Liver transplantation as an alternative for the treatment of perihilar cholangiocarcinoma: A critical review
Wellington Andraus,Francisco Tustumi,Alexandre Chagas Santana,Rafael Soares Nunes Pinheiro,Daniel Reis Waisberg,Liliana Ducatti Lopes,Rubens Macedo Arantes,Vinicius Rocha Santos,Rodrigo Bronze de Martino,Luiz Augusto Carneiro D’Albuquerque
Department of Gastroenterology, Transplantation Unit, Universidade de São Paulo, São Paulo, Brazil
Keywords: Liver transplantation Cholangiocarcinoma Liver neoplasms
ABSTRACT Background: Perihilar cholangiocarcinoma (phCCC) is a dismal malignancy.There is no consensus regarding the best treatment for patients with unresectable phCCC.The present review aimed to gather the current pieces of evidence for liver transplantation and liver resection as a treatment for phCCC and to build better guidance for clinical practice.Data sources: The search was conducted in PubMed,Embase,Cochrane,and LILACS.The related references were searched manually.Inclusion criteria were: reports in English or Portuguese literature that a) patients with confirmed diagnosis of phCCC;b) patients treated with a curative intent;c) patients with the outcomes of liver resection and liver transplantation.Case reports,reviews,letters,editorials,conference abstracts and papers with full-text unavailability were excluded from the analysis.Results: Most of the current literature is based on observational retrospective studies with low grades of evidence.Liver resection has better long-term outcomes than systemic chemotherapy or palliation therapy and liver transplantation is a good alternative for selected patients with unresectable phCCC.All candidates for resection or transplantation should be medically fit and free of intrahepatic or extrahepatic diseases.As a general rule,patients presenting with a tumor having a longitudinal size > 3 cm or extending below the cystic duct,lymph node disease,confirmed extrahepatic dissemination;intraoperatively diagnosed metastatic disease;a history of other malignancies within the last five years,and did not complete chemoradiation regimen and were medically unfit should not be considered for transplantation.Some of these criteria should be individually assessed.Liver transplantation or resection should only be considered in highly experienced hepatobiliary centers,and any decision-making must be based on a multidisciplinary evaluation.Conclusions: phCCC is a complex condition with high morbidity.Surgical therapies,including hepatectomy and liver transplantation,are the best option for better long-term disease-free survival.
Introduction
Cholangiocellular cancer (CCC) stands as a perplexing and devastating malignancy,posing considerable challenges to both patients and clinicians.The etiology of CCC is not yet well understood.Several risk factors,including inflammatory bowel disease,chronic liver diseases,primary sclerosing cholangitis (PSC),and genetic conditions,may play roles in pathogenesis [1].
Perihilar cholangiocarcinoma (phCCC) accounts for up to 60%of the CCC [2].Its relative rarity and a dearth of large-scale studies have hindered advancements in the understanding of the best treatment approaches [3].Surgical R0 resection remains the primary curative option for localized phCCC [4].However,most patients present with advanced disease at the time of diagnosis,rendering them ineligible for surgical resection [4].The efficacy of systemic therapies,including chemotherapy and targeted agents,has been modest at best,necessitating novel and personalized approaches to improve treatment responses [3].
More recently,liver transplantation (LT) has gained as an alternative for unresectable phCCC.LT plays a pivotal role in managing intra-hepatic neoplasms,especially in cases of unresectable tumors or tumors developed in underlying liver disease [3].For patients with intrahepatic neoplasms,LT offers a potentially curative option[5].Moreover,LT addresses the issue of impaired liver functional reserve,which is often encountered in patients with chronic liver disease and concurrent malignancies.However,there is no current consensus regarding the best approach for addressing unresectable advanced phCCC.
The present review aims to bring together the current pieces of evidence for LT and liver resection (LR) for phCCC to build guidance for clinical practice.
Methods
This review gathers scientific evidence for LT and LR for phCCC.For the construction of this review,elements of both systematic and narrative literature reviews were combined.
Database search
Our search covered the publications from January 1990 to July 2023 in PubMed,Embase,Cochrane,LILACS.We also manually searched the pertinent references.The following search terms were used: “cholangiocarcinoma”,“perihilar”,"hilar","liver resection","hepatectomy",and “liver transplantation”.
