子痫前期患者血清miR-20b、miR-4443水平及与不良妊娠结局的关系



[摘"要]目的"检测子痫前期(PE)患者血清微小RNA-20b(miR-20b)、微小RNA-4443(miR-4443)的水平,并探讨二者对PE患者妊娠结局的预测价值。方法"选取2021年2月至2023年1月在本院接受治疗的212名PE患者为研究组,根据病情严重程度分为重度PE组(n=106)和轻度PE组(n=106);另选取同期106例孕检健康的孕妇作为对照组。根据重度PE组患者的妊娠结局分为妊娠结局良好组和妊娠结局不良组。采用实时荧光定量PCR法(qRT-PCR)检测所有受试者血清中miR-20b和miR-4443的表达水平;使用多因素Logistic回归分析患者妊娠结局的影响因素;采用受试者工作特征(ROC)曲线评估miR-20b、miR-4443对重度PE孕妇妊娠不良结局的预测价值。结果"对照组、轻度PE组、重度PE组血清miR-20b、miR-4443水平逐渐升高(F值分别为486.199和354.434,P<0.001),胎儿宫内窘迫和早产的发生率在各组之间差异显著(χ2值为10.498和15.163,P<0.001)。重度PE组不良妊娠结局总发生率为48.11%,显著高于轻度PE组及对照组(χ2=50.956,P<0.001)。妊娠结局不良组miR-20b水平及miR-4443水平均显著高于妊娠结局良好组(t=5.750,5.853,P<0.001)。多因素Logistic回归分析表明,miR-20b(OR=3.564,95%CI:1.546~8.214)、miR-4443(OR=2.365,95%CI:1.472~3.800)、收缩压(OR=2.869,95%CI:1.373~5.995)、尿蛋白(OR=3.837,95%CI:1.910~7.709)、甘油三酯(TG)(OR=4.236,95%CI:2.027~8.851)是患者发生不良妊娠结局的危险因素(P<0.05)。ROC曲线分析结果显示,miR-20b、miR-4443联合预测重度PE妊娠结局的曲线下面积(AUC)为0.945(95%CI:0.901~0.989),显著高于miR-20b及miR-4443单独预测(Z值分别为2.412和2.055,P<0.05)。结论"重度PE患者血清miR-20b、miR-4443呈高表达,与不良妊娠结局的发生风险有关,二者联合使用可作为重度PE患者不良妊娠结局的预测指标。
[关键词]子痫前期;微小RNA-20b;微小RNA-4443;妊娠结局;预测
Doi:10.3969/j.issn.1673-5293.2024.10.08
[中图分类号]R714""""[文献标识码]A
[文章编号]1673-5293(2024)10-0043-07
Serum levels of miR-20b and miR-4443 of patients with severe preeclampsia and
their relationships with adverse pregnancy outcomes
LIU Zhiming1,LI Suhang2,QI Guijie1,JIANG Tiancong1
(1.Tangshan Municipal Maternal and Child Health Hospital,Tangshan Key Laboratory of
Birth Defect Screening and Diagnosis,Hebei Tangshan 063000,China;2.The Second Hospital
of Hebei Medical University,Hebei Shijiazhuang 050000,China)
[Abstract] Objective To detect serum levels of microRNA-20b (miR-20b) and microRNA-4443 (miR-4443) of patients with severe preeclampsia,and to explore their predictive values for pregnancy outcomes of the patients. Methods A total of 106 patients with severe preeclampsia who were treated in our hospital from February 2021 to January 2023 were selected as severe preeclampsia group,and 106 patients with mild preeclampsia were selected as mild preeclampsia group,other 106 healthy pregnant women who received regular prenatal examination in the same period were as the control group.Quantitative real-time PCR (qRT-PCR) method was applied to detect expression levels of miR-20b and miR-4443 in serum.According to pregnancy outcome,the patients with preeclampsia were divided into good pregnancy outcome group (n=55) and poor pregnancy outcome group (n=51).Multivariate Logistic regression was applied to analyze influencing factors of pregnancy outcomes of the patients with severe preeclampsia.Receiver operating characteristic (ROC) curve was applied to evaluate values of miR-20b and miR-4443 in predicting adverse pregnancy outcomes of the patients with severe preeclampsia. Results The serum levels of miR-20b and miR-4443 of the pregnant women in the control group,mild preeclampsia group and severe preeclampsia group gradually increased (F=486.199 and 354.434 respectively,both Plt;0.001).There were significant differences in incidences of fetal intrauterine distress and preterm delivery (χ2=10.498 and 15.163 respectively,both Plt;0.001).The total incidence of adverse pregnancy outcomes in the severe preeclampsia group was 48.11%,which was significantly higher than those in the mild preeclampsia group and the control group (χ2=50.956,Plt;0.001).The serum levels of miR-20b and miR-4443 of the pregnant women in the poor pregnancy outcome group were significantly higher than those in the good pregnancy outcome group (t=5.750 and 5.853 respectively,both Plt;0.001).Multivariate Logistic regression analysis showed that miR-20b (OR=3.564,95% CI:1.546-8.214),miR-4443 (OR=2.365,95% CI:1.472-3.800),systolic blood pressure (OR=2.869,95% CI:1.373-5.995),urinary protein (OR=3.837,95%CI:1.910-7.709) and triglycerides (TG) (OR=4.236,95%CI:2.027-8.851) were all risk factors for adverse pregnancy outcomes of the patients with severe preeclampsia (all Plt;0.05).ROC curve analysis showed that area under the curve (AUC) of combination detection of serum miR-20b and miR-4443 levels for predicting pregnancy outcome of the patients with severe preeclampsia was 0.945 (95% CI:0.901-0.989),which was significantly higher than those predicted by single detection of miR-20b (Z=2.412,Plt;0.05) and miR-4443 alone (Z=2.055,Plt;0.05). Conclusion The miR-20b and miR-4443 of the patients with severe preeclampsia are highly expressed in serum,which is related to risk of adverse pregnancy outcomes.The combination detection of serum miR-20b and miR-4443 levels can be considered as a predictive index for adverse pregnancy outcomes of the patients with severe preeclampsia.
