Sex and racial disparities in non-alcoholic fatty liver disease-related cardiovascular events: National inpatient sample analysis (2019)
Rupak Desai,Ali Tariq Alvi,Advait Vasavada,Yashwitha Sai Pulakurthi,Bhavin Patel,Adil Sarvar Mohammed,Shreyans Doshi,Ikechukwu Ogbu
Abstract BACKGROUND Non-alcoholic fatty liver disease (NAFLD) increases cardiovascular disease (CVD) risk irrespective of other risk factors.However,large-scale cardiovascular sex and race differences are poorly understood.AIM To investigate the relationship between NAFLD and major cardiovascular and cerebrovascular events (MACCE) in subgroups using a nationally representative United States inpatient sample.METHODS We examined National Inpatient Sample (2019) to identify adult hospitalizations with NAFLD by age,sex,and race using ICD-10-CM codes.Clinical and demographic characteristics,comorbidities,and MACCE-related mortality,acute myocardial infarction (AMI),cardiac arrest,and stroke were compared in NAFLD cohorts by sex and race.Multivariable regression analyses were adjusted for sociodemographic characteristics,hospitalization features,and comorbidities.RESULTS We examined 409130 hospitalizations [median 55 (IQR 43-66) years] with NFALD.NAFLD was more common in females (1.2%),Hispanics (2%),and Native Americans (1.9%) than whites.Females often reported non-elective admissions,Medicare enrolment,the median age of 55 (IQR 42-67),and poor income.Females had higher obesity and uncomplicated diabetes but lower hypertension,hyperlipidemia,and complicated diabetes than males.Hispanics had a median age of 48 (IQR 37-60),were Medicaid enrollees,and had non-elective admissions.Hispanics had greater diabetes and obesity rates than whites but lower hypertension and hyperlipidemia.MACCE,all-cause mortality,AMI,cardiac arrest,and stroke were all greater in elderly individuals (P < 0.001).MACCE,AMI,and cardiac arrest were more common in men (P < 0.001).Native Americans (aOR 1.64) and Asian Pacific Islanders (aOR 1.18) had higher all-cause death risks than whites.CONCLUSION Increasing age and male sex link NAFLD with adverse MACCE outcomes;Native Americans and Asian Pacific Islanders face higher mortality,highlighting a need for tailored interventions and care.
Key Words: Non-alcoholic fatty liver disease;Cardiovascular disease;Major cardiovascular and cerebrovascular events;Sex/gender disparities;Mortality
INTRODUCTION
With the global rise in obesity and metabolic diseases,non-alcoholic fatty liver disease (NAFLD) has become a prevalent condition.It is now widely recognized that NAFLD has numerous extrahepatic consequences[1] including an increased risk of cardiovascular disease (CVD) independent of traditional cardiovascular risk factors[2,3].Understanding NAFLD and its impact on patient outcomes is of utmost importance,given its intricate underlying mechanisms.This is particularly significant because various modifiable behavioral factors play a role in the development and progression of the condition.Therefore,gaining insight into NAFLD and exploring the potential effects of lifestyle interventions can significantly enhance patient outcomes[4].Risk factors for NAFLD are well-established and can be categorized as modifiable,such as smoking,sedentary lifestyle,poor nutrition habits,and physical inactivity,or non-modifiable,including genetic background,fat metabolism,and age[5].The exploration of sex and racial disparities in cardiovascular outcomes related to NAFLD is an area that has received limited attention and remains largely unexplored on a broader scale.The current body of evidence in this regard is lacking,highlighting the need for further research to address these gaps in knowledge[6].Therefore,this study was conducted to investigate the association between NAFLD and major cardiovascular and cerebrovascular events (MACCE) using a nationally representative sample in the United States.