Study selection
The inclusion criteria were: (a) studies that evaluate patients with a confirmed diagnosis of phCCC;(b) outcomes of LR or LT;(c) patients treated with curative intent;(d) published in English or Portuguese;and (e) original studies,commentary articles,and systematic or critical reviews.Case reports,narrative reviews,and conference abstracts were excluded from the analysis as well as papers with full-text unavailability.
Outcomes
Treatment-related complications and long-term survival rates[overall survival (OS) and disease-free survival]were assessed.
Data extraction
Tworesearchers(TustumiF and Santana AC) extracted the following data: baseline characteristics of the included studies (study design,year of publication,sex,age,neo-adjuvant and adjuvant regimen) and the outcomes (treatment-related complications and long-term survival rates) following the defined eligibility criteria.
Data synthesis
Due to the high clinical heterogeneity of the included studies in relation to the variability of patients’ clinical status,stage,and neoadjuvant and adjuvant therapies,a meta-analysis was unsuitable;so a qualitative synthesis was used.
Results
Fifty-six studies were included.Most were observational and very few were controlled ones [4,6-60].
Routine evaluation
All patients with phCCC should be carefully evaluated for diagnosis,staging,and fitness status.A multidisciplinary team,including cardiologists,anesthesiologists,radiologists,oncologists,and hepatobiliary surgeons,should evaluate the patients to determine the best approach.
The age,nutritional status,and physical condition need to be assessed.Customized pre-rehabilitation,including physical therapy,preoperative immune-nutrition,or parenteral nutrition,should be considered according to patients’ status [6].
All patients with biliary drainage should have a bile culture sensitivity test to guide perioperative antibiotic selection [6].
Serum carbohydrate antigen 19-9 (CA19-9) level and liver enzymes should be tested [7].The serum biomarkers carcinoembryonic antigen (CEA),micro-RNA (miRNA),exostosin1 (EXT1),cathepsin B to cystatin C ratio,heat shock protein (HSP70),and angiopoietin-2 (Angpt-2) can also be used to help differentiate CCC from other types of hepatobiliary neoplasms [8].Endoscopic ultrasonography with a biopsy or a percutaneous biopsy of suspicious lymph nodes should be considered [9].
For cancer staging,magnetic resonance imaging (MRI) might be performed on a high-field scanner (1.5T or 3T) with an MR cholangiopancreatography sequence [10].Intravenous contrast injection computed tomography (CT) is more accurate than MRI in predicting vascular invasion,and 3D CT cholangiography is more useful for surgical planning [6,11].
LR
Resection of the phCCC,whenever feasible,is the better alternative compared to systemic chemotherapy or palliation.Bae et al.evaluated 117 patients with type IV phCCC.Resected patients had a significantly longer OS than non-resected patients (32.4 vs.16 months;P=0.002).Of note,40.6% of resected patients experienced severe postoperative complications [12].
Patient selection
It is common that patients waiting for surgery experience malnutrition,repeated episodes of cholangitis,and neo-adjuvant therapy related adverse events,explaining the high vulnerability.Consequently,patient selection must follow rigorous evaluation criteria to improve outcomes.Patients who are not considered fit or have poor nutritional status,even after a pre-rehabilitation program,should not be considered for surgery.
Candidates for major LR should have sufficient liver function as well as a sufficient future liver remnant (FLR).Resection should only be considered when the FLR is larger than 40% in cirrhotic patients,30% in patients presenting significant steatosis or fibrosis,and 20% in case of normal parenchyma [13].
Neo-adjuvant therapy
The systematic review by Baltatzis et al.included seven studies that evaluated neo-adjuvant therapy before LR,with a pooled number of 87 patients [14].Neo-adjuvant therapy has the potential benefit of increasing the R0 resection rate and of complete pathological response.However,neo-adjuvant therapies are quite heterogeneous across studies,with a neo-adjuvant-to-surgery time interval ranging from 3 days to 6 months.The most used chemotherapy included gemcitabine,fluoropyrimidine-and platinum-based regimens with concurrent radiotherapy ranging from 10.5 to 60 cGy.
LR procedure
LR should be performed only in centers with expertise in hepatobiliary procedures and transplantation,seeing their better both short-and long-term outcomes [15].
When the FLR is insufficient,strategies to increase the FLR such as portal vein embolization or associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) have to be considered [16,17].