[Key words] severe preeclampsia;micro RNA-20b;micro RNA-4443;pregnancy outcome;prediction
子痫前期(preeclampsia,PE)是孕妇及胎儿死亡的主要原因,影响了全球5%~8%的孕妇,对孕妇和胎儿造成严重的生命威胁[1-3]。当发生重度PE时,胎儿会受到不同程度的损伤,因此,需要有效的生物标志物和治疗策略,改善患者妊娠结局。研究发现微小RNA(microRNA,miRNAs)在重度PE患者中显著增加[4],且对PE患者妊娠结局的评估具有重要作用[5]。微小RNA-20b(microRNA-20b,miR-20b)与胎盘滋养层细胞的增殖、侵袭和迁移有关,可通过靶向髓系白血病-1抑制胎盘滋养层细胞的增殖、侵袭和迁移促进PE的发生[6]。微小RNA-4443(microRNA-4443,miR-4443)在人类疾病中异常表达[7]。Chen等[8]研究发现,miR-4443可通过靶向基质金属蛋白酶2(matrix metallopeptidase 2,MMP2)抑制滋养层的侵袭和迁移,miR-4443水平上调可能进一步影响肝素结合性表皮生长因子(heparin-binding epidermal growth factor-like growth factor,HB-EGF)或表皮生长因子受体(epidermal growth factor receptor,EGFR)信号,并对PE的发生产生影响。miR-20b、miR-4443均可通过靶向MMP2在PE中起作用。本研究将血清miR-20b、miR-4443作为联合观察指标,探讨PE患者血清miR-20b、miR-4443水平及临床意义。
1资料与方法
1.1一般资料