MATERIALS AND METHODS
Source of data
The 2019 National Inpatient Sample (NIS) database of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality was examined.The NIS is the largest all-payer inpatient healthcare dataset accessible to the public in the United States.With an annual average of 7 million unweighted discharges (and about 35 million weighted nationwide discharges),the dataset comprises around 20% of United States hospitalizations across 50 states.For each inpatient admission,the NIS includes one primary diagnosis and up to 24 sary discharge diagnoses.Due to the de-identified nature of NIS data,permission from the IRB is not mandatory.The HCUP website provides additional information regarding the database[7].
Study population
We identified all hospitalizations with NAFLD in the 2019 NIS database using the K76.0 ICD-10-CM code.We included hospitalizations of adults (18 years and older) with a primary or secondary diagnosis of NAFLD.The latter code has been demonstrated to have a positive predictive value of over 91% for identifying NAFLD and has been previously recommended for use by an expert panel consensus statement for identifying NAFLD in administrative health databases or electronic health records,allowing researchers to ensure accurate identification and classification of NAFLD cases[8,9].
Study outcomes
The primary outcome of interest was to identify gender and racial disparities in NAFLD-related MACCE,including allcause mortality,acute myocardial infarction (AMI),cardiac arrest,and stroke.Secondary outcomes included clinical,demographic,and hospital-level characteristics,and comorbidities associated with NAFLD hospitalizations by ethnicity and gender.Last,we evaluated and compared across subgroups of gender and race the median duration of hospital stay (in days) and total hospital charges (in USD) due to NAFLD-related MACCE in NAFLD hospitalizations.
Statistical analyses
The prevalence of NAFLD was calculated per sex and race categories.Using Pearson’s Chi-square test for categorical variables and the Mann WhitneyUtest for continuous variables,we compared the clinical,demographic and hospitallevel characteristics of NAFLD hospitalizations between subgroups of interest: sex and race.Discharge records with missing data for sex or race (< 5% of data) were excluded from analysis.The continuous and categorical variables were expressed as medians and percentages,respectively.To determine statistical significance,a two-tailed alpha level of less than 0.05 was used.The NIS database discharge weight (DISCWT) was utilized to derive national estimates and complex survey modules were used to perform analyses.Multivariate logistic regression analyses were performed to evaluate the independent associations of sex and race with NAFLD-related MACCE,while adjusting for social-demographic and hospitalization characteristics and comorbidities: age,sex,race,household income quartile,payer status,type of admission,hospital bed size,location/teaching status,region,comorbidities including hypertension,diabetes mellitus,hyperlipidemia,obesity,smoking,peripheral vascular disease,prior myocardial infarction,prior percutaneous coronary intervention,prior coronary artery bypass graft (CABG),drug abuse,prior stroke or transient ischemic attack,and prior venous thromboembolism (VTE).The results of logistic regressions were reported using adjusted odds ratios (aOR),95%CI,andPvalues.The SPSS statistics 25.0 software package (IBM Corp,Armonk,New York,United States) was used for all statistical analyses.
RESULTS
Participant characteristics
Our study included 409130 NAFLD hospitalizations [median age=55 years (IQR=43-66)].Social-demographic and clinical characteristics,comorbidities and outcomes were stratified based on sex and race independently.
Prevalence of NAFLD
The prevalence of NAFLD was higher in males compared to females (1.5%vs1.2%).Among races,the prevalence of NAFLD was highest in Hispanic (2.0%) and Native American (1.9%) patients,compared to White (1.3%),Black (1.0%),Asian-Pacific Islander (1.2) and Other (1.5%).Blacks had the lowest prevalence of NAFLD (allP< 0.001,Table 1).

Table 1 Prevalence of non-alcoholic fatty liver disease based on gender and race from the national inpatient sample analysis (2019)
Sex disparities in social-demographic and clinical characteristics, comorbidities and outcomes
The females had a median age of 55 years (IQR 42-67).Despite a similar length of stay between genders,females were charged higher costs associated with the admission (41695 USDvs40952 USD).Female patients were more often from lowest income quartile,Medicare enrollees,and had non-elective admissions.Compared to males,females demonstrated lower rates of hypertension,hyperlipidemia,complicated diabetes but higher rates of obesity and uncomplicated diabetes (Table 2).
