Racial, ethnic, and socioeconomic differences in hepatocellular carcinoma across the United States
Adrian Diaz, Samantha M.Ruff, Timothy M.Pawlik
Department of Surgery, Division of Surgical Oncology, The Ohio State University Wexner Medical Center and James Comprehensive Cancer Center, Columbus, OH 43210, USA.
Abstract Hepatocellular carcinoma (HCC) poses a significant public health challenge within the US, exerting an increasingly substantial influence on cancer-related deaths.However, the HCC burden is not uniformly distributed, with significant disparities related to race, ethnicity, and socioeconomic status.This manuscript comprehensively reviews the multifaceted origins of HCC disparities, exploring their roots in the sociocultural environment,socioeconomics, the physical/built environment, and the healthcare/political systems.The sociocultural environment highlights the unique challenges faced by racial and ethnic minority populations, including language barriers, cultural beliefs, and limited healthcare access.The socioeconomics and the physical/built environment section emphasize the impact of neighborhood poverty, geographic disparities, and healthcare infrastructure on HCC outcomes.The healthcare and political systems play a pivotal role in driving HCC disparities through practice guidelines, healthcare policies, insurance coverage, and access to care.Inconsistent practice guidelines across specialties and variations in insurance coverage contribute to disparities in HCC surveillance and treatment.In conclusion, addressing HCC disparities requires a multifaceted, patient-centered approach that includes cultural competence, infrastructure enhancements, policy changes, and improved access to care.Collaborative efforts among healthcare professionals, researchers, policymakers, and institutions are essential to reducing the burden of HCC on marginalized communities and ensuring equitable care for all individuals affected by this complex disease.
Keywords: Liver, cancer, hepatocellular, race, socioeconomic, United States
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common primary liver cancer and the fastest-growing cause of cancer-related death in the United States (US)[1].Nonetheless, HCC is not experienced equally among patients in the US.Race/ethnicity and socioeconomic disparities related to HCC pervade the entire spectrum of care, ranging from screening and early detection of cirrhosis all the way to HCC-related mortality[2].These disparities have multifactorial origins and are intricately intertwined between the patient and societal factors.Drivers of healthcare disparities encompass downstream social determinants of health,encompassing health literacy, health insurance, and neighborhood characteristics, among many others[3-5].Additionally, factors such as discriminatory policies and systemic racism[6-9]overwhelmingly impact racial and ethnic minorities[10,11].
Evaluation of HCC disparities relative to race/ethnicity and social determinants of health provides an opportunity for healthcare providers and policymakers to identify interventions and policies that can address inequities in HCC care.In this review, we systematically summarize racial/ethnic and socioeconomic variations in HCC care across three domains: (1) the sociocultural environment; (2) the physical/built environment; and (3) the healthcare system [Figure 1][12].Sociocultural factors, such as cultural beliefs and social support, impact healthcare-seeking behaviors.The physical and built environment, including geographic disparities and healthcare infrastructure, plays a pivotal role in HCC outcomes.The healthcare system itself, including healthcare provider biases and insurance coverage,contributes to these disparities.As we delineate in this review, these disparities encompass an extensive array of determinants, spanning from individual and behavioral factors to deeply entrenched systemic issues.Only through a multifaceted, interdisciplinary approach can more equitable outcomes for all patients with HCC be achieved and the burden of this fatal disease on marginalized communities be better alleviated.
In the pursuit of equitable outcomes for all patients facing the challenges of hepatocellular carcinoma(HCC), it is essential that we recognize the need for continued research, policy reform, and collective action.As we embark on this journey to address disparities in HCC care, it is vital that we remain committed to not only identifying these disparities but also implementing evidence-based solutions.In doing so, we have the potential to not only improve the care and outcomes for individuals impacted by HCC but also to reduce the broader health disparities that affect marginalized communities.By fostering a collaborative environment among healthcare providers, researchers, policymakers, and affected communities, we can work towards a future where access to high-quality HCC care is a reality for all, regardless of race/ethnicity,socioeconomic status, or geographic location.This collective effort holds the promise of not only reducing the burden of HCC but also advancing the broader mission of health equity in the United States and beyond.Our goal is that this review serves as a guidepost towards more equitable care and outcomes for all patients with HCC.
SOCIOCULTURAL
Racial and ethnic disparities in HCC care have been consistently observed, with minority populations facing unique challenges.Barriers related to language, cultural beliefs, and healthcare access are common.Moreover, healthcare disparities intersect with socioeconomic status, often disproportionately affecting minority communities.For example, racial and ethnic minorities are more likely to experience poverty, lack of health insurance, and limited access to quality healthcare services[13].The cumulative impact of these sociocultural determinants can lead to delayed HCC diagnosis, advanced disease stage at presentation, and suboptimal treatment options, contributing to disparities in HCC outcomes.