Although there is no consensus on the best approach due to the lack of strong evidence,several reports indicate that a minimally invasive approach is nowadays feasible for phCCC resection and has become a valuable alternative to conventional open surgery [18].
Caudate lobe resection is mandatory to increase the likelihood of R0 resection.The Nagoya group in Japan was the first to recommend caudate lobe resection in the 1970s and 1980s [19].The Gilbert meta-analysis reported that caudate lobe resection increased the odds of R0 resection [odds ratio (OR)=5.85]and survival [hazard ratio (HR)=0.65]without increasing postoperative morbidity [20].
Frozen section analysis should be considered during the hepatectomy to check for margin involvement.If the common bile duct margin is involved wider excision and eventually associated pancreaticoduodenectomy are needed.
Outcomes
Major hepatectomy has a risk for postoperative 30-and 90-day mortality of 5% and 9%,respectively.The overall morbidity and severe morbidity were 57% and 40%,respectively [21].The risk for liver failure was 11% for left sided resection and 22% for left and right sided resection.Five-year OS rate was 43.7% after left-sided resections and 38.2% after right-sided resections [21].The main recent published series reporting long-term outcomes after LR for phCCC are displayed in Table 1.
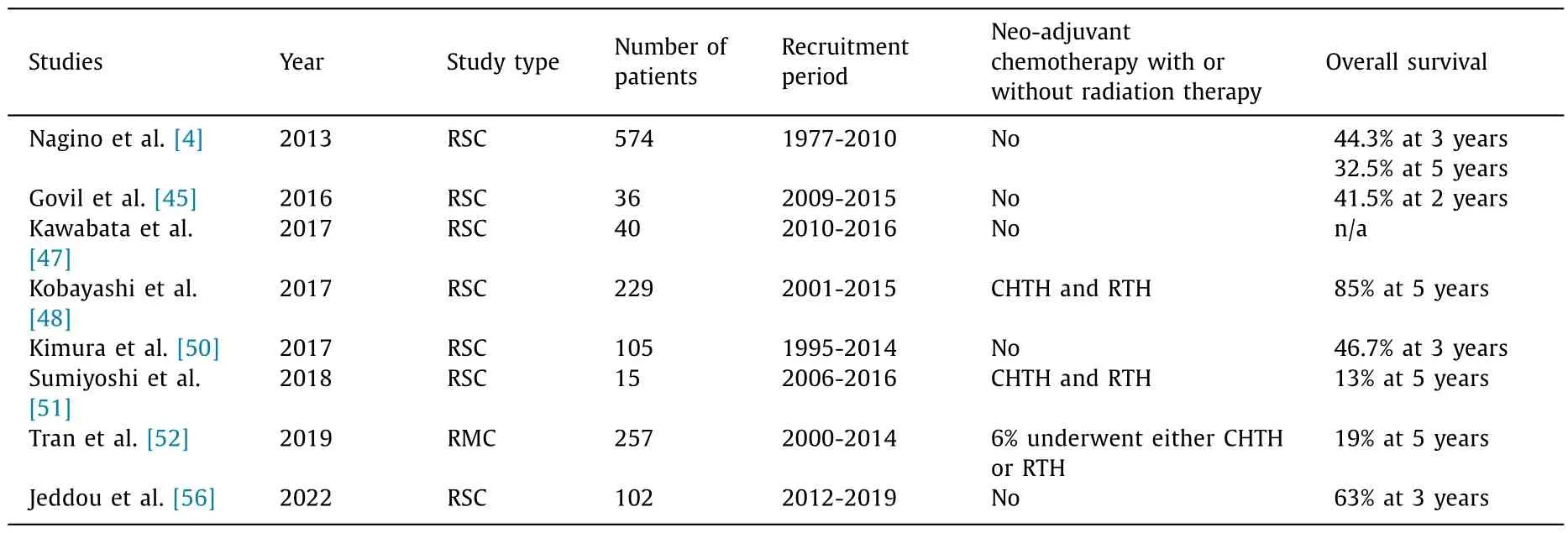
Table 1Recent literature review in relation to LR for phCCC.