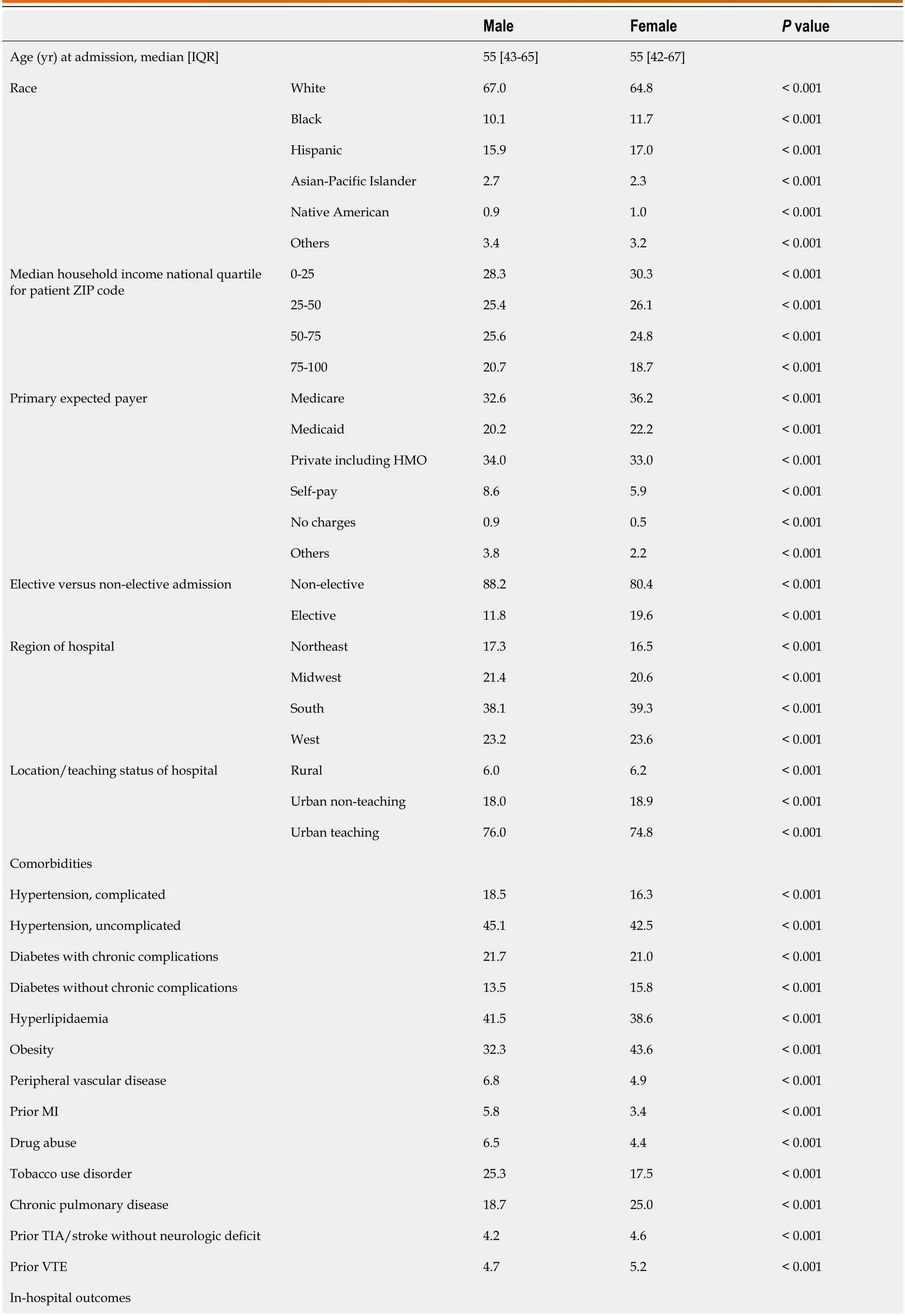
Table 2 Baseline characteristics,comorbidities and outcomes in non-alcoholic fatty liver disease hospitalizations by sex,2019,n (%)
Racial disparities in social-demographic and clinical characteristics, comorbidities and outcomes
Despite a similar length of stay across all races,the Hispanics [median age: 48 years (IQR 37-60)] and the Asian-Pacific Islanders (median age: 56 years) were charged the highest median costs (48351 USD and 51003 USD).The majority of the Hispanic patients came from the lowest income quartile (37.3%),were Medicaid enrollees (33.5%),and underwent nonelective admissions (85.7%).The Hispanics exhibited lower prevalence rates of hypertension,hyperlipidemia,but higher rates of diabetes and obesity compared to Whites (Table 3).