选取2021年2月至2023年1月在本院接受治疗的212名PE患者为研究组,根据病情严重程度分为重度PE组(n=106)和轻度PE组(n=106);另选取同期106例孕检健康的孕妇作为对照组。纳入标准:①符合PE相关诊断标准[9];②单胎妊娠;③临床资料完整。排除标准:①除PE外,合并妊娠糖尿病等其它妊娠期并发症;②孕前有高血压史;③有早产、自然流产等不良妊娠史;④合并自身免疫疾病、中枢神经系统疾病。本研究经医院伦理委员会批准(批号:2023-N01115),所有研究对象均知情同意且自愿参与研究。
1.2方法
1.2.1血液样本采集
采集重度PE组、轻度PE组患者入组次日(对照组为孕妇产检当日)空腹静脉血5mL,静置30min,4℃离心机中3 000r/min离心10min,分离出血清,-80℃条件下保存备用。
1.2.2检测血清中miR-20b和miR-4443的表达水平
采用Trizol试剂盒由爱必信(上海)生物科技有限公司提供,提取各组样品中总RNA,并使用Takara反转录试剂盒由博爱派克生物科技提供,反转录成cDNA。以cDNA为模板,采用实时荧光定量PCR(quantitative real-time PCR,qRT-PCR)检测样本中miR-20b、miR-4443的表达水平(PCR反应体系:2×Taq PCR master mix 7.5μL、cDNA模板2μL、正、反向引物各1μL、ddH2O补齐至20μL),反应条件:95℃预变性10min,1个循环;扩增38个循环:95℃变性15s,60℃退火、延伸30s。miR-20b、miR-4443引物及U6内参引物由贝塞尔特(北京)生物技术有限公司提供,引物序列见表1。实验重复3次。使用2-ΔΔCt方法计算miR-182-5p、miR-372-3p的相对表达水平。
1.2.3不良妊娠结局定义及分组
若出现胎儿早产、宫内窘迫、死亡、窒息,产妇出现羊水过少、产后出血等,则判定为不良妊娠结局。根据随访记录(妊娠结局情况),将重度PE患者分为妊娠结局不良组(n=51例)和妊娠结局良好组(n=55例)。
1.3统计学分析
