Severe hypoxemia after radiofrequency ablation for atrial fibrillation in palliatively repaired tetralogy of Fallot: A case report
Zhi-Hang Li,Lian Lou,Yu-Xiao Chen,Wen Shi,Xuan Zhang,Jian Yang
Abstract BACKGROUND Patients with tetralogy of Fallot (TOF) often have arrhythmias,commonly being atrial fibrillation (AF).Radiofrequency ablation is an effective treatment for AF and does not usually cause severe postoperative hypoxemia,but the risk of complications may increase in patients with conditions such as TOF.CASE SUMMARY We report a young male patient with a history of TOF repair who developed severe hypoxemia after radiofrequency ablation for AF and was ultimately confirmed to have a new right-to-left shunt.The patient subsequently underwent atrial septal occlusion and eventually recovered.CONCLUSION Radiofrequency ablation may cause iatrogenic atrial septal injury;thus possible complications should be predicted in order to ensure successful treatment and patient safety.
Key Words: Atrial fibrillation;Radiofrequency ablation;Tetralogy of Fallot;Right-to-left shunt;Hypoxemia;Medical decision;Case report
INTRODUCTION
Tetralogy of Fallot (TOF) has been reported to be the most common cyanotic congenital heart disease with an incidence of 0.34 per 1000 Live births[1,2].With the development of medical technology,the survival rate of patients with TOF has significantly increased;however,long-term complications can occur.Atrial arrhythmia is one of the most common late complications after the repair of TOF (and is generally related to myopathy caused by atrial surgical scarring,right atrial dilatation,and valve reflux[3,4]).However,rhythm control and heart rate control are not effective in preventing atrial fibrillation (AF) in patients with TOF[4],and radiofrequency ablation has become an important method of treating these patients[5].Multiple studies have confirmed the safety and feasibility of this treatment[6,7],but few reports have focused on the risk of transatrial septal puncture in patients with TOF.Here,we report a case of severe hypoxemia in a patient with TOF who developed a right-to-left shunt after radiofrequency ablation for AF.This case provides an important reference for the surgical risk assessment and final decision in the treatment of similar patients,and may effectively prevent the occurrence of serious complications.
CASE PRESENTATION
Chief complaints
A 32-year-old man visited our center due to “heart palpitations for 2 mo”.
History of present illness
In the past 2 mo,the patient had persistent palpitations without obvious inducement,but there was no discomfort such as chest pain and dyspnea.
History of past illness
The patient had sustained palpitations recently and had a history of similar attacks in the past.He completed a 12-lead electrocardiogram (ECG) in the outpatient clinic and was diagnosed with AF.The patient still had palpitations and discomfort after taking metoprolol sustained-release tablets for heart rate control,and was admitted to the hospital for catheter ablation of AF.He had a history of TOF,and underwent palliative correction surgery 20 years ago,involving correction of complex congenital heart disease and pulmonary artery artificial vascular implantation.
Personal and family history
The patient denied any family history of congenital heart disease and AF.
Physical examination
Surgical scars were seen on the chest,arrhythmia was present,a systolic murmur was heard in the auscultation area of the pulmonary valve,and the cardiac boundary was enlarged.
Laboratory examinations
No obvious abnormalities were found during preoperative examinations such as routine blood and liver and kidney function tests.
Imaging examinations
The 12-lead ECG showed AF (Figure 1).Transthoracic echocardiography confirmed the changes after TOF correction and pulmonary artery implantation,with the formation of collateral circulation between the descending aorta and the left pulmonary artery,no shunt at the ventricular septum level,enlargement of the right heart,and moderate to severe tricuspid regurgitation (Figure 2).Transesophageal echocardiography did not show the atrial septal shunt,which ruled out the possibility of “pentalogy of Fallot” in this patient.In addition,pulmonary venous computed tomography angiography (CTA) was performed preoperatively to evaluate pulmonary venous structure and function,showing that the right heart was significantly enlarged,and no obvious filling defect was found in the lumen.An artificial blood vessel shadow was seen between the right pulmonary artery and the right ventricle.The left side of the descending aorta was connected to the left pulmonary artery by another artificial blood vessel (Figure 3).These two artificial vessels may have reduced the symptoms of right ventricular outflow tract obstruction.

Figure 1 The patient’s admission electrocardiogram indicating atrial fibrillation.