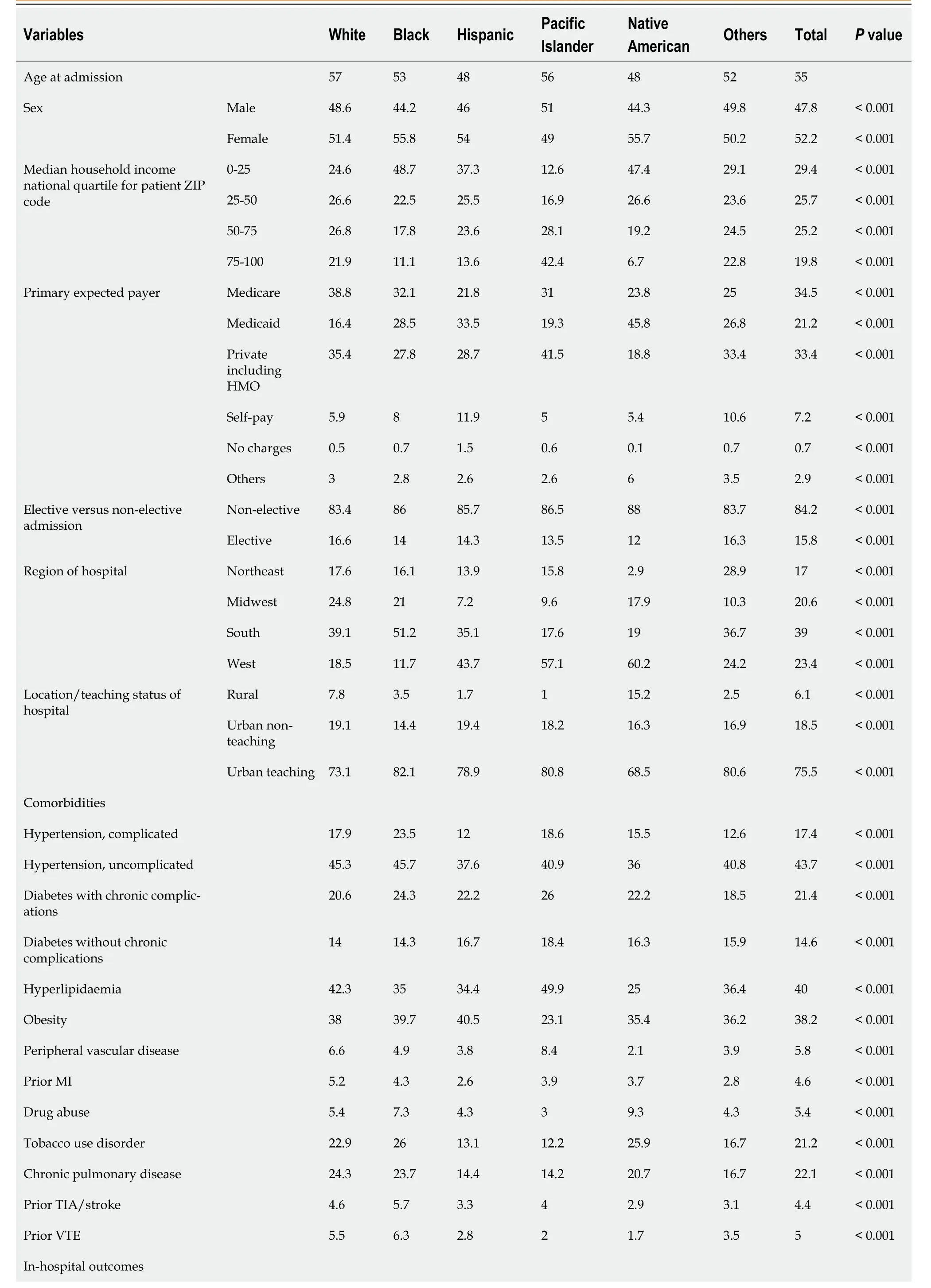
Table 3 Baseline characteristics,comorbidities and outcomes in non-alcoholic fatty liver disease hospitalizations by race,2019
Odds of MACCE, all-cause mortality, AMI, cardiac arrest, and stroke
Males had a greater risk of MACCE (aOR 1.22) (P< 0.001),AMI (aOR 1.35) (P< 0.001) and Cardiac arrest (aOR 1.54) (P<0.001).Native Americans (aOR 1.64) (P< 0.001) followed by Asian Pacific Islanders (aOR 1.18) (P< 0.001) had significantly higher odds of all-cause mortality compared to whites (aOR 1.00) (P< 0.001) (Table 4).Older patients had significantly higher odds of MACCE (aOR 3.01) (P< 0.001),all-cause mortality (aOR 4.13) (P< 0.001),AMI (aOR 2.81) (P< 0.001),cardiac arrest (aOR 2.24) (P< 0.001) and stroke (aOR 2.58) (P< 0.001) (Table 4).

Table 4 Adjusted odds of major cardiovascular and cerebrovascular events,all-cause mortality,acute myocardial infarction,cardiac arrest,stroke by age,gender and race
DISCUSSION
NAFLD is associated with obesity and insulin resistance as comorbidities.In obese individuals,the expansion of adipose tissue results in adipocyte dysfunction and increased insulin resistance,thereby leading to lipolysis.This results in elevated levels of circulating free fatty acids and leptin,with decreasing adiponectin levels,ultimately leading to intrahepatic fat accumulation.The situation is exacerbated by a diet high in carbohydrates and fat,which further contributes to fat accumulation in the liver[10].Additionally,the expansion of adipose