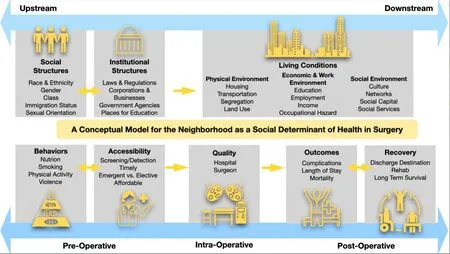
Figure 1.Conceptual model for social determinates of health and delivery of healthcare.
Assessing HCC disparities associated with race and ethnicity is a complex endeavor.Because race is a social construct that is frequently self-reported and subject to under- or misreporting, they fail to fully encapsulate the rich cultural diversity within and across racial and ethnic groups.Disparities linked to race and ethnicity are deeply entrenched in historical, cultural, and socioeconomic factors, influencing every facet of the HCC care continuum.Consequently, understanding and addressing these disparities necessitates a comprehensive perspective that considers the sociocultural context within which they manifest.Recognizing that these disparities are rooted in multifaceted factors is the first step towards equitable healthcare.
Data from the US Surveillance, Epidemiology, and End Results (SEER) program demonstrates significant disparities in HCC incidence across racial and ethnic groups.The highest incidence of HCC is among American Indians and Alaska Natives (AI/AN) at 15.7 per 100,000 persons, followed by Hispanics at 13.5,Asian Americans or Asian and Pacific Islanders (API) at 12.6, Black individuals at 11.0, and White individuals at 7.1[14].Notably, the Hispanic population experienced a remarkable 35.8% increase in HCC incidence from 2003 to 2011, foreshadowing the likelihood that Hispanic and Black individuals will have the highest HCC incidence rates by 2030[15].These statistics underscore the urgency of addressing the unique challenges faced by these populations in HCC care and prevention.
The causes of liver cirrhosis and the related risk of HCC vary among distinct racial and ethnic populations.Understanding these variations and the factors underlying them is critical to exploring and eventually mitigating their effects.Chronic liver diseases, such as NAFLD or HBV, are more prevalent among minority groups, resulting in a higher incidence of HCC[16,17].For instance, Alaska Native people experience a high prevalence of HBV, HCV, and autoimmune hepatitis, leading to elevated HCC rates[18-20].Similarly, Black individuals have a higher prevalence of HCV infection, a significant risk factor for HCC in cirrhotic patients[21,22].Despite progress in awareness of the downstream consequences of HBV, vaccination efforts,and treatment, Asian American individuals continue to endure a significant burden of HBV-related HCC[23].This is largely attributed to a significant number of individuals who have immigrated from countries with high HBV prevalence and elevated rates of vertical transmission[24].
HCC surveillance, which involves regular imaging and laboratory tests, is recommended every six months for individuals with chronic HBV infection or cirrhosis[25].Despite these guidelines, surveillance rates often fall short of optimal standards, and disparities are evident across different racial and ethnic groups[26].For example, data from SEER-Medicare claims revealed that 49% of Hispanic and 59% of Black patients did not receive any HCC screening within the three years prior to their HCC diagnosis[27].Additionally, other studies have shown that Black and Hispanic patients are 60% less likely to undergo HCC screening compared to White patients[28].Moreover, these disparities extend to referral rates to specialty clinics,especially for Black and Hispanic patients.Factors influencing these disparities include patient-provider interactions affected by implicit racial/ethnic biases[29], limited clinical time for screening[30], and varying perceptions of the importance of screening[31].
The stage at which HCC is diagnosed is closely related to the HCC treatment a patient has access to.Even when patients present with similar disease stages, racial and ethnic minorities do not receive equitable HCC treatment.For instance, Black and Hispanic patients are the least likely to undergo any HCC treatment and are less likely to receive curative-intent interventions such as hepatic resection or ablation[32-36].In contrast,Asian American patients are more likely to undergo resection and receive curative-intent therapy for earlystage HCC[35,37].This discrepancy can be partly explained by the higher prevalence of HBV-related HCC in the Asian American community, including non-cirrhotic cases[38].Since routine HCC surveillance is recommended for patients with chronic HBV, regardless of cirrhosis status, Asian American patients have been demonstrated to have a greater likelihood of early-stage HCC diagnoses amenable to curative treatments[25].Addressing these disparities is essential to ensure that all HCC patients receive appropriate and timely care, regardless of their racial or ethnic background, and to strive for a more equitable healthcare system.
