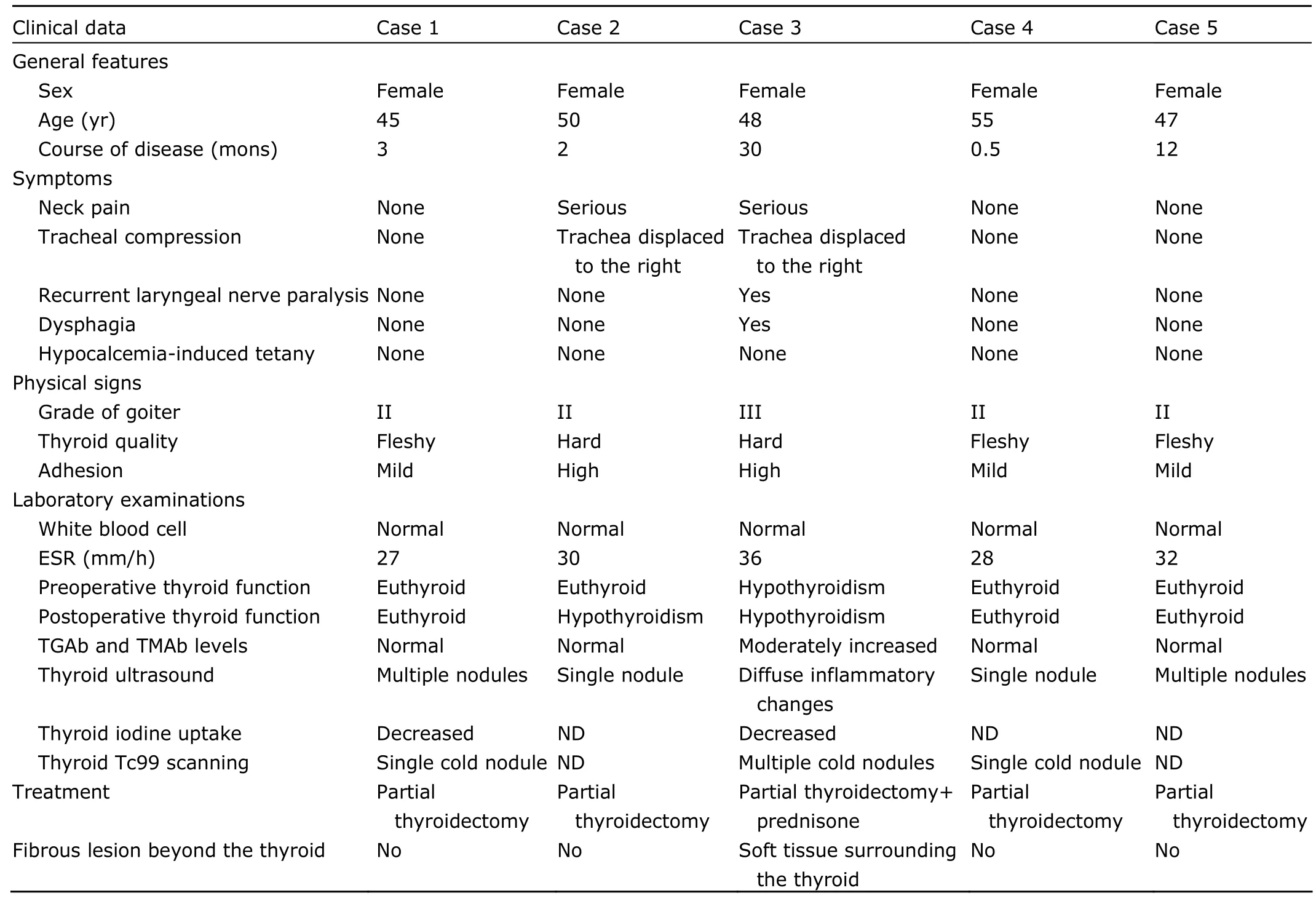
Table 1.Clinical features of the five Riedel’s thyroiditis cases

Figure 1.Microscopic pictures of Riedel’s thyroiditis (A-D) and Hashimoto’s thyroiditis (E).HE staining
Treatment and follow-up
All the five patients received partial thyroidectomy.The neck pain in two patients (cases 2 and 3) was alleviated immediately after surgery.Case 2 developed hypothyroidism after surgery while the preoperative hypothyroidism in case 3 persisted after surgery.Moreover,neck pain recurred in case 3 and several nodules were found 2 months after surgery.These symptoms were obviously mitigated after prednisone treatment (30 mg/d) for 2 weeks with a follow-up period of 36 months.Up to December,2009,no malignant thyroid lesions were observed in the follow-up period of the 5 cases.