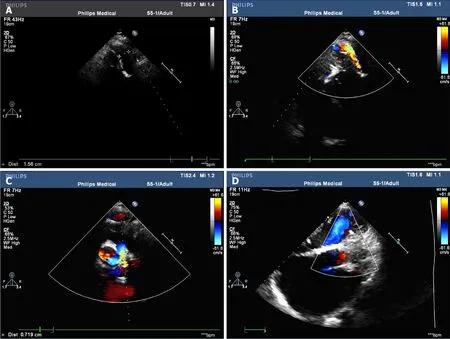
Figure 2 Preoperative echocardiography. A and B: Artificial blood vessel shadow and blood flow signal can be seen between the descending aorta and the left pulmonary artery;C: Moderate to severe tricuspid regurgitation can be seen during cardiac systole;D: No significant residual shunt was observed at the interventricular septal level.
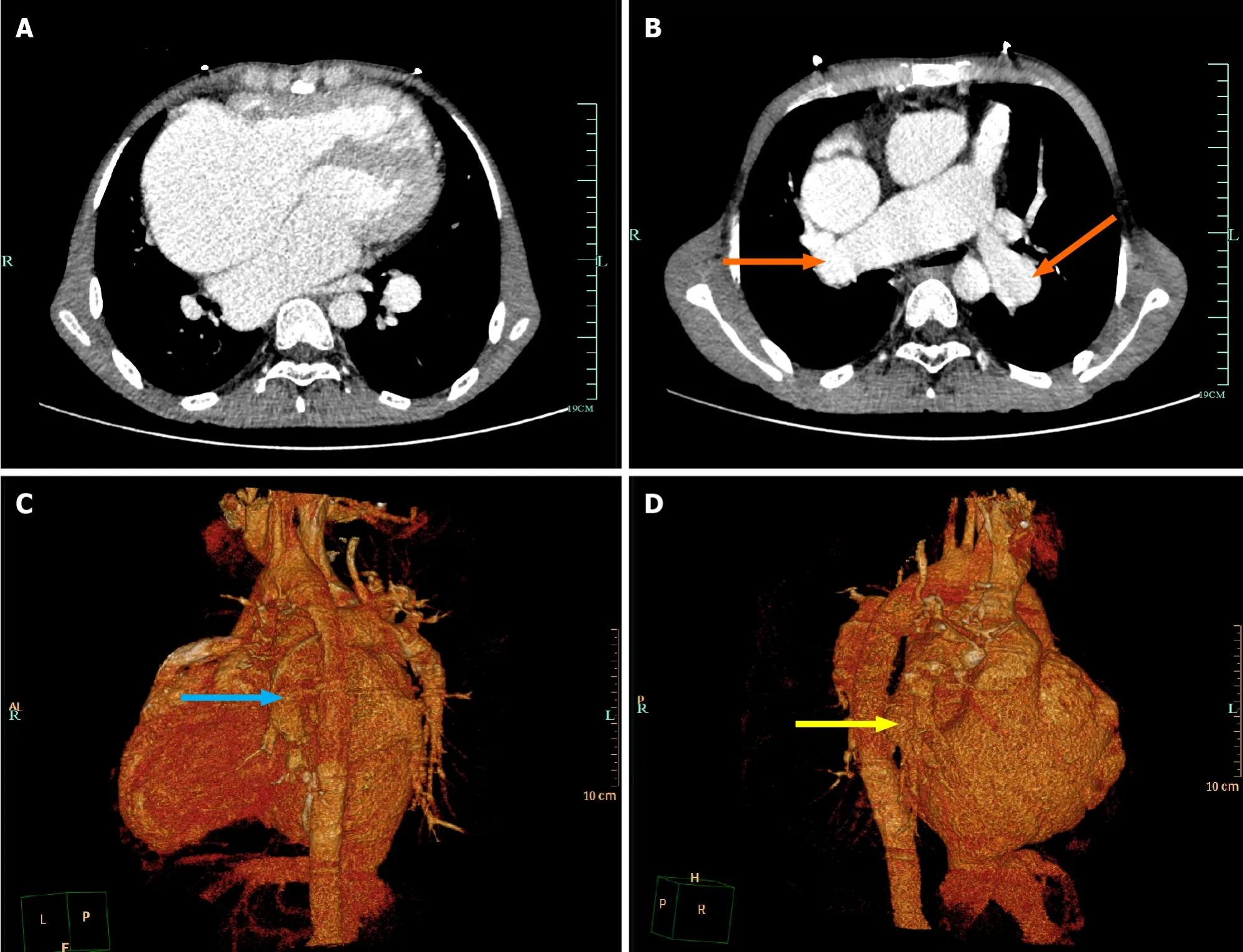
Figure 3 Preoperative pulmonary venous computed tomography angiography imaging. A: The right heart was significantly enlarged;B: Artificial blood vessel shadow can be seen on computed tomography angiography (orange arrow);C: The left side of the descending aorta is connected to the left pulmonary artery by an artificial vessel (blue arrow);D: The artificial blood vessel is visible between the right pulmonary artery and the right ventricle (yellow arrow).
