Cervical cancer prevention in China: where are we now,and what’s next?
Huijiao Yan, Qiankun Wang, Youlin Qiao
1School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100730, China; 2Department of Cancer Epidemiology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
Cervical cancer (CC) epidemiology
CC, the fourth most frequently diagnosed malignancy in women worldwide, is a major global health challenge, particularly in low-resource regions.Approximately 88.1% of the 604,000 CC new cases occurred in low- and middle-income countries in 2020, and more than 90% of the 342,000 CC deaths occurred in low- and middle-income countries in 20201.China, as one of the most populous developing countries worldwide, accounts for 18% of global CC incidence and 17% of global CC deaths1.In 2016, 119,300 CC new cases and 37,200 deaths occurred in China2.Although CC incidence and mortality in China were lower than the global average level, the mortality was 2 times higher than that in the USA and UK3.Overall, the incidence and mortality rates of CC in China are increasing, particularly in rural areas(annual percentage change in incidence during 2007-2014 of 6.0 and 2.2 in rural and urban areas, respectively)4,5.Gaps in CC prevention between China and the developed world,as well as among regions of China, highlight the necessity for implementing comprehensive and sustainable CC control strategies tailored to the socioeconomic development of different areas of China.
CC elimination
CC is preventable through the adoption of multi-pronged approaches.In 2018, the World Health Organization (WHO)issued a global call for action for the elimination of CC6,and in 2020 launched the Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem, setting an ultimate goal of decreasing the incidence rate to below 4 per 100,000 women.The target is expected to be accomplished through 3 key pillars: vaccinating 90% of girls by the age of 15,screening 70% of women by 35 years of age and again by 45 years of age, and offering effective treatment to 90% of people with cervical diseases-these goals are described by the motto“90-70-90”7.Both incidence and mortality would significantly decrease if countries could achieve the “90-70-90” goal by the year 20307.China is one of the 194 countries committed to eliminating CC8.To translate this vision into tangible results,China has set targets for multiple aspects of CC prevention and control in governmental documents including the Outline for Women’s Development in China (2021-2030), the Healthy China Initiative (2019-2030), and the Action Plan to Accelerate the Elimination of Cervical Cancer in China (2023-2030).By applying a whole-government approach, these documents have established a policy foundation for strengthening multi-sectoral cooperative mechanisms and promoting financial support for exploring comprehensive CC prevention strategies, including vaccination, screening, and treatment, to expedite the elimination of CC in China.
HPV vaccination
The prophylactic HPV vaccine has been demonstrated to effectively prevent HPV-associated CC and has been progressively included in many national immunization programs.As of July 15, 2023, 122 (63%) of the 194 WHO member countries, primarily high-income countries, had introduced HPV vaccination either nationwide or partially9.By the year 2021,approximately 20% of girls younger than 15 years had been vaccinated with at least one dose worldwide, and 18 countries had reached the goal of 90% HPV vaccination coverage9.Inadequate supply chains and manufacturing capacity to meet current demands for HPV vaccines, among other political,economic, and social factors, are major reasons for the low global HPV vaccination coverage.
High demand and limited accessibility
The HPV vaccine did not become available in the Chinese mainland until 10 years after the first HPV vaccine was licensed in 2006.This decade-long delay in vaccine supply has resulted in a high demand for HPV vaccines and caused China to lag behind most countries in HPV vaccination coverage.During 2018-2020, a total of 21.6 million doses of HPV vaccines were administered in the Chinese mainland, with an estimated cumulative coverage of 2.24% among females 9-45 years of age10.Available data from Shanghai11and Tianjin12have indicated that less than 1% of girls younger than 15 years received at least one HPV vaccine dose, a percentage far lower than the global average of 20%.HPV vaccination coverage is also affected by socioeconomic, medical, and educational levels, and a relatively lower coverage rate has been reported in remote areas (ranging from 0.06% in Tibet to 8.28% in Beijing) in China10.Strategies must be devised to overcome these barriers and to make HPV vaccination available to all people needing them, regardless of location.