DISCUSSION
RT is a rare type of thyroid disease with an estimated incidence of 0.06%,the etiology of which has not been clarified yet.It has been suggested that an autoimmune mechanism is involved in the etiology of RT.9It was shown in a quantitative immunohistochemical study that the cells containing lambda chains outnumbered kappa chaincontaining cells (71%vs.29%),and that the number of IgG-containing cells was comparable to IgA-containing cells (53%vs.47%) in tissues of RT.10The similar result in kappa and lambda chains was observed in our study,though showing only slight difference (30.8%vs.16.4%).It was also reported that the total counts of heavy and light chains per field were much higher in HT than those in RT,with a ratio of 6∶1 for the heavy chains combined and 5∶1 for the light chains combined.11The differences between HT and RT in the proportions of various immunoglobulin-containing cell types raise the possibility that an autoimmune mechanism,different from that seen in the former thyroiditis,may be relevant to the etiology of RT.
As RT is sometimes associated with mediastinal and retroperitoneal fibrosis as well as and sclerosing cholangitis,it is now believed that RT is probably a local manifestation of idiopathic multifocal fibrosclerosis.12,13Although no multifocal fibrosclerosis were found beyond the thyroid in our group of patients,further follow-up is still needed to clarify the existence or absence of other fibrosis foci.
A previous report identified a patient series with a mean age of 47.8 years and a female preponderance of 83%,7similar as the age and sex structure of the patient group in our study.The course of RT may range from months to years,and the patients typically present with painless thyroid mass.14Two of our patients (cases 2 and 3)had neck pain and local tenderness,but no fever on physical examination.The neck pain was relieved immediately after partial thyroidectomy,indicating that RT,not subacute thyroiditis,accounted for that symptom in those two patients.
Schwaegerle et al7reviewed 178 previously reported cases,of which 64% presented with euthyroidism,32%with hypothyroidism,and 4% with hyperthyroidism,similar with the proportion in the present study.In addition,the serum levels of TGAb and TMAb in RT patients were reported to be either normal or slightly elevated,15the same as we observed in the present study.The high percentage of euthyroidism as well as the normal levels of TGAb and TMAb in RT form a contrast with HT.Concurrent HT and RT were reported for several times in the literature.16,17Pathological features of this rare coincidence demonstrated extensive replacement of the thyroid parenchyma with dense keloidal fibrosis,intermixed well-developed lymphoid follicles,scattered lymphocytes and plasma cells.The fibrotic process extended into the perithyroidal soft tissues and skeletal muscle with complete obliteration of the thyroid capsule.Based on those previous observations,case 3 in this study could not be considered as concurrent RT and fibrous variant of HT,as intact or well-developed follicles were not seen in diffuse fibrosis.
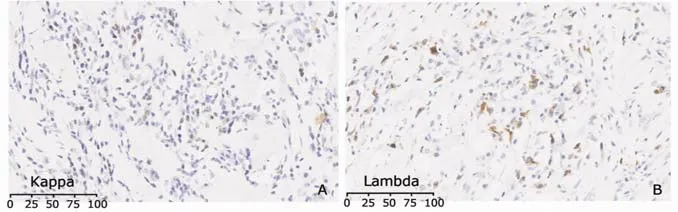
Figure 2.Immunostaining of kappa (A) and lambda chains (B) in Riedel’s thyroiditis.DAB ×400 The number of lambda-containing cells exceeds that of cells containing kappa chains.