FINAL DIAGNOSIS
Based on the clinical manifestations and imaging findings,the patient was initially diagnosed with AF,and post-repair for TOF.
TREATMENT
After completing the evaluation,pulmonary vein isolation and BOX isolation were performed under the guidance of the CARTO®system,and an ablation catheter was delivered to the bilateral pulmonary veins by an atrial septal puncture method under the guidance of ultrasound to complete electrical isolation during the operation.Intraoperative oxygen saturation was maintained at 90%-93%.No obvious complications were observed following catheter withdrawal.After ablation,the ECG showed sinus rhythm and dual-source atrial premature contractions.The outcome of the operation was satisfactory and met our expectations.
On the second day after ablation,the patient complained of chest tightness and shortness of breath without obvious inducement,and blood oxygen saturation decreased gradually,reaching a minimum of 50%.Oxygen saturation was only maintained at 70%-75% by oxygen inhalation.Physical examination revealed poor mental status,distention of the jugular vein,cyanosis of the mouth and lips,and decreased temperature in the extremities.Arterial blood gas analysis showed that the partial pressure of carbon dioxide was 25 mmHg,the partial pressure of oxygen was 42 mmHg,and the blood pH and bicarbonate concentration were within the normal range.Blood tests showed a brain natriuretic peptide level of 2716 ng/mL.In light of the patient’s history of congenital heart disease,acute heart failure was considered,an echocardiogram was performed,and a new right-to-left shunt approximately 9 mm wide was identified (Figure 4).After multidisciplinary consultation,hypoxemia due to circulatory hypoxia caused by an arteriovenous shunt,and atrial septal defect repair surgery were considered.However,blood oxygen saturation should be maintained before surgery to prevent damage to important organs,while endotracheal intubation was of little help to correct hypoxemia in this patient and may even have aggravated hypoxia.Therefore,the patient was transferred to the intensive care unit and a veno-venous extracorporeal membrane oxygenation intubation was performed.Postoperative oxygen saturation was maintained above 90%.Arterial blood gas analysis showed 29 mmHg of carbon dioxide and 85 mmHg of oxygen.

Figure 4 Postoperative cardiac ultrasound. A: Doppler ultrasound showed multicolored blood flow between the left and right atria,indicating the presence of atrial septal defect;B: The diameter of the atrial septal defect was about 0.88 cm.
When the patient’s vital signs became stable,we communicated with his family and an atrial defect closure was subsequently performed with insertion of a 14 mm occluder (Figure 5).Oxygen saturation was maintained above 90% in the shutdown state of extracorporeal membrane oxygenation after occlusion.Following administration of anti-infection and anticoagulation therapy,the patient’s condition improved and he was discharged.

Figure 5 Postoperative pulmonary imaging showed implantation of the atrial septal occluder.
OUTCOME AND FOLLOW-UP
The patient’s oxygen saturation was normal and there were no episodes of AF after the operation.
DISCUSSION
AF has been reported with a higher probability in patients with TOF and occurs at a younger age than in the general population[8].Ablative therapy has been proved to be an effective curative treatment modality for AF[5].A previous study proved that AF progresses more rapidly in patients with TOF and conventional antiarrhythmic drugs are not effective[4].With the development of electrophysiological techniques,the success rate of ablation at the lesion site in the presence of complex arrhythmogenic scarring and substrate in patients with TOF has improved.Current reports focus on the recurrence of postoperative arrhythmias and the quality of life of patients,and have confirmed the efficacy of radiofrequency ablation in the treatment of AF after repair of TOF[7,9].However,there have been few reports on the risks of radiofrequency ablation in patients with TOF.Due to congenital abnormalities,patients with TOF may not be able to tolerate atrial septal puncture during radiofrequency ablation in terms of cardiac infrastructure and hemodynamics.
