Significance of balloon aortic valvuloplasty as palliative procedure for symptom benefit in patients with severe aortic stenosis
Jovica Banovic,Vladimir Djuric,Vojislav Vuksinovic,Sasa Loncar,✉
1.Department of Internal Medicine;Prijedor,Republic of Srpska,Bosnia and Herzegovina;2.University Clinical Centre of Republic of Srpska,Cardiology Clinic,Banja Luka,Republic of Srpska,Bosnia and Herzegovina
Aortic stenosis (AS) stands out as the most prevalent individual valvular defect globally.The onset and progression of AS mirror an active process akin to atherosclerosis,and the traditional triad of symptoms includes chest pain,breathlessness,and loss of consciousness.Prognosis takes a significant downturn when symptoms manifest,with mortality reaching approximately 50%-85% within the subsequent 5 years after symptom onset.[1]The risk is evidently amplified with age,and the 2-year and 3-year survival rates are reported at 37%-40%.[2]
According to the European Heart Register,aortic valve stenosis accounts for 34% of all cases of valvular heart disease,with degenerative changes being the cause in 80% of instances.[3]The advancements in civilization over the past few decades in developed countries have markedly decreased the occurrence of rheumatic heart disease.Consequently,rheumatic heart disease is responsible for only 11%of aortic stenosis cases.[4]
The surgical replacement of the aortic valve,known as Surgical Aortic Valve Replacement (SAVR),is a well-established and recommended therapeutic approach for symptomatic aortic stenosis.However,the risk of periprocedural death for patients under 70 years of age varies from 1% to 3%,while for octogenarians with significant concurrent diseases,it escalates to a range of 5% to 15%.[5]Consequently,nearly one-third of patients aged over 80 years are deemed ineligible for surgical intervention.
Introduced over 30 years ago as a potential treatment for severe AS,balloon aortic valvuloplasty (BAV)was initially regarded as unsuitable due to perceived procedural complexity,elevated restenosis rates,and post-BAV mortality rates comparable to those of untreated AS.[6,7,8]
Borderline patients with poor left ventricular systolic function,chronic obstructive pulmonary disease (COPD),and advanced comorbidities,which make them unsuitable candidates for transcatheter aortic valve replacement (TAVR) or SAVR,are increasingly undergoing BAV procedures.BAV is now being utilized more frequently within its defined indications,particularly in cases of cardiogenic shock or for symptomatic palliation.Survival rates are estimated at 50%-68% after 6 months,33%-64% after 1 year,and 18%-37% after 3 years.[9]In comparison,50% of patients with symptomatically severe aortic stenosis treated only pharmacologically succumb within two years of observation.
In recent years,there has been a renewed interest in BAV due to the rapid progression of TAVR.While the concept of BAV as an alternative to surgical aortic valve replacement has not stood the test of time,its use is still justified.According to guidelines,the application of this procedure should be limited to carefully selected patients who can achieve an improvement in hemodynamic status,potentially qualifying them for further invasive treatment.Consequently,BAV is conducted as a bridging therapy for patients in an advanced stage of the disease who are hemodynamically unstable.This approach may provide sufficient hemodynamic and clinical stability,enabling consideration for definitive therapy.BAV may also be contemplated in patients requiring emergency non-cardiac surgery or in specific cases as palliative treatment when cardiac surgery is contraindicated due to severe disease.
The objective of this study was to evaluate the clinical outcomes of patients diagnosed with severe aortic stenosis who were deemed ineligible for surgical aortic valve replacement.Our investigation focused on individuals with severe and symptomatic aortic stenosis,identified as unsuitable candidates for surgical aortic valve replacement,who underwent balloon aortic valvuloplasty within the timeframe of 2018-2022 at our institution.
The main focus of the follow-up was to assess allcause mortality at 1,6,and 12 months.Baseline characteristics were expressed as frequencies and percentages for categorical data,while numerical variables were presented as means with standard deviations.Group comparisons were conducted using a two-samplet-test or ANOVA as applicable.Cumulative mortality was visually represented through Kaplan-Meier curves,and the Log-Rank test was employed for stratified variables.
A total of 37 patients,with ages ranging from 67 to 92 years,were enrolled in the study.The average age of the participants was 80.9 ± 5.5 years.Among these patients,18 were female (48%),and 19 were male (52%).The average age for males was 81.4 years,while females had an average age of 80.4 years.Detailed baseline characteristics of the patients are provided in Table 1.