HPV hesitancy limits HPV vaccination
Vaccine hesitancy, one of the top 10 health threats identified by the WHO, contributes to the suboptimal HPV vaccination coverage worldwide and in China.A survey of approximately 13,000 parents of unvaccinated adolescents has found that worries regarding safety or adverse effects are the most common reasons for hesitant to vaccinate, and a lack of provider recommendation is the most common reason for unsure to vaccinate13.In China, beyond economic factors, undesirable self-efficacy and family health hinder HPV vaccination14.A lack of information, spread of misinformation, and cultural barriers can negatively affect related public service rollouts.Therefore, health education regarding HPV vaccination must be bolstered, particularly in populations with low education levels, to eradicate vaccine hesitancy.
Low-resource areas require more support
According to the Chinese Population Census Yearbook 2020,to achieve the WHO’s “90-70-90” goals, 48 million girls 9-14 years of age must be vaccinated in China, 20 million of whom live in rural areas.The government, civil societies, the private sector, and academia must collaborate to increase HPV vaccination coverage.Currently, 6 HPV vaccines are licensed worldwide: 3 bivalent, 2 quadrivalent, and 1 nonavalent HPV vaccines.More than 13 HPV vaccines are in clinical trials.The availability of 2 Chinese domestic HPV vaccines in 2019 and 2022 relieved the pressure of the HPV vaccine supply shortage to some extent, thereby accelerating the rate of increasing HPV vaccination coverage.China started to provide the first free HPV vaccinations in Jungar Banner (county level), Inner Mongolia Autonomous Region, and the vaccination efforts subsequently spread to cities and provinces.By the end of 2023,more than 30 economically developed cities and provinces(e.g., Chengdu, Jinan, Jiangsu, and Fujian) provided free or subsidized HPV vaccines for adolescent girls (Figure 1).These efforts, together with improvements in vaccine accessibility and public health education, are expected to lead to CC elimination through vaccination.However, economically less developed areas that cannot afford to provide free HPV vaccination have been neglected.Therefore, resources and funding must be directed to those areas to support the HPV vaccination rollout.
CC screening and treatment
HPV-based screening is underpromoted