RT in the early stage was difficult to differentiate from other chronic thyroiditis;on the other hand,RT in the late stage may develop compressive symptoms such as dyspnea,dysphagia,and vocal cord paralysis due to extension of inflammatory cells into surrounding tissues and adhesion of the thyroid gland to adjacent tissues,imposing difficulty on clinical differentiation from malignancy.18Of the five patients in this study,only one patient (case 3) was distinguished based on her typical symptoms after long disease duration (30 months).The other 4 patients with shorter disease duration did not have such typical manifestations.Before surgery,none of the five cases in this study were diagnosed as RT solely based on the clinical manifestations.Because fine needle aspiration was not widely applied in our hospital until 2003,the diagnosis of RT in the present study was confirmed by pathological findings after surgery.The well accepted and established pathological criteria for RT include:(1) gross description of a visible fibro-inflammatory process involving all or a portion of the thyroid gland;(2) gross and/or histological evidence of extension into adjacent structures;(3) absence of granulomatous reaction;and (4) absence of neoplasm.6In addition,histological examination of RT often reveals invasion of collagen-rich fibrous bands into shrinking or disappearing damaged follicles.Apart from the existence of shrinking or atrophic follicles,another histological indicator distinguishing RT from the fibrous variant form of HT is the extension of fibrosis into structures beyond thyroid.For confirmation,pathological examination is necessary to identify the property of thyroid nodules.
In treating RT,high dose of glucocorticoids was recommended as the first-line therapy for patients with confirmed diagnosis.19Our findings also proved the effectiveness of prednisone.Tamoxifen has also been proved effective for some patients resistant to glucocorticoids or prohibited to use them,possibly through stimulating production of transforming growth factor-beta and inhibiting fibroblastic proliferation.20,21However,in the case of suspected carcinoma and serious compressive symptoms,surgical treatment should also be considered to both confirm diagnosis and relieve symptoms.22
In conclusion,RT is a rare chronic thyroiditis,which manifests euthyroidism,and normal levels of TGAb and TMAb in most cases.Differentiation from other chronic thyroiditis in the early stage and thyroid malignancies in the end stage is difficult if given only clinical signs and laboratory results.Hence we suggest that for middle-aged female patients presenting with a hard thyroid mass,especially those with accompanying compressive neck symptoms,pathological examinations of the thyroid and advanced examinations with emphasis on extensive fibrosis may help in diagnosis.When confirmed,glucocorticoid could be prescribed as the first-line medication,or replaced by tamoxifen in the case of resistance or contraindication.For serious compression or suspected carcinoma,surgical procedure could be provided.Careful long-term follow-up is necessary to prevent recurrence,subsequent complications,and thyroid malignancies.
1.Papi G,Corrado S,Cesinaro AM,et al.Riedel’s thyroiditis:clinical,pathological and imaging features.Int Clin Pract 2002;56:65-7.
2.Cho MH,Kim CS,Park JS,et al.Riedel’s thyroiditis in a patient with recurrent subacute thyroiditis:a case report and review of the literature.Endocr J 2007;54:559-62.
3.Shahi N,Abdelhamid MF,Jindall M,et al.Riedel’s thyroiditis masquerading as anaplastic thyroid carcinoma:a case report.J Med Case Reports 2010;20:15.
4.Fontaine S,Gaches F,Lamant L,et al.An unusual form of Riedel’s thyroiditis:a case report and review of the literature.Thyroid 2005;15:85-8.
5.Hay ID.Thyroiditis:a clinical update.Mayo Clin Proc 1985;60:836-43.
6.Beahrs OH,McConahey WM,Woolner LB.Invasive fibrous thyroiditis (Riedel’s struma).J Clin Endocrinol Metab 1957;17:201-20.