SPSS 25.0用于分析数据。符合正态分布的计量资料采用均数±标准差(x-±s)表示,两组间比较采用独立样本t检验,三组间比较采用单因素方差分析;计数资料采用例数(百分比)[n(%)]表示,比较采用χ2检验。采用多因素Logistic回归分析PE患者不良妊娠结局的影响因素;采用受试者工作特征(receiver operating characteristic,ROC)曲线评价miR-20b、miR-4443对PE患者妊娠结局的预测价值,P<0.05为差异有统计学意义。
2结果
2.1三组孕妇一般资料比较
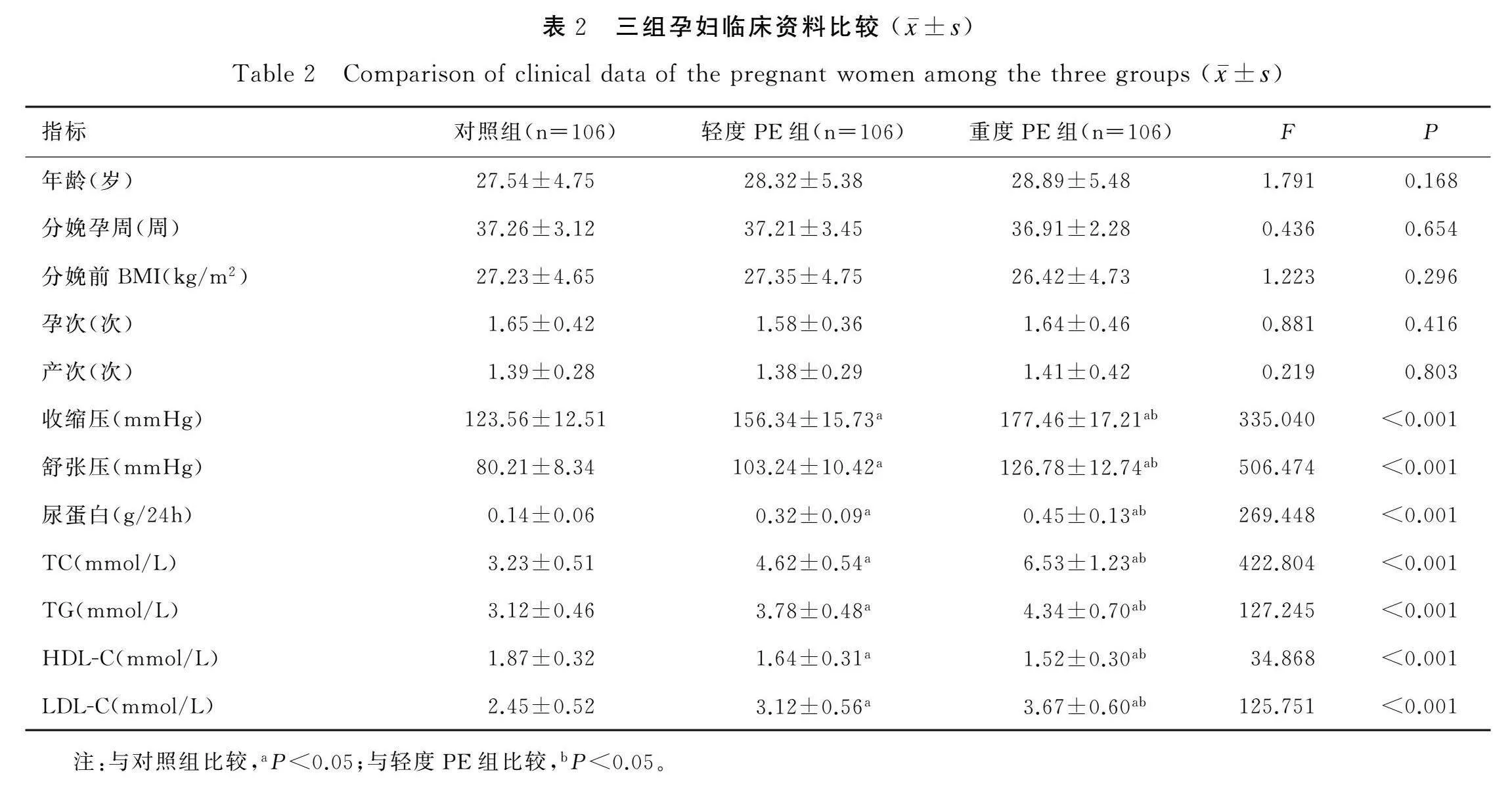
三组孕妇年龄、分娩孕周、分娩前体质量指数(body mass index,BMI)、孕次、产次比较均无统计学差异(P>0.05);对照组、轻度PE组、重度PE组孕妇收缩压、舒张压、尿蛋白、总胆固醇(total cholesterol,TC)、甘油三酯(triacylglycerol,TG)、低密度脂蛋白胆固醇(low density lipoprotein cholesterol,LDL-C)水平逐渐升高(F值介于125.751~506.474,P<0.001),而高密度脂蛋白胆固醇(high density lipoprotein cholesterol,HDL-C)逐渐降低(F值为34.868,P<0.001)。见表2。
2.2三组孕妇血清miR-20b、miR-4443水平比较
对照组、轻度PE组、重度PE组孕妇血清miR-20b、miR-4443水平逐渐增加(F值分别为486.199和354.434,P<0.001)。见表3。
2.3三组孕妇不良妊娠结局比较
对照组、轻度PE组、重度PE组孕妇不良妊娠结局中的低体重儿、羊水过少、胎儿死亡、新生儿窒息、产后出血间比较差异无统计学意义(P>0.05),而胎儿宫内窘迫、早产间比较差异显著(χ2值为10.498和15.163,P<0.01)。重度PE组患者不良妊娠结局总发生率为48.11%,显著高于轻度PE组及对照组(χ2=50.956,P<0.001)。见表4。