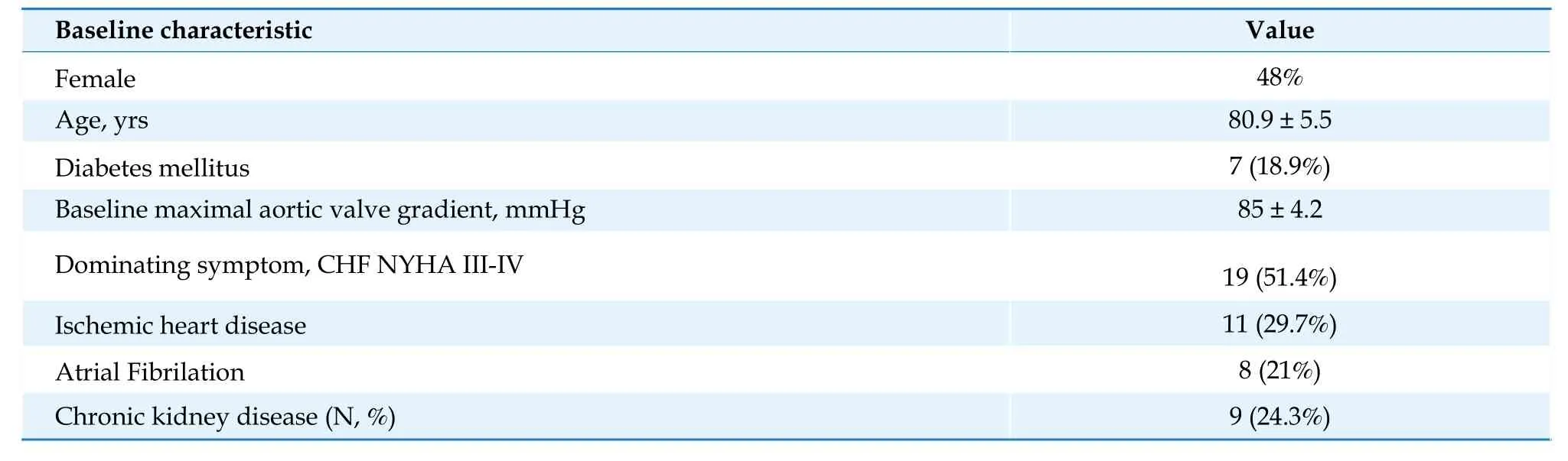
Table 1 Baseline characteristics of the patients.
Out of the total procedures,6 (16.2%) were conducted urgently in patients experiencing cardiogenic shock or multi-organ failure,while 31 (83.8%)were elective cases.19 patients (51.3%) presented with heart failure,and 18 patients (48.6%) reported symptoms such as effort angina or light-headedness.The mean value of peak systolic pressure before the procedure was 85 ± 4.2 mmHg (ranging from 39 to 136 mmHg),and the mean post-procedure value was 38 ± 3 mmHg (ranging from 20 to 68 mmHg),P< 0.001 (refer to Figure 1).
Twenty-nine patients (78.3%) experienced symptom improvement upon discharge,and only 5 (13%)required readmission within six months.One patient underwent a repeated Balloon Aortic Valvuloplasty.In-hospital deaths were reported in three urgent cases.An additional patient passed away within one month,4 patients within 1-6 months postprocedure,2 patients within 6-12 months post-procedure,and 4 patients more than one year post-procedure.This results in a total mortality rate of 14 patients (37.8%),and 27 patients (72.9%) survived more than one-year post-procedure.Figure 2 illustrates the survival function over time in months.

Figure 2 Survival function over time.
When stratified based on presenting symptoms,the presence of atrial fibrillation (AF),and gender,no significant differences were observed within groups.Dividing patients into categories of low baseline maximal gradient (less than 60 mmHg),appropriate maximal gradient (60-100 mmHg),and very severe maximal gradient (more than 100mm-Hg),no difference in survival was noted (refer to Figure 3).
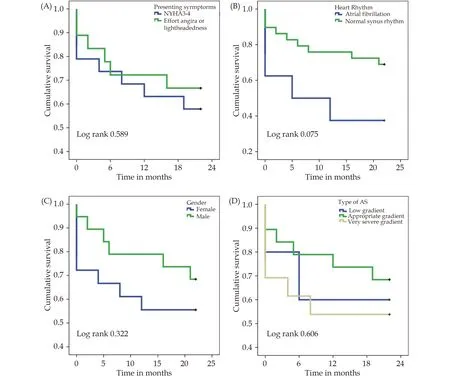
Figure 3 Kaplan-Meier survival estimates for different categorical variables.(A): Symptoms prior to procedure;(B): baseline hearth rhythm;(C): gender;and (D) different baseline maximal gradient.