tissue promotes infiltration of immune cells into both adipocytes and the liver,leading to chronic inflammation.Prolonged inflammation triggers hepatic stellate cells to mediate fibrosis,ultimately resulting in cirrhosis.Obesity is an independent risk factor for cardiovascular events,as it can also contribute to the development of diabetes mellitus,hyperlipidemia,hypertension,and sleep disorders,thereby indirectly exacerbating cardiovascular risks[11].
Strong evidence indicates that NAFLD causes chronic inflammation through the release of pro-inflammatory cytokines (IL-6,TNF-a,CRP),hepatokines (FGF-21,fetuin-A),adhesion molecules,and procoagulant factors from the liver,resulting in endothelial dysfunction with systemic atherosclerosis,which makes the NAFLD an independent risk factor for cardiovascular disease[12-14].Additionally,NAFLD is associated with a higher risk of left ventricular hypertrophy[15],left ventricular diastolic dysfunction[16],and atrial fibrillation[17],all of which contribute to adverse cardiovascular outcomes.It has also been reported that the presence of NAFLD is associated with poor clinical outcomes in STEMI patients and that greater severity of NAFLD is associated with higher mortality rates in such patients[18].We intended to examine the differences in cardiac and cerebrovascular outcomes (MACCE) between different sex and racial groups of NAFLD patients.This was a large-scale retrospective cross-sectional study comparing NAFLD outcomes by ethnicity and gender.