Further, the medical treatment of HCC is quickly evolving.Specifically, the landscape of new agents and combinations continues to expand.For example, immune-based combinations have been associated with improved results among patients with advanced HCC, as reported in several recent landmark trials[39-41].Based on the promising results of early-phase clinical trials, lenvatinib plus pembrolizumab has the potential to represent a novel treatment option in the advanced HCC setting.Differences in access to or efficacy of these novel medical therapies in different patient populations need to be examined.As such, diversity in clinical trials is paramount and of the utmost importance to elucidate how novel therapies perform in different patient populations.
SOCIOECONOMICS AND PHYSICAL/BUILT ENVIRONMENT
Disparities can also be attributed to differences in the continuum of care for HCC across socioeconomic levels, as well as by physical and built environment factors.Differences observed in healthcare delivery and outcomes are largely impacted by the intersection of race/ethnicity and socioeconomic status, often disproportionately affecting minority communities.While attempts to disaggregate that intersection to focus on the socioeconomic and the physical/built environment are important, racial and ethnic minorities are routinely more likely to experience poverty, lack of health insurance, and limited access to quality healthcare services[13].The cumulative impact of these determinants often leads to delayed HCC diagnosis,advanced disease stage at presentation, and suboptimal treatment options, contributing to disparities in HCC outcomes.
Individual-level outcomes among patients with HCC are impacted by several societal level factors, such as median neighborhood income, rural versus urban residence, and patients’ proximity to certain healthcare facilities.Among AI/AN patients, the incidence of HCC varies significancy based on their geographic location[42].Despite these variations, the underlying reasons for these disparities have not been elucidated.Therefore, researchers and policy makers alike have begun to advocate for the collection of individual-level and community-level characteristics to help identify and mitigate the underlying mechanisms behind healthcare disparities.Additionally, assessing the impact of socioeconomic factors and examining how clinical cofactors such as NAFLD and alcohol use interact among different groups may provide insights into the variations in HCC incidence.This information can guide the development and implementation of interventions aimed at addressing these aforementioned factors along the HCC care pathway[43].The goal is ultimately improving the effectiveness and sustainability of policies focused on achieving health equity.
As delineated in the previous sections, there are notable disparities in the diagnosis and staging of Hepatocellular Carcinoma (HCC) based on racial and ethnic backgrounds[33,37,44,45].Studies have revealed that compared to their White counterparts, Hispanic and Black patients are at a 20% and 18% higher risk of being diagnosed with advanced-stage HCC[15,46].These disparities in HCC outcomes are often influenced by various factors in the built environment, encompassing both neighborhood- and county-level attributes.Further, numerous built environment factors, including neighborhood and county-level characteristics, may contribute to these disparities.For instance, individuals residing in rural areas have an increased likelihood of presenting with late-stage HCC, missing out on HCC treatment, and succumbing to the disease, as opposed to those in urban areas[47].Additionally, a significant percentage of Black and Hispanic patients reside in counties with elevated social vulnerability indices, which results in a higher probability of encountering more advanced tumors and therefore receiving nonsurgical or non-curative intent interventions for HCC[48].Moreover, it has been observed that individuals of API and Hispanic backgrounds are at a greater risk of developing HCC when living in neighborhoods characterized by low socioeconomic status (SES)[32].These findings emphasize the critical importance of gathering comprehensive data on both individual and neighborhood-level social determinants of health.This holistic approach is necessary to effectively address and mitigate disparities in HCC care that stem from differences in the built environment differences, ensuring equitable healthcare outcomes for all.Finally, it is imperative to establish a healthcare system that not only recognizes these disparities but also proactively addresses them.By prioritizing data collection and interventions focused on both individual and community-level factors, healthcare providers and policymakers can work towards reducing the impact of social determinants on HCC outcomes and,ultimately, improving the health and well-being of affected populations.Achieving equity in HCC care requires a multifaceted approach that acknowledges the intricate interplay between geographic and built environment factors and their influence on health disparities.
In terms of geographic disparities and healthcare infrastructure, access to healthcare services, transportation options, and the availability of specialized liver care centers all influence the timely diagnosis and treatment of HCC.For example, significant travel burdens can exist for patients from lower SES communities; in turn,regionalization of complex cancer surgery may be associated with a significant travel burden for a large subset of patients with complex cancer from certain communities[49-52].Furthermore, healthcare infrastructure, including the presence of comprehensive liver centers and advanced diagnostic tools, varies widely across geographic regions.Disparities in the availability of these resources can impact the quality of care delivered to HCC patients.For example, patients residing in communities with high social vulnerability were less likely to undergo high-risk cancer surgery at a high-volume hospital[53].