Postoperative follow-up and adjuvant therapy
Adjuvant therapy,either using chemotherapy or chemoradiotherapy,may be beneficial for patients with stage III-IV phCCC.In case of compromised margins,radiotherapy should be performed [22].Treatment decisions must be based on the patient’s tolerability.Im et al.suggest adjuvant chemo-radiotherapy with a radiation dosage of 45 cGy and oral 5-fluorouracil or adjuvant chemotherapy with gemcitabine monotherapy or a combination of gemcitabine/cisplatin [22].Kamarajah et al.suggest performing adjuvant therapy for all phCCC patients after LR.In a population-based study,the benefits of adjuvant were significant even in case of node-positivity and of a positive margin resection [23].
LT and phCCC
Moris et al.compared LT to LR for phCCC in a meta-analysis.They included five observational studies.Due to the rarity,nature,and complexity of the condition,there was again a significant clinical heterogeneity among studies.Despite the absence of a significant difference in postoperative mortality,length of hospital stay was shorter in LT compared to LR,and the 3-year survival was better after LT [HR=0.61;95% confidence interval (CI): 0.40-0.93][24].
A recent large multicenter study comparing a transplanted cohort to a matched LR Bismuth-Corlette IV phCCC cohort revealed a significant improvement in the 5-year disease-free survival rate after LT (50.2% vs.17.4%) [25].
Patient selection
All candidates for LR or LT should be medically fit and free of metastatic disease according to CT scan and MRI performed within three months before LT.Patients should be assuredly unresectable or presenting an advanced underlying liver disease [26].
Generally,any of the following should be used as exclusion criteria for LT: tumor size>3 cm;tumor below the cystic duct,presence of lymph node involvement and/or extrahepatic dissemination,realization of a transcutaneous or transperitoneal tumor biopsy,previous attempt of LR,metastatic disease found at surgery,non-completion of chemoradiation regimen;medically unfitness and a history of other malignancies within the last five years.These criteria should be individually assessed [9,27-29].
Breuer and coworkers demonstrated that even in patients with potentially resectable lesions,the oncologic outcomes are better after LT compared to LR [25].
In the context of LT,it is important to determine the etiology of the phCCC.Contrary tode novophCCC,phCCC developed in an underlying primary sclerosing cholangitis (PSC) is often seen in the context of impaired liver function.Consequently,patients with phCCC and PSC will be more frequently oriented towards an LT project [30].The main indications and contraindications for LT for phCCC are listed in Table 2.

Table 2Indications and contraindications to LT for phCCC.
Neo-adjuvant therapy
Several authors proposed neo-adjuvant treatment with chemoradiation before LT [27,28].Such a tri-modal approach (radiotherapy and chemotherapy followed by surgery) aims to increase the R0 resection rate and improve long-term survival [31].Before considering neo-adjuvant chemotherapy,(internal) biliary drainage should be performed to alleviate symptoms,treat infection,and enable chemotherapy and most importantly eliminate the tumor burden [9].The role of biliary drainage still needs to be further clarified.
The Mayo Clinic team proposed a neo-adjuvant protocol with fractionated high-dose external beam and internal (iridium-192 brachytherapy) radiotherapy under chemo-sensitization using intravenous 5-fluorouracil and oral capecitabine [9].The Toronto group developed a protocol with capecitabine with hyper-fractionated external beam radiotherapy and maintenance chemotherapy with gemcitabine and cisplatin.Loveday et al.performed a retrospective analysis of patients with unresectable phCCC treated with this protocol [26].The patients were treated with conformal radiotherapy given concurrently with capecitabine.Following surgical staging,patients received maintenance cisplatin and gemcitabine until transplantation.They concluded that their treatment protocol was feasible although completed in 6 of 43 patients only.
The analysis of an European patient cohort,done by Hoogwater et al.,also concluded that neo-adjuvant chemo-radiotherapy resulted in a lower risk for recurrence but a higher risk of early liver vascular complications [32].Mantel et al.evaluated the posttransplantation complications related to this protocol.Arterial and portal complications occurred in 21% and 22%,respectively,providing an overall risk of 40% for developing vascular complications after LT in this tri-modal protocol [33].