Screening can quickly detect cervical precancerous lesions,which, if treated effectively and early, can be prevented from developing into CC.HPV testing has high sensitivity in the detection of cervical intraepithelial neoplasia with severity of grade 2 or greater (CIN2+) and is recommended by the WHO as the primary screening test rather than VIA or cytology (cytology and VIA are recommended as triage approaches after a positive HPV DNA test).However, HPV-based screening is constrained by economic factors and competing health priorities, particularly in high-income countries where cytological diagnosis systems are well established.In low-income counties, HPV-based screening is also limited by the substantial requirements for laboratory establishment and specimen storage.In 2019, cytology-based screening was implemented in many more countries (109/139) than HPV-based screening(35%; 48/139).VIA was the most common screening approach in low or lower-middle countries, given its low cost and easy implementation15.
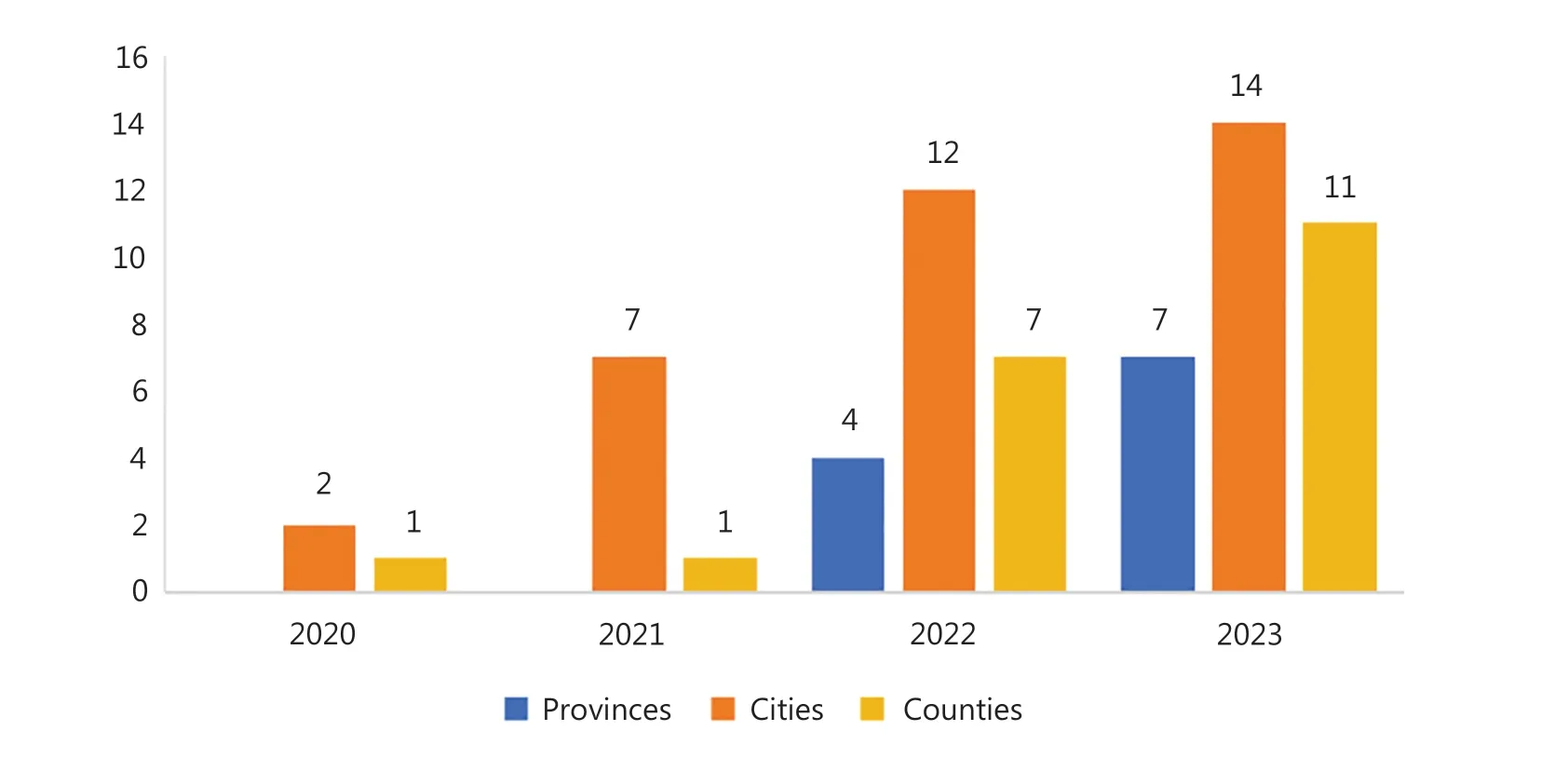
Figure 1 Number of areas providing free or subsidized HPV vaccination.
CC screening coverage is low
The screening coverage rate was notably far from the target of the global screening rate (70%).A total of 36% of women 30-49 years of age have been screened in their lifetime worldwide.In 2019, the estimated screening coverage in China (33%) was slightly lower than the global average (36%) and upper-middle-income countries (48%), was half of that in high-income countries (84%), but higher than the rates in lower-middle-income (9%) and low-income countries (11%)15.A substantial disparity in lifetime screening coverage among women 35-49 years of age exists between urban and rural areas of China(coverage of 41.1% and 32.4%, respectively)16.
To alleviate the burden of CC and promote health equity,China launched a nationwide government-organized CC screening program in 2009 in rural areas, which brought CC screening services to neglected populations and increased CC screening coverage to above 30% from nearly 0.Cytology and HPV DNA tests are recommended as primary screening methods by Chinese CC screening guidelines (2021).Substantial barriers exist to increasing screening coverage,including a shortage in qualified healthcare personnel (given that insufficient compensation from the government has weakened personnel training, particularly in rural areas),equipment allocation, health education, and screening service quality control17.Furthermore, improving data quality and compre hensiveness, and establishing an integrated surveillance system, are also crucial for evaluating screening effects.