SES can also impact HCC-related outcomes including treatment complications, and mortality[48,54-57].Patients with lower SES experience higher HCC mortality irrespective of race and ethnicity.Notably, black patients with low SES have the highest 5-year HCC mortality (11.5%)[58].Hyeret al.noted that social vulnerability was associated with lower attainment of textbook outcomes and an increased risk of adverse postoperative surgical outcomes after several common oncologic procedures, including surgery for HCC[Figure 2][57].Textbook outcomes are defined as no postoperative surgical complications, no prolonged length of hospital stay, no readmission ≤ 90 days after discharge, and no postoperative mortality ≤ 90 days after surgery.Such data suggest that difficult-to-measure factors including social stigma and cultural identity play important roles in the pathway of HCC-related survival.Further research is required to investigate the interplay of these factors, including the potential influence of additional confounders such as health literacy, educational attainment, and their effect more comprehensively on HCC outcomes.
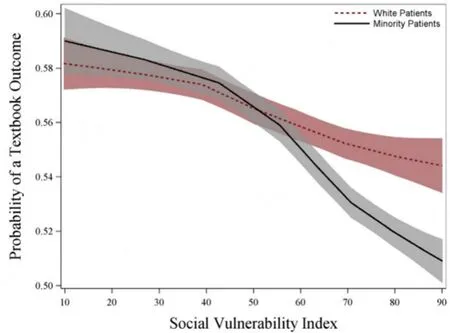
Figure 2.Probability of textbook outcomes in cancer operations.Locally estimated scatterplot smoothing curve demonstrating the association between Social Vulnerability Index and the adjusted probability of achieving textbook outcomes stratified by racial minority status derived from mixed-effect logistic regression.
Overall, individual HCC outcomes are often influenced by factors like neighborhood poverty, rural residence, and proximity to healthcare facilities, with the physical environment and healthcare infrastructure playing a crucial role in driving disparities.Access to healthcare services, transportation, and specialized liver care centers affects timely diagnosis and treatment.Geographic variation in healthcare infrastructure exists, impacting the quality of care.Initiatives to reduce disparities may involve telemedicine,mobile health units, and outreach to underserved regions, ensuring equitable care access.Additionally,addressing socioeconomic factors like poverty is essential.Implementing community-based programs that provide financial assistance, job training, and access to affordable housing can help mitigate the impact of poverty on HCC outcomes.
THE HEALTHCARE AND POLITICAL SYSTEMS
The political and healthcare systems play a pivotal role in driving HCC disparities, particularly through practice guidelines, healthcare policies, insurance coverage, and access to care.For example, the existence of clear practice guidelines is pivotal in the decision-making process concerning HCC surveillance for patients[31].These guidelines significantly influence whether patients receive HCC surveillance.However,there is currently a lack of consistency in guidelines across different medical specialties and professional associations.For example, the American Association for the Study of Liver Diseases recommends HCC surveillance every 6 months for at-risk individuals[25].In contrast, the US Preventive Services Task Force(USPSTF), which helps guide cancer screening practices for primary care clinicians, has not provided guidance on HCC surveillance.Because racial and ethnic minorities are more likely to receive care in primary care settings, HCC screening is often less frequent[59].One major step in addressing variations in HCC care would be advocating consistent practice guidelines across all majors.
Fostering equity in HCC surveillance requires a steadfast commitment to multidisciplinary research.This research is essential in shaping evidence-based practice guidelines.An illustrative instance lies in the realm of NAFLD, which has emerged as a leading cause of cirrhosis[16,17].Issues such as whether to screen solely patients with cirrhosis or encompass those with advanced fibrosis and cirrhosis, as well as the complexities associated with HCC detection through ultrasound, especially in the context of obesity, necessitate immediate investigation and resolution[60].Addressing the underrepresentation of minority patients in clinical trials is paramount.These trials offer potential life-saving interventions for HCC, and prioritizing their inclusion is vital for promoting equitable healthcare outcomes[61,62].