LT procedure
Neo-adjuvantchemo-radiotherapy causes changes in the irradiated surgical field,and damage of the native hepatic artery (HA)and portal vein (PV) are especially feared.To reduce the risk of hepatic arterial thrombosis (HAT) and stenosis (HAST) induced by the changes of the native vessels,complex arterial reconstructions such as the use of free arterial interposition grafts to the infrarenal aorta [a technique that is more difficult to apply in the case of living donor liver transplantation (LDLT)]or alternative methods of arterialization to the graft such as the use of the gastroepiploic artery are advocated.The arterialization of the allograft needs to be closely monitored;in case HAT or HAST are diagnosed,early reintervention is warranted.The same holds for delayed PV stenosis.In recent years,endovascular therapies,such as balloon dilatation and/or endovascular stenting,have become an appealing and minimally invasive alternative for surgical reintervention in addressing vascular stenosis following LT.
A staging laparoscopy is necessary before LT to exclude extrahepatic disease.Routine sampling of lymph nodes along the common hepatic (8a and 8p stations) and the proper hepatic arteries,bile duct and PV (12a,12b,and 12p stations) is necessary to exclude involvement [34].Sampling nodes from the celiac trunk and along the superior mesenteric artery despite the fact that the risk for dissemination on these stations is lower,should also be done[58].
In patients with phCCC arising from PSC,microscopic involvement of the common bile duct is common,therefore frozen section analysis is mandatory during the hepatectomy to check for margin involvement.If a positive margin is identified,a re-excision or even combined pancreaticoduodenectomy must be performed [35].
Outcomes
Vascular complications are of major concern due to neoadjuvant radiotherapy.HAT,HAST,pseudoaneurysm,and eventual rupture,as well as PV,hepatic vein,and inferior vena cava stenosis or thrombosis,have all been reported [36].In the world largest(Mayo) series the incidence of early arterial complications was 5.4%,and the incidence of late arterial complications was 18.9%;PV and hepatic vein/inferior vena cava complications occurred in 37.8% and 1.4%,respectively [36].Short-and long-term outcomes of the main recently published transplant series for phCCC are displayed in Table 3.

Table 3Recent literature review in relation to LT for phCCC.
In the Mayo Clinic,LT experience for phCCC,including 237 patients,5-and 10-year OS rates reached 68% and 60%;5-year disease-free survival was 55% [37].Patients transplanted for PSC-associated phCCA had a higher long-term OS than patients transplanted forde novophCCA (74% vs.58% at 5 years;P=0.023).In the Toronto experience,using a different neo-adjuvant protocol,1-and 2-year OS rates reached 83.3% and 55.6%,respectively [38].Cambridge et al.did a meta-analysis,and the pooled 1,3-,and 5-year OS rates were 71.2%,48.0%,and 31.6%,respectively,in the absence of neo-adjuvant therapy.These results improved to 82.8%,65.5%,and 65.1% in the case of completed neo-adjuvant therapy [39].
The North American multicenter study showed that OS was significantly associated with institutional experience (5-year:HR=1.81;P=0.026).In centers having performed ≥6 LT,the 1-,3-,and 5-year OS rates were 91.8%,56.9%,and 45.8%,compared to 65.6%,48.8%,and 26.0%,respectively,in centers which performed less than 6 LT [40].
The presence residual tumor in the explant specimen has been identified as the most important prognostic factor.In this constellation 5-and 10-year OS rates reached only 45.1% and 36.1% versus 44.7% and 27.9% in PSC andde novophCCC patients respectively [36].When free margins were not achieved,the probability of 5-year OS was near 0 [55].Elderly patients,patients with elevated preoperative serum CA19-9,and large tumors have also been shown to develop more recurrences [41].PSC-associated phCCC has significantly higher survival rates thande novophCCC [42].The main sites of post-LT recurrence are the mediastinum,perihilar,abdominal lymph nodes,peritoneum,and bones [35,43].
Postoperative follow-up and adjuvant therapy
Patients should have a three-monthly reevaluation using routine biochemistry,including tumor marker CA19-9 and CT scan to look for recurrences.Immunosuppressive agents should be applied according to institutional protocols and the patient’s individual requirements [33].The pro-oncogenic effect of the immunosuppressive regimen minimizing immunosuppressive load is advocated to further impact on the risk for recurrence [59,60].
Schmelzle et al.compared LT alone to LT with adjuvant therapy with gemcitabine in a multicenter randomized trial [44].Unfortunately,the study was prematurely terminated without conclusion due to slow enrollment.In the absence of clear benefits,the use of adjuvant therapy should be based on risk stratification.Patients with high preoperative CA19-9 levels and large tumors are more likely to develop recurrence,and hence they could be considered for adjuvant therapy.Further studies are necessary to better evaluate the impact of such a strategy on outcomes after LT [41].