The social-demographic and clinical characteristics and comorbidities of the patients were compared over groups of sex and race.The comorbidities studied in these groups included hypertension,DM,hyperlipidemia,obesity,PVD,prior MI,prior stroke,prior VTE,chronic pulmonary disease,tobacco use,and drug use.An analysis conducted in 2015 as part of the Framingham Heart Study revealed a strong independent association between hepatic steatosis and subclinical cardiovascular disease outcomes,regardless of other metabolic risk factors[19].Furthermore,In a study using data from NHANES,patients with NAFLD demonstrated to develop increased odds of developing cardiovascular disease[20].Their study lacked to control for conditions like hyperlipidemia or systemic hypertension.However,this limitation was addressed in our study through adjustments for a comprehensive range of comorbid conditions,including hyperlipidemia and hypertension,thereby enhancing the robustness of our findings.Patients with NAFLD often have one or more components of the metabolic syndrome,which is a known risk factor for cardiovascular disease[21].This makes NAFLD independently associated with cardiovascular disease.Moreover,our study revealed that the prevalence of hypertension,diabetes with and without chronic complications,hyperlipidemia,and obesity were significantly higher in all racial groups among NAFLD patients.While the relationship between NAFLD and diabetic complications remains unclear,it is worth noting that individuals with steatosis and type 1 diabetes may be at a heightened risk of developing cardiovascular disease and subsequent cardiovascular complications[22].Therefore,it is of utmost importance to screen high-risk groups for NAFLD-related fibrosis,and the American Association of clinical endocrinology clinical practice guideline for thediagnosis and management of NAFLD strongly recommend screening patients with type 2 diabetes using the Fibrosis (FIB)-4 index[23].Other metrics such as the NAFLD activity score,a validated grading system for disease activity[24] and noninvasive assessments of hepatic fibrosis,like the NAFLD fibrosis score,are specific to NAFLD.The NAFLD fibrosis score considers factors such as age,body mass index,hyperglycemia,aminotransferase levels,platelet count,and albumin[25].Elevated NAFLD fibrosis scores may correlate with heightened cardiovascular disease mortality[26].These assessment tools are essential for stratifying the NAFLD population into distinct grading categories,enabling targeted screening for adverse cardiovascular outcomes.Establishing a causal relationship between NAFLD and cardiovascular disease will be challenging due to the complex interplay of overlapping metabolic disturbances in these individuals,such as obesity,diabetes,hypertension,atherogenic dyslipidemia,and visceral adiposity.Further research is necessary to clarify this mechanistic link.Nevertheless,regardless of causality,it is crucial for endocrinology and primary care clinicians to recognize individuals with NAFLD as being at a heightened risk of cardiovascular complications.
Our findings showed that males had greater risk of MACCE,AMI,and cardiac arrest compared to females.Native Americans,followed by Asian Pacific Islanders,were found to have significantly higher odds of all-cause mortality compared to other racial groups.The literature offers multiple studies demonstrating higher prevalence of NAFLD among males compared to females[27,28],which could be attributable to greater consumption of high-calorie drinks and alcohol,and higher frequency of insulin resistance[29].To improve this poor trend among male population,public health measures should be implemented targeting optimal control of comorbidities among males in the community.The higher prevalence of NAFLD among Hispanics is also consistent with prior studies[30].This could be attributed to a higher prevalence of chronic diseases such diabetes or metabolic syndrome,genetic and lifestyle differences,or access to healthcare among this racial group[30].Regarding genetic factors,one of the most researched genes is the Patatin-like phospholipase domain-containing protein 3 (PNPLA3),which is responsible for encoding a membrane-bound phospholipase protein that regulates the use and storage of energy resources.Hispanics more often have an allele of PNPLA3 (rs738409[G]) that causes an increased hepatic accumulation of fat compared to Blacks,who have a different allele of PNPLA3 (rs6006460[T]) that in turn results in lower hepatic fat accumulation[31].In a striking revelation,a study focusing on Native American patients with Medicare in the United States uncovered that nearly half of the patients grappled with severe cardiovascular conditions,while also bearing a heightened load of cardiovascular risk factors such as hypertension,diabetes,and hyperlipidemia[32].These alarming findings parallel our own study,which demonstrated that Native Americans faced elevated odds of in-hospital mortality.This stark correlation underscores the profound and widespread racial disparities in cardiovascular health across the United States[33].Consequently,there is a pressing need for the implementation of comprehensive multilevel interventions in healthcare,encompassing individual-and community-level factors for Native Americans and Asian/Pacific Islanders diagnosed with NAFLD,to enhance cardiovascular health.This approach must be complemented by strategic investments in communities to tackle the socioeconomic determinants of health,ultimately leading to improved cardiovascular outcomes within these populations.