Numerous studies have unveiled the profound influence of an individual's insurance status on the landscape of HCC care [Figure 3][63-69].A striking example is the disparity in insurance coverage between minority patients and their White counterparts.The data has demonstrated that compared to White patients,minority patients are more likely to be uninsured or covered by Medicaid[70,71].To be precise, 9.6% and 45.3% of Black, 17.7% and 37.7% of Hispanic, and 5.8% and 28.2% of Asian patients were uninsured or recipients of public insurance, in contrast to 5.7% and 35.7% of White Americans, respectively[72].This discrepancy in insurance status translates into dire consequences, as uninsured and Medicaid-covered patients with HCC face up to an 88% and 43% higher risk of mortality, compared to those with Medicare or private insurance[62,67].Additionally, lacking insurance has been associated with reduced survival rates among HCC patients[65].These revelations underscore the critical importance of enhancing individual access to health insurance as a pivotal strategy for ameliorating HCC-related mortality and fostering health equity.
Policies affecting access to health insurance can also influence health outcomes for patients with HCC.Medicaid expansion, for instance, has been linked to increased access to insurance coverage among HCC patients, particularly among low-income and minority populations[68,73,74].In the US Veterans Affairs healthcare system, disparities by race/ethnicity have been demonstrated to be less prevalent.For example,one particular study demonstrated that within the VA, Black and Hispanic patients are more likely to receive HCC screening compared to White patients[75].Because insurance coverage and access to healthcare are less variable across the VA system, these findings highlight potentially modifiable factors that currently contribute to disparities in HCC-related outcomes outside of the VA system.Further research is needed to examine the mechanisms through which insurance coverage may impact equitable receipt of surveillance and access to treatment for HCC.Additionally, the effects of broader policy changes on insurance coverage should be examined to gain a better understanding of government-level changes that could improve outcomes for patients with HCC.Overall, the evidence is clear that health insurance plays a central role in determining access to HCC care, and policies should be examined to ensure they do not perpetuate disparities.
CONCLUSION
In conclusion, this review has shed light on the intricate web of disparities in HCC care in the US [Table 1].As described, HCC is experienced unequally among patients, with race/ethnicity and socioeconomic factors deeply intertwined in the web of disparities.The multifactorial origins of these disparities, encompassing social determinants of health, discriminatory policies, systemic racism, and healthcare access, have been systematically dissected across three domains: the sociocultural environment, the physical/built environment, and the healthcare and political systems.To address these disparities effectively, a multifaceted, interdisciplinary approach is essential, bridging individual and systemic issues and fostering equitable outcomes for all HCC patients.

Table 1.Summary of key takeaways
One of the key takeaways from this review is the urgency to identify interventions and policies that can mitigate these disparities and promote equitable access to high-quality HCC care for all patients,irrespective of their racial, ethnic, or socioeconomic backgrounds [Table 2].Collaborative efforts between healthcare providers, researchers, policymakers, and affected communities are imperative to break down the barriers that have contributed to the persistent inequalities in HCC care.By recognizing and proactively addressing the multifaceted factors at play, we can work towards a healthcare system that better serves marginalized communities and reduces the burden of this devastating disease.
Efforts to standardize practice guidelines, invest in research, and promote diversity in clinical trials are pivotal steps towards achieving health equity in HCC care.Addressing the critical influence of health insurance status and the impact of health policies, such as Medicaid expansion, is essential to ensuring that individuals have equitable access to HCC care and that disparities do not persist due to variations in coverage.As we move forward, it is crucial to remain committed to addressing these disparities through evidence-based strategies and policies, with the ultimate goal of ensuring that every patient facing HCC receives the appropriate and timely care they deserve.By doing so, we not only alleviate the burden of this fatal disease on marginalized communities but also contribute to the broader mission of health equity in theUnited States and beyond.

Table 2.Top priorities for health workers, stakeholders, and policymakers

Figure 3.Quarterly trends in case mix before and after Medicaid Expansion.
DECLARATIONS
Authors’ contributions
Made substation contribution to conception, design, acquisition, analysis, and interpretation, drafting of initial manuscript, critical review of final manuscript: Diaz A, Pawlik TM
Made substation contribution to conception, design, and drafting of initial manuscript, critical review of final manuscript: Ruff SM
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2024.
- Hepatoma Research的其它文章
- Introduction of the Chinese expert consensus on postoperative adjuvant therapy for hepatocellular carcinoma (2023 Edition)
- Precise staging of advanced HCC promotes higher quality of personalized treatment management:Chinese experts consensus on precision diagnosis and management of advanced hepatocellular carcinoma (2023)
- Crosstalk between cancer cell plasticity and immune microenvironment in cholangiocarcinoma
- Interpretation of Chinese expert consensus on the whole-course management of hepatocellular carcinoma (2023 edition)
- Mutation-based therapies for intrahepatic cholangiocarcinoma: new options on the horizon
- Associations between physical activity and risk of liver cancer: results from a population-based cohort study in Chinese women