Typically,transseptal puncture for radiofrequency ablation of AF does not cause serious complications and does not require special treatment[9].However,in this report,atrial septal puncture resulted in severe hypoxemia.It is known that patients with TOF usually develop right ventricular outflow tract obstruction,and this hemodynamic abnormality may still be present even after surgical treatment.In this case,the patient underwent TOF palliative surgery,in which the implantation of artificial blood vessels relieved some,but not all,of the pulmonary hypertension.In addition,during the preoperative ECG examination,the right heart was enlarged and the tricuspid valve showed medium-severe regurgitation,which suggested that during the systolic period,a large amount of blood flow regurgitated into the right atrium,resulting in high pressure in the right atrium.If an atrial septal defect is present at the same time,a right-to-left shunt is likely to form,resulting in hypoxemia.Transatrial septal puncture during radiofrequency ablation resulted in this condition followed by the subsequent development of hypoxemia.Unfortunately,we failed to accurately assess the right atrial pressure and predict the risk of atrial septal puncture leading to subsequent disease.
Usually,no serious pulmonary hypertension occurs after correction of TOF[10],but there are still a small number of patients with significantly increased pressure in the right ventricular outflow tract[11,12].This long-term complication not only affects the quality of life of patients,but also increases the potential risk of atrial septal puncture therapy.Preoperative elevated pulmonary artery pressure has been shown to promote the risk of right-to-left shunt in iatrogenic atrial septal defects[13].In addition,the persistence of an iatrogenic atrial septal defect leading to refractory hypoxemia has been reported in several cases[14,15],and studies have shown that patients with iatrogenic atrial septal defects are more likely to have hemodynamic abnormalities,heart failure,and other conditions[16,17].These results suggest that patients with right ventricular outflow tract abnormalities and iatrogenic atrial septal defects are more likely to develop hypoxemia.Following the diagnosis and treatment of this critically ill patient,we believe that it may be possible to effectively reduce the occurrence of postoperative hypoxemia by accurately detecting the right heart pressure through the right cardiac catheter in advance for patients with right-to-left shunt risk.This method is not only suitable for TOF,but can also be used for preoperative evaluation of patients with pulmonary malformation,pulmonary embolism,chronic obstructive pulmonary disease,and other diseases to reduce the risk of surgery.
CONCLUSION
More attention should be paid to patient hemodynamics before and after radiofrequency ablation in those with a potential risk of right-to-left shunt such as TOF patients.These patients may need to be further evaluated before or during surgery to make safer treatment decisions.This case provides an important reference for appropriate treatment decisions and perioperative management of AF under special circumstances.
FOOTNOTES
Co-first authors:Zhi-Hang Li and Lian Lou.
Co-corresponding authors:Jian Yang and Xuan Zhang.
Author contributions:Li ZH,Lou L,and Chen YX participated in the data collection,and writing and literature analysis of the article.All authors were involved in the critical review of the results and have contributed to,read,and approved the final manuscript.Li ZH was responsible for article writing and case information collection,and Lou L was responsible for article revision and literature review.Li ZH and Lou L made equal major contributions to this article,so they are listed as the co-first authors.Yang J and Zhang X contributed equally to this work as co-corresponding authors.They all provided constructive suggestions on case selection,diagnosis and treatment process,prognosis analysis,writing guidance,and so on.To sum up,the author ranking above reflects our recognition and respect for the efforts of the authors,as well as the recognition of the teamwork spirit of this research.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:The authors declare that they have no conflict of interest to disclose.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Jian Yang 0000-0002-4163-2309.
S-Editor:Lin C
L-Editor:Wang TQ
P-Editor:Yuan YY
 World Journal of Cardiology2024年3期
World Journal of Cardiology2024年3期
- World Journal of Cardiology的其它文章
- Cardiovascular diseases in European ethnic minorities: Beyond the traditional cardiovascular risk factors
- Epicardial adipose tissue in obesity with heart failure with preserved ejection fraction: Cardiovascular magnetic resonance biomarker study
- Sex and racial disparities in non-alcoholic fatty liver disease-related cardiovascular events: National inpatient sample analysis (2019)
- Cardiac arrest,stony heart,and cardiopulmonary resuscitation: An updated revisit
- Interest of thoracic ultrasound after cardiac surgery or interventional cardiology
- Mechanistic insights into fasting-induced autophagy in the aging heart