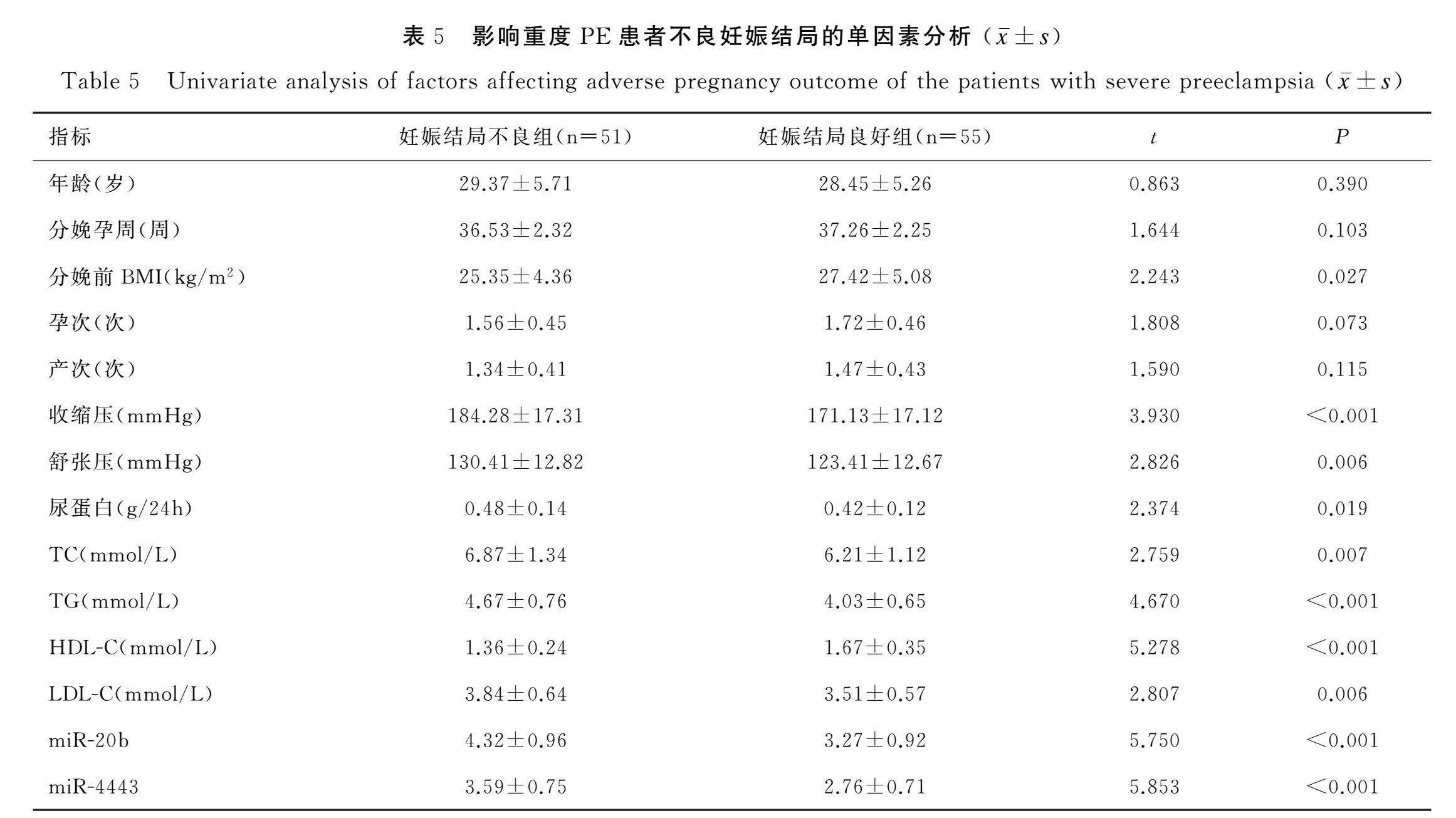
2.4影响重度PE患者妊娠结局的单因素分析
妊娠结局不良组和妊娠结局良好组两组患者年龄、分娩孕周、孕次、产次比较差异不显著(P>0.05);妊娠结局不良组患者收缩压、舒张压、尿蛋白、TC、TG、LDL-C、miR-20b水平及miR-4443水平均显著高于妊娠结局良好组(t值介于2.374~5.750,P<0.05),分娩前BMI、HDL-C低于妊娠结局良好组(t值为2.243和5.278,P<0.05)。见表5。
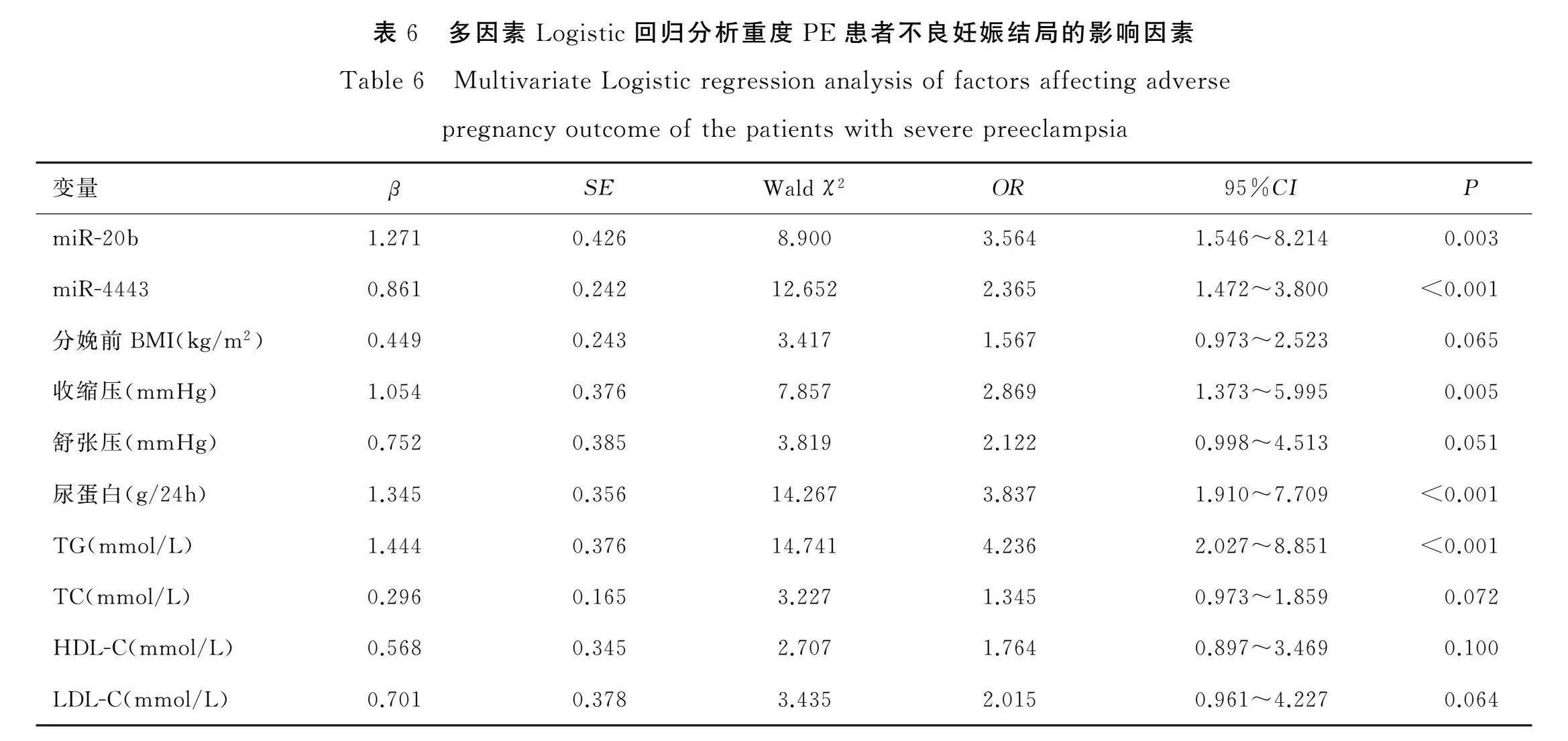
2.5影响重度PE患者妊娠结局的多因素Logistic回归分析
以重度PE患者的妊娠结局作为因变量(妊娠结局良好=0,妊娠结局不良=1),将表5有统计学意义的指标:miR-20b、miR-4443、分娩前BMI、收缩压、舒张压、尿蛋白、TC、TG、HDL-C及LDL-C作为自变量,自变量均为连续变量,带入实测值。经多因素Logistic回归分析表明,miR-20b(OR=3.564,95%CI:1.546~8.214)、miR-4443(OR=2.365,95%CI:1.472~3.800)、收缩压(OR=2.869,95%CI:1.373~5.995)、尿蛋白(OR=3.837,95%CI:1.910~7.709)、TG(OR=4.236,95%CI:2.027~8.851)是患者发生不良妊娠结局的危险因素(P均<0.05)。见表6。
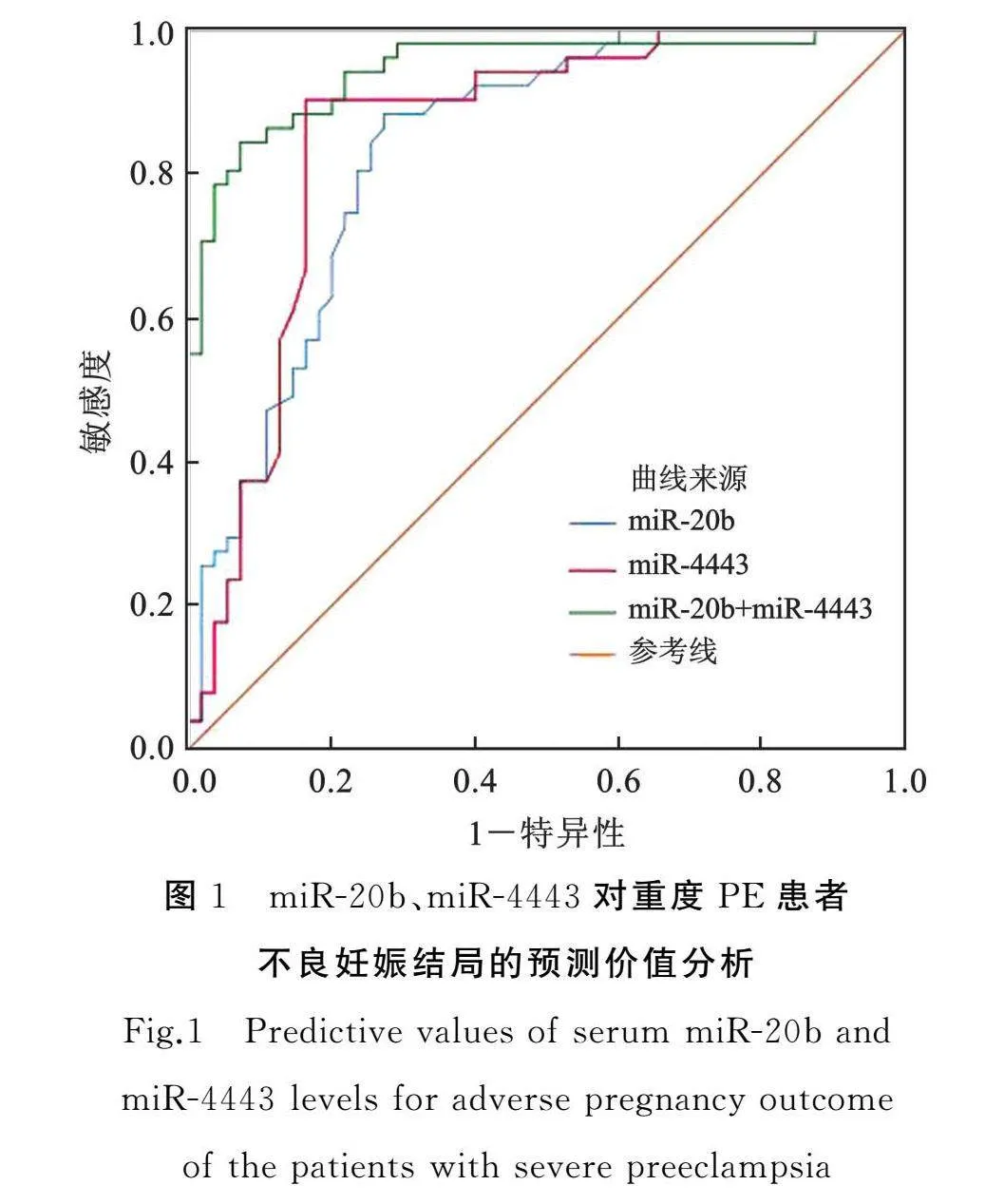
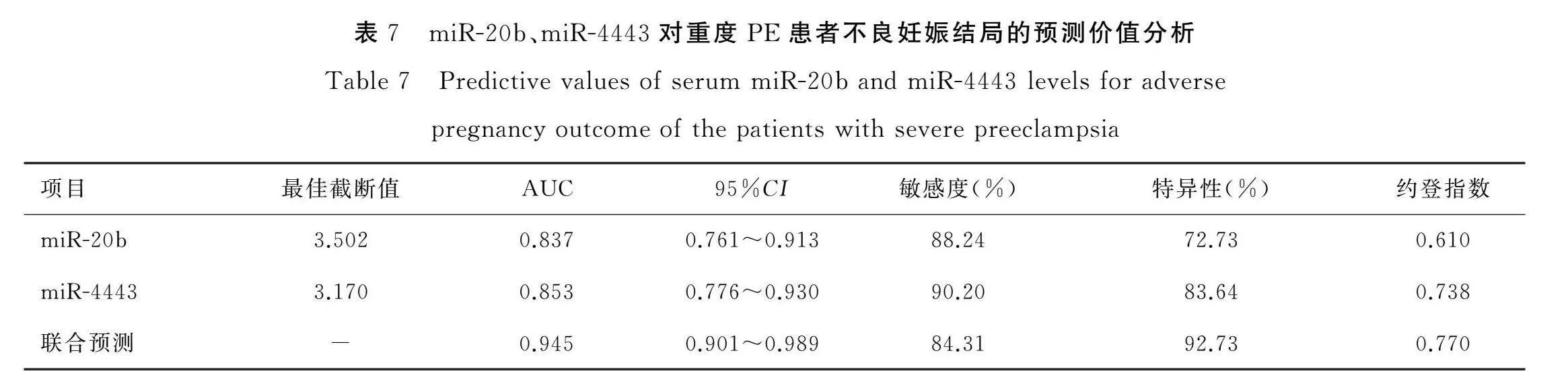