Discussion
During recent years,significant strides have been achieved in the field of phCCC management.These advances have brought renewed hope to both patients and healthcare professionals facing this aggressive disease.Collaborative efforts between researchers,surgeons,oncologists,radiotherapeutics,hepatologists,and pharmaceutical companies continue to drive progress,offering the promise of improved outcomes and quality of life for individuals afflicted by phCCC.
The development of surgical approaches and novel treatment modalities,including neo-adjuvant chemo-radiotherapy regimens,has expanded the range of available therapeutic options for phCCC patients.Difficult patients are defined as those who elicit strong negative emotions from their physicians.Patients previously addressed to palliation can now be candidates for both LR and LT.Since Pichlmayr et al.first documented the outcome of LR and LT in biliary tract cancer,survival rates significantly improved for both treatment strategies explained by a much better selection of the patients [61-63].Currently,LR and LT should be considered alternative potentially curative options for phCCC patients depending on the tumor characteristics and behavior.How and when to choose LT and LR as the therapeutic option remains a complex clinical decision.Both approaches offer potential benefits and must be seen as complementary procedures having both their inherent challenges.The recently obtained achievements underscore the relentless pursuit of the oncologic,surgical,and transplantation communities to find solutions in the fight against this “difficult to treat” cancer.
As randomized controlled trials are lacking and may even be very difficult to set up,there is still a low grade for the evidence for the best clinical practice in phCCC.The lack of such studies is due to the rarity of this condition leading to a very low enrollment rate,and also to the existing high pretreatment clinical heterogeneity imposing difficulty in designing treatment protocols.Identifying subsets of phCCC according to biomarker expression might allow clustering of phCCC patients within more homogenous study groups.The Methodist Houston group investigated the biomarker panel of patients with intrahepatic CCC and found clear patterns of mutations [64].The most frequently mutated genes were related to fibroblast growth factor receptor 2 (FGFR2).Future studies with target therapy toward FGFR2 and other biomarkers might represent a step forward to improve outcomes of LT and LR for phCCC [65].Such an approach may therefore of interest in the decision making process also of phCCC patients.
Multicenter prospective studies will be necessary to further evaluate the different neo-adjuvant and adjuvant regimens,as well as the respective values of LR and LT.The Mayo Clinic experience and some meta-analyses show the benefits of neo-adjuvant and adjuvant therapies;timing and type of regimen are still debated and will need further refinement.Future research holds the key to refining treatment strategies,identifying better biomarkers for better patient selection,expanding patient eligibility,and ultimately improving survival rates for this aggressive malignancy.Collaborative effort s between clinicians,researchers,and institutions are crucial to unravel the mysteries of phCCC and to improve patient outcomes.
Conclusion
phCCC is a complex condition with high morbidity.However,surgical therapies,including hepatectomy and LT,represent the best option to achieve long-term disease-free survival.A judicious patient selection alongside multidisciplinary team evaluation and surgical expertise are all mandatory to reach this goal.
Acknowledgments
None.
CRediT authorship contribution statement
Wellington Andraus:Conceptualization,Methodology,Writing -original draft.Francisco Tustumi:Data curation.
Alexandre Chagas Santana:Data curation.Rafael Soares Nunes Pinheiro:Writing -original draft.Daniel Reis Waisberg:Writing -review &editing.Liliana Ducatti Lopes:Writing -review&editing.Rubens Macedo Arantes:Investigation.Vinicius Rocha Santos:Validation.Rodrigo Bronze de Martino:Visualization.Luiz Augusto Carneiro D’Albuquerque:Supervision.
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2024年2期
Hepatobiliary & Pancreatic Diseases International2024年2期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Editors
- Information for Readers
- Meetings and Courses
- Liver transplantation and liver resection as alternative treatments for primary hepatobiliary and secondary liver tumors: Competitors or allies?
- Laparoscopic anatomical liver resection of segment 7 using a sandwich approach to the right hepatic vein (with video)
- Severe liver injury and clinical characteristics of occupational exposure to 2-amino-5-chloro-N,3-dimethylbenzamide: A case series