7.Schwaegerle SM,Bauer TW,Esselstyn CB.Riedel’s thyroiditis.Am J Clin Pathol 1988;90:715-22.
8.Munro JM,van der Walt JD,Cox EL,et al.A comparison of cytoplasmic immunoglobulins in retroperitoneal fibrosis and abdominal aortic aneurysms.Histopathology 1986;10:1163-9.
9.Papi G,LiVolsi VA.Current concepts on Riedel thyroiditis.Am J Clin Pathol 2004;121:S50-63.
10.LiVolsi VA.The pathology of autoimmune thyroid disease:a review.Thyroid 1994;4:333-9.
11.Harach HR,Williams ED.Fibrous thyroiditis—an immunopathological study.Histopathology 1983;7:739-51.
12.Brihaye B,Lidove O,Sacré K,et al.Diffuse periarterial involvement in systemic fibrosclerosis with Riedel’s thyroiditis,sclerosing cholangitis,and retroperitoneal fibrosis.Scand J Rheumatol 2008;37:490-2.
13.Kotilainen P,Airas L,Kojo T,et al.Riedel’s thyroiditis in a patient with multiple sclerosis.Neuro Endocrinol Lett 2005;26:67-8.
14.Yasmeen T,Khan S,Patel SG,et al.Riedel’s thyroiditis:report of a case complicated by spontaneous hypoparathyroidism,recurrent laryngeal nerve injury,and Horner’s syndrome.J Clin Endocrinol Metab 2002;87:3543-7.
15.Zelmanovitz F,Zelmanovitz T,Beck M,et al.Riedel’s thyroiditis associated with high titers of antimicrosomal and antithyroglobulin antibodies and hypothyroidism.J Endocrinol Invest 1994;17:733-7.
16.Papi G,Corrado S,Carapezzi C,et al.Riedel’s thyroiditis and fibrous variant of Hashimoto’s thyroiditis:a clinicopathological and immunohistochemical study.J Endocrinol Invest 2003;26:444-9.
17.Baloch ZW,Feldman MD,LiVolsi VA.Combined Riedel’s disease and fibrosing Hashimoto’s thyroiditis:a report of three cases with two showing coexisting papillary carcinoma.Endocr Pathol 2000;11:157-63.
18.Slatosky J,Shipton B,Wahba H.Thyroiditis:differential diagnosis and management.Am Fam Physician 2000;61:1047-52,1054.
19.Moulik PK,Al-Jafari MS,Khaleeli AA.Steroid responsiveness in a case of Riedel’s thyroiditis and retroperitoneal fibrosis.Int J Clin Pract 2004;58:312-5.
20.Jung YJ,Schaub CR,Rhodes R,et al.A case of Riedel’s thyroiditis treated with tamoxifen:another successful outcome.Endocr Pract 2004;10:483-6.
21.Pritchyk K,Newkirk K,Garlich P,et al.Tamoxifen therapy for Riedel’s thyroiditis.Laryngoscope 2004;114:1758-60.
22.Lorenz K,Gimm O,Holzhausen HJ,et al.Riedel’s thyroiditis:impact and strategy of a challenging surgery.Langenbecks Arch Surg 2007;392:405-12.
 Chinese Medical Sciences Journal2010年3期
Chinese Medical Sciences Journal2010年3期
- Chinese Medical Sciences Journal的其它文章
- Cicatricial Pemphigoid in Accompany with Rheumatoid Arthritis:a Case Report
- Non-Hodgkin’s Lymphoma Primarily Presenting with Fanconi Syndrome and Acute Kidney Injury
- Laparoscopic Partial Splenectomy for Giant Hemangioma Misdiagnosed as Splenic Cyst:a Case Report
- Diagnosis and Treatment of Infective Endocarditis in Chronic Hemodialysis Patients△
- The St.George’s Respiratory Questionnaire in Lymphangioleiomyomatosis△
- Effects of Acute Normovolemic Hemodilution on Perioperative Coagulation and Fibrinolysis in Elderly Patients Undergoing Hepatic Carcinectomy△