Clinical implications
It is crucial to understand the implications of NAFLD,the increasing worldwide incidence of hepatic disease caused byNAFLD,aggressive public health measures are needed to target optimal control of comorbidities among the general population.This can be achieved through education on lifestyle modification,exercise,and dietary changes,including low calorie and high glycemic index foods,increased consumption of omega 3 and monounsaturated fatty acids.If lifestyle and dietary changes are unsuccessful,bariatric surgery may be considered[34].Early diagnosis and proper management of NAFLD and related risk factors are essential to prevent atherosclerosis and other cardiovascular outcomes,particularly in high risk and underserved racial and ethnic groups.Furthermore,comprehensive multilevel interventions in healthcare,addressing individual and community level factors,are urgently needed for Native Americans and Asian/Pacific Islanders diagnosed with NAFLD to enhance cardiovascular health and reduce disparities.These efforts must be complemented by strategic investments in communities to address the socioeconomic determinants of health,ultimately leading to improved cardiovascular outcomes within these populations and promoting health equity.
Limitations
This retrospective cross-sectional study has limitations tied to its reliance on ICD-10 codes for identifying NAFLD hospitalizations,potentially influenced by coding accuracy and completeness.Because it focused solely on hospitalized patients,the findings may not fully capture NAFLD characteristics in the general population.The study's use of a 2019 sample might not be entirely representative of the broader NAFLD patient population over time.The study design doesn't provide insights into causality,and unmeasured confounding variables may impact observed associations.Generalizability is confined to the United States population and may not extend to regions with different demographics or healthcare systems.Notably,the study did not consider the severity of NAFLD,including crucial factors such as NAS score,NAFLD fibrosis score,FIB-4 index,and ultrasonography findings.The absence of this information in the NIS database hinders a comprehensive understanding of the disease's nuances.Furthermore,the lack of established screening guidelines for NAFLD exacerbates the issue,as its asymptomatic nature and the absence of a correlation with elevated liver function enzymes make it easily overlooked in clinical settings.Hence,our results are only representative of a small group of patients already diagnosed with NAFLD and may not reflect the actual disease burden[13,18,35].This could be crucial when considering that certain racial groups may not have access to ideal healthcare services and meticulous laboratory evaluation and may not be aware of the severity of their NAFLD,thereby being underrepresented in the included data.Additional potential limitations may include limited availability of thorough clinical data,potential misclassification or underreporting of comorbid conditions,lack of long-term follow-up data,conceivable changes in coding practices over time,and inability to account for lifestyle and behavioral factors that could influence NAFLD and cardiovascular outcomes.
CONCLUSION
The findings from this study indicated that NAFLD is linked to a greater risk of major cardiovascular events,especially among older males,and that Native Americans and Asian Pacific Islanders with NAFLD have higher all-cause mortality.These results emphasize the need for early detection and comprehensive management of cardiovascular risk factors in NAFLD patients,as well as the significance of addressing racial and gender disparities in outcomes.Future research directions may include investigating the mechanisms involved in contributing to the increased cardiovascular risk in individuals with NAFLD,exploring sex-and race-specific risk factors,and assessing the effectiveness of targeted interventions in improving cardiovascular outcomes.Strategies enhancing access to healthcare and addressing the disparities in NAFLD-related outcomes across sexes and racial/ethnic groups may also be a subject of future research.