2.6 miR-20b、miR-4443对重度PE患者发生不良妊娠结局的预测价值
将重度PE患者的血清miR-20b、miR-4443水平做检验变量,妊娠结局情况作为因变量(0=良好,1=不良),绘制ROC曲线图,结果显示miR-20b、miR-4443联合预测重度PE妊娠结局的曲线下面积(area under the curve,AUC)为0.945(95%CI:0.901~0.989),显著高于miR-20b单独预测(Z=2.412,P=0.016)及miR-4443单独预测(Z=2.055,P=0.040)。见表7和图1。
3讨论
PE与胎盘灌注不足有关,主要因滋养层细胞凋亡所致[10-11]。重度PE患者病情更严重,可能引发胎儿早产、低体重儿、胎儿死亡、新生儿窒息等不良妊娠结局[12-13],沈敦隽等[14]研究表明重度PE患者不良妊娠结局发生率达到53.84%,严重影响母婴的健康。因此,探讨与PE患者妊娠结局有关的指标,对早期干预、预防不良妊娠结局的发生有重要作用。
3.1 PE患者血清miR-20b和miR-4443水平表达情况
研究发现,滋养层侵袭不足与PE的发展有关[15-16]。Cao等研究[17]发现miR-20a-5p与妊娠并发症的发生有关。Zhang等[6]研究表明,miR-20b在PE患者的胎盘组织中高表达,可通过靶向髓系白血病-1抑制胎盘滋养层细胞的增殖、侵袭和迁移,促进PE的发生。Wang等[18]的研究表明miR-20b在PE胎盘中表达明显上调,提示miR-20b可能参与PE的病理过程。本研究中,对照组、轻度PE组、重度PE组孕妇血清miR-20b水平逐渐增加,表明miR-20b高表达可能与重度PE的发生发展有关,在一定程度上可反应疾病程度。miR-4443在PE中可能具有致病作用,Chen等[9]研究发现,miR-4443在重度PE患者胎盘组织中表达上调。本研究中,对照组、轻度PE组、重度PE组孕妇血清miR-4443水平逐渐增加,提示miR-4443高水平与患者疾病程度有关,参与PE的进展,与既往研究[9]中在胎盘组织中表达趋势一致。