Treatment capacity in primary health care facilities is another priority
Coverage is not always associated with effective screening.Adequate diagnosis, follow-up, treatment of precancerous lesions and CC, and management of positive test results must be implemented and strengthened simultaneously.Health care efficiency varies widely across regions of China and is lower in the western region.Because of limited diagnostic and treatment capacity in rural areas, women with positive screening results might be unable to receive timely diagnostic examination or effective treatment if they are diagnosed with precancerous lesions.Several simple treatment technologies, such as thermal ablation, are recommended for treating high-grade lesions in low-resource areas by the WHO18.Furthermore,artificial intelligence-assisted diagnostic systems, which are under development and evaluation, might be instrumental in improving the diagnostic accuracy of less experienced health workers.Introducing simple but useful technologies to primary healthcare facilities should be prioritized to increase diagnostic and treatment capacity.
Future perspectives
The incidence of CC is increasing and is expected to continue to grow in China.To mitigate or even reverse this trend to fewer than 4 cases per 100,000 women, priorities should contain optimizing prevention strategies including HPV vaccination and CC screening and treatment, as well as establishing a sustainable, integral, coordinative, and cooperative system with a broad range of stakeholders (government, civil societies, and private enterprises) to support surveillance, training,and referral.More importantly, greater resource and budget allocation should be directed toward less developed regions,to close the gap in CC prevention between rural and urban areas of China.
Improving HPV vaccination
Given the constraints on vaccine supplies, additional efforts are required to increase vaccine manufacturing capacity and strengthen the supply chain.Furthermore, a one or two-dose vaccination schedule for girls 9-14 years of age recom mended by WHO might help increase the number of girls vaccinated in both urban and rural areas.Free HPV vaccination programs are critical for improving vaccination coverage across socioeconomic strata.Hence, China should investigate cost-efficient approaches to assist more rural areas in implementing HPV vaccination programs that are free or subsidized.
Building HPV DNA test capacity
China has established CC screening service systems by initiating CC screening programs in vast rural areas of China.These programs require improvements in both personnel training and infrastructure building to improve screening quality.Specific measures include enhancing primary health worker training to improve service quality (e.g., providing professional recommendations and consultations to the public) and improving investment in laboratory establishment to introduce HPV DNA-based screening to a wider area.Moreover,HPV-based self-sampling kits can decrease dependence on physicians and could be used more broadly to reach people who are reluctant or embarrassed to visit physicians for speculum exams, or who lack access to standard physician-based sampling.
Increasing diagnostic and treatment capacity
The diagnosis and management of patients with positive results after primary screening must also be enhanced.Recently, the development and application of artificial intelligence19in colposcopy and cytology has reformed CC diagnosis by increasing diagnosis capacity, particularly for less experienced physicians,who are more likely to work in rural areas.Furthermore, a unified comprehensive surveillance and follow-up system is required for routine management of screening positive results and standardization of screening procedures.
Providing life-cycle management
CC prevention and control should be part of life-cycle management, including HPV vaccination and CC screening.The propensity toward vaccination and screening may be interrelated; for example, health-conscious people are often open to both vaccination and screening.Therefore, health education and social support networks addressing HPV infection and CC-associated stigma and discrimination should be strengthened and established, to encourage more voluntary engagement in vaccination and screening, and ultimately accelerate the elimination of CC.
Grant support
This work was supported by the Bill and Melinda Gates Foundation [Research on Expending Human Papillomavirus(HPV) Vaccination, Grant Number: INV - 006373; and Implementation Research around the Pilots of Cervical Cancer Elimination, Grant Number: INV-031449].
Conflicts of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the analysis: Huijiao Yan, Youlin Qiao.Collected the data: Qiankun Wang.
Wrote the paper: Huijiao Yan, Youlin Qiao.
 Cancer Biology & Medicine2024年3期
Cancer Biology & Medicine2024年3期
- Cancer Biology & Medicine的其它文章
- Innate IgM antibodies to mannose in patients with gastric cancer
- Peptide drugs: a new direction in cancer immunotherapy
- Reducing the global cancer burden with gastrointestinal screening: China’s 30 years practice
- Current status of early gastric cancer screening research
- A retrospective analysis of mature T- and NK-cell lymphomas
- Bronchoalveolar lavage fluid assessment facilitates precision medicine for lung cancer