Patients with persistent atrial fibrillation showed a trend toward worse survival compared to those presenting with normal sinus rhythm,although this difference was not statistically significant with a Log Rank of 0.075.No differences were noted when stratifying patients according to presenting symptoms and severity of maximal aortic gradient.A trend of higher mortality in females compared to male patients was observed but also not statistically significant with a Log Rank of 0.322.
Our case series study demonstrated that in the elderly population with severe symptomatic AS and limited life expectancy due to advanced age,comorbidities,and frailty,BAV has a low rate of procedural complications and may be considered safe.BAV may improve the patient’s quality of life.
The demographic and clinical characteristics of the patients in our study closely resemble those reported in previous studies.The majority of participants were elderly individuals with significant comorbidities,including hypertension,diabetes,renal failure,and atrial fibrillation.Specifically,18.9% of patients had diabetes,82.6% had heart failure,34.8% experienced renal failure,and 24% had atrial fibrillation.
Medical therapy is no longer a viable option for patients with symptomatic AS.[10]Although the prognosis is expected to decline with age,conservative treatment for eighty-year-olds yields 1-,2-,and 5-year survivals of 52%,40%,and 22%,respectively.Notably,these survival rates do not significantly differ from the prognosis observed in the group of patients treated with BAV,highlighting the palliative nature of this treatment.[11]This strategy serves as an appealing form of treatment that allows for future therapeutic interventions.In our study,survival reached 72.9% after one year.It is worth mentioning that mortality was higher in female patients and those with AF,but these differences did not achieve statistical significance.
Our study showed that some patients with severe AS,initially managed with medical treatment,presented as acute heart failure with multiple futility markers,including shock,renal failure,and immobility.Following the procedure,with the effective reduction of transvalvular gradients and improvement in symptoms,we illustrated that BAV can create a window of opportunity to improve or reverse AS,potentially influencing clinical outcomes and identifying candidates for TAVR.
The significance of BAV lies in its capacity to aid in valve delivery,size the device appropriately,and optimize device implantation and expansion.Performing the BAV procedure allows the team to prepare for the initiation of TAVR in the future,a procedure that is currently unavailable in Bosnia and Herzegovina.
Recent data indicates a rise in the utilization of BAV over the last decade,[12]particularly driven by a substantial increase in the number of patients eligible for TAVR.Concurrently,technological advancements have played a role in fostering this trend.
In certain scenarios,adopting a “BAV first”strategy,coupled with diligent outpatient monitoring to enhance risk factors,becomes essential to ensure the suitability and potential clinical efficacy of subsequent TAVR,particularly in low-income countries like Bosnia and Herzegovina.BAV can serve as a safe interim measure,allowing time for the recuperation of left and right ventricular function,improving congestive status,and optimizing patient conditions for subsequent TAVR.
Nevertheless,the noteworthy symptom improvement observed in 78% of patients in our study,potentially redirecting them towards alternative therapeutic pathways,should not be overlooked.
In this cohort of high-risk,elderly,frail,and comorbid individuals experiencing symptomatic severe aortic stenosis,BAV,employed as a palliative intervention,was executed with a minimal complication rate.Moreover,BAV demonstrated a substantial reduction in aortic valve gradient and an amelioration of heart failure symptoms.This underscores the pivotal role of BAV in alleviating symptoms for patients with severe AS and limited life expectancy,especially in situations where the suitability of TAVR is uncertain or deemed inappropriate due to resource constraints in developing countries.
 Journal of Geriatric Cardiology2024年3期
Journal of Geriatric Cardiology2024年3期
- Journal of Geriatric Cardiology的其它文章
- Community-based prevention and treatment of cardiovascular diseases
- Sleep quality and characteristics of older adults with acute cardiovascular disease
- The diagnostic value of tenascin-C in acute aortic syndrome
- Association of acute glycemic parameters at admission with cardiovascular mortality in the oldest old with acute myocardial infarction
- Effects of loneliness and isolation on cardiovascular diseases:a two sample Mendelian Randomization Study
- Cardiovascular risk burden and disability: findings from the International Mobility in Aging Study (IMIAS)