3.2 PE患者血清miR-20b和miR-4443水平与不良妊娠结局的关系
本研究显示不同PE严重程度患者的不良妊娠结局发生率差异有统计学意义,与沈敦隽等[14]研究的不良妊娠结局发生率相近。近一步分析发现,妊娠结局不良组PE患者的收缩压、舒张压、尿蛋白、TC、TG、LDL-C水平均显著高于妊娠结局良好组,分娩前BMI、HDL-C低于妊娠结局良好组,表明血脂异常增加了不良妊娠结局的发生[19-20]。妊娠结局不良组PE患者的miR-20b及miR-4443水平均显著高于妊娠结局良好组,进一步多因素Logistic回归分析显示,miR-20b、miR-4443、收缩压、尿蛋白、TG是重度PE患者发生不良妊娠结局的危险因素,进一步证实了miR-20b、miR-4443与PE患者不良妊娠结局有关。且本研究发现miR-20b、miR-4443联合预测重度PE患者不良妊娠结局的AUC高于二者单独预测的AUC,且特异性更高,二者联合预测重度PE患者妊娠结局的效能提高。临床可根据两指标水平情况,快速对患者做出判断,及时治疗,改善预后。当血清miR-20b相对表达水平高于3.502,同时miR-4443相对表达水平高于3.170时,结合患者其他相关指标,可对病情快速做出判断,及时采取措施,有较好的临床参考价值。
综上所述,重度PE患者血清miR-20b、miR-4443水平均显著升高,且二者对患者妊娠结局具有一定的评估价值。但本研究样本量较少,可能会存在统计偏差,后续将继续扩大样本量进一步验证。
[参考文献]
[1]Overton E,Tobes D,Lee A.Preeclampsia diagnosis and management[J].Best Pract Res Clin Anaesthesiol,2022,36(1):107-121.