ARTICLE HIGHLIGHTS
Research background
This study delves into the impact of non-alcoholic fatty liver disease (NAFLD) on cardiovascular disease risk,focusing on the underexplored variances in cardiovascular outcomes across different sexes and races within a large,nationally representative United States inpatient sample.
Research motivation
The motivation for this research was to elucidate the relationship between NAFLD and major cardiovascular and cerebrovascular events (MACCE),particularly investigating the sex and racial disparities,to inform future healthcare strategies and interventions.
Research objectives
The objective was to examine the association of NAFLD with MACCE across various subgroups by age,sex,and race,aiming to highlight specific population needs and guiding tailored healthcare approaches.
Research methods
The study utilized a thorough analysis of the National Inpatient Sample,with multivariable regression models adjusted for sociodemographic and clinical factors,to compare MACCE-related outcomes in patients with NAFLD.
Research results
It found that NAFLD prevalence varies by sex and race,with adverse MACCE outcomes more common in older age groups and males,and higher all-cause mortality observed in Native Americans and Asian Pacific Islanders.
Research conclusions
The study revealed critical links between NAFLD,MACCE,age,and sex,as well as significant racial disparities in mortality rates,underscoring the necessity for customized care to improve health outcomes.
Research perspectives
This research paves the way for future studies focused on individualized patient care and highlights the importance of considering demographic variables in medical research and healthcare provision.
FOOTNOTES
Co-first authors:Rupak Desai and Ali Tariq Alvi.
Author contributions:Desai R designed the methodology and performed analysis;Desai R,Alvi AT,Vasavada A,Pulkurthi YS,Patel BA,Mohammed AS,Doshi S and Ogbu I were involved with data curation,visualization,and interpretation;Alvi AT,Pulkurthi YS,Patel BA,Vasavada A,and Mohammed AS were involved with writing of manuscript;Desai R,Alvi AT,Doshi S and Ogbu I performed reviewing and final editing;all authors have read and agreed to the published version of the manuscript;Desai R and Alvi AT are designated co-first authors,with Desai R contributing substantially to conceptualization,methodology,and editorial work,and Alvi AT to data curation,visualization,interpretation,and writing.
Institutional review board statement:Since the data included in this review were deidentified and already available in the publicly accessible databases,the IRB review was not mandatory.This review was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict-of-interest statement:The authors declare no conflicts of interest.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Rupak Desai 0000-0002-5315-6426;Ali Tariq Alvi 0009-0006-1622-334X;Advait Vasavada 0000-0002-7756-6606;Yashwitha Sai Pulakurthi 0000-0001-6195-6741;Bhavin Patel 0000-0002-0961-3132;Adil Sarvar Mohammed 0000-0002-4298-6459;Shreyans Doshi 0000-0002-8965-6748;Ikechukwu Ogbu 0000-0002-7911-833X.
S-Editor:Gong ZM
L-Editor:A
P-Editor:Zhao S
 World Journal of Cardiology2024年3期
World Journal of Cardiology2024年3期
- World Journal of Cardiology的其它文章
- Predictors of permanent pacemaker implantation following transcatheter aortic valve replacement-the search is still on!
- Mechanistic insights into fasting-induced autophagy in the aging heart
- Interest of thoracic ultrasound after cardiac surgery or interventional cardiology
- Cardiac arrest,stony heart,and cardiopulmonary resuscitation: An updated revisit
- Epicardial adipose tissue in obesity with heart failure with preserved ejection fraction: Cardiovascular magnetic resonance biomarker study
- Severe hypoxemia after radiofrequency ablation for atrial fibrillation in palliatively repaired tetralogy of Fallot: A case report