[2]Alese MO,Moodley J,Naicker T.Preeclampsia and HELLP syndrome,the role of the liver[J].J Matern Fetal Neonatal Med,2021,34(1):117-123.
[3]Hromadnikova I,Kotlabova K,Dvorakova L,et al.Postnatal expression profile of microRNAs associated with cardiovascular and cerebrovascular diseases in children at the age of 3 to 11 years in relation to previous occurrence of pregnancy-related complications[J].Int J Mol Sci,2019,20(3):654-707.
[4]Chen D,He B,Zheng P,et al.Identification of mRNA-,circRNA-"and lncRNA-"associated ceRNA networks and potential biomarkers for preeclampsia from umbilical vein endothelial cells[J].Front Mol Biosci,2021,8(1):652250-652262.
[5]Hromadnikova I,Kotlabova K,Krofta L.First-trimester screening for fetal growth restriction and small-for-gestational-age pregnancies without preeclampsia using cardiovascular disease-associated microRNA biomarkers[J].Biomedicines,2022,10(3):718-733.
[6]Zhang SS,Kan XQ,Liu P,et al.MiR-20b is implicated in preeclampsia progression via the regulation of myeloid cell leukemin-1[J].J Biol Regul Homeost Agents,2020,34(5):1709-1717.
[7]Mao Y,Shen J,Wu Y,et al.Aberrant expression of microRNA-4443(miR-4443)in human diseases[J].Bioengineered,2022,13(6):14770-14779.
[8]Chen C,Gao J,Chen D,et al.miR-4443/MMP2 suppresses the migration and invasion of trophoblasts through the HB-EGF/EGFR pathway in preeclampsia[J].Cell Cycle,2022,21(23):2517-2532.
[9]谢幸,孔北华,段涛,等.妇产科学(第九版)[M].北京:人民卫生出版社,2018:83-90.
[10]胡敏,刘丽,罗玉芳,等.妊娠晚期维生素A、D、E水平与子痫前期及胎儿生长发育的关联分析[J].中国妇幼健康研究,2022,33(8):116-119.
[11]习辉,聂鸿雁,张世凤.子痫前期胎盘组织中SMARCA5基因的表达及其与滋养细胞侵袭、凋亡的相关关系[J].中国性科学,2020,29(5):111-114.
[12]Zhang T,Bian Q,Chen Y,et al.Dissecting human trophoblast cell transcriptional heterogeneity in preeclampsia using single-cell RNA sequencing[J].Mol Genet Genomic Med,2021,9(8):e1730-"e1740.
[13]Turbeville HR,Sasser JM.Preeclampsia beyond pregnancy:long-term consequences for mother and child[J].Am J Physiol Renal Physiol,2020,318(6):F1315-F1326.
[14]沈敦隽,王听,黄晓林.重度子痫前期患者血清FOXA1、TRAF6水平及预测不良妊娠结局价值[J].中国计划生育学杂志,2022,30(11):2604-2610.
[15]Zhou W,Wang H,Yang Y,et al.Trophoblast cell subtypes and dysfunction in the placenta of individuals with preeclampsia revealed by single-cell RNA sequencing[J].Mol Cells,2022,45(5):317-328.
[16]Peng P,Song H,Xie C,et al.miR-146a-5p-mediated suppression on trophoblast cell progression and epithelial-mesenchymal transition in preeclampsia[J].Biol Res,2021,54(1):30-41.
[17]Cao YL,Jia YJ,Xing BH,et al.Plasma microRNA-16-5p,-17-5p and -20a-5p:novel diagnostic biomarkers for gestational diabetes mellitus[J].J Obstet Gynaecol Res,2017,43(6):974-981.
[18]Wang W,Feng L,Zhang H,et al.Preeclampsia up-regulates angiogenesis-associated microRNA (i.e.miR-17,-20a and -20b) that target ephrin-B2 and EPHB4 in human placenta[J].J Clin Endocrinol Metab,2012,97(6):E1051-E1059.
[19]周玲,王莉,张妍,等.孕妇血脂水平与巨大儿的关系[J].中国妇幼健康研究,2018,29(06):697-701.
[20]乔小改,蔡大军,张庆.载脂蛋白B/A1比值对子痫前期患者妊娠结局的预测价值[J].现代妇产科进展,2022,31(8):597-600,604.
[专业责任编辑:李春芳]
[中文编辑:牛"惠;英文编辑:杨周岐]