Reducing the global cancer burden with gastrointestinal screening: China’s 30 years practice
Lei Yang*, Li Feng*, Yong Zhu*, Ning Wang, Xinpu Lu, Fanghui Gu, Xiaotian Zhang,, Jiafu Ji
1Peking University Cancer Hospital (Inner Mongolia Campus)/Affiliated Cancer Hospital of Inner Mongolia Medical University,Inner Mongolia Cancer Center, Hohhot 010020, China; 2Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Beijing Office for Cancer Prevention and Control, Peking University Cancer Hospital & Institute, Beijing 100142, China; 3Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Peking University Cancer Hospital & Institute, Beijing 100142, China; 4Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Gastrointestinal Oncology, Peking University Cancer Hospital & Institute, Beijing 100142,China; 5State Key Laboratory of Holistic Integrative Management of Gastrointestinal Cancers, Beijing Key Laboratory of Carcinogenesis and Translational Research, Gastrointestinal Cancer Center, Peking University Cancer Hospital & Institute,Beijing 100142, China
Gastrointestinal (GI) cancers include esophageal [EC(International Classification of Disease 10threvision: C15)],gastric [GC (C16)], and colorectal [CRC (C18-C21)] cancers.China is a high-incidence country of GI cancers.According to GLOBOCAN2020, the number of new cases and deaths from GI cancers in China was 1,368,407 and 961,086, respectively, accounting for approximately 38%and 43% of the global new cases and deaths, respectively, in 20201.Upper GI cancers, including EC and GC, dominate in developing countries, while CRC is prevalent in developed countries2.
GI cancers derived from distinct but associated origins have diverse clinical features yet share some similar characteristics.Esophageal squamous cell carcinoma (ESCC) is the most common pathologic EC subtype in China.The main risk factors for ESCC include a preference for eating hot foods,cigarette smoking, alcohol consumption, a high-salt diet, and bad oral hygiene3.For GC, especially non-cardia GC, the main risk factors areHelicobacter pyloriinfection, a high-salt diet,insufficient fruit and vegetable intake, cigarette smoking, alcohol consumption4, and a family history of GC5.Consequently,upper GI cancers, particularly ESCC and non-cardia GC, are prevalent in countries with a low human development index(HDI), especially China.At the same time, CRC is more common in regions with a high HDI, with the main risk factors including the consumption of processed meats, overweight and obesity, lack of physical activity, and a family history of CRC6.
As global urbanization accelerates and economies develop rapidly, countries undergoing economic transitions have experienced notable shifts in digestive tract cancer patterns2.In China, this shift has manifested as a declining incidence of upper GI cancers, which is mainly due to the decreasing proportion of infectious factors.Conversely, CRC, which is primarily linked to a westernized lifestyle7, has been reported to have an upward trend.Recent data on cancer mortality in China revealed significant decreases in mortality and years of life lost (YLL) rates for all GI cancers in urban areas after age-standardization, except the CRC mortality in males8.
Owing to the large and aging population in China, upper GI cancers, despite a decreasing mortality rate, claimed 464,490 lives in 2020, resulting in 9,916,570 YLLs.CRC, with increasing annual incidence and mortality rates, causes 182,430 deaths annually, resulting in 3,884,250 YLLs8.The prevention and control of GI cancers are exceptionally serious matters in China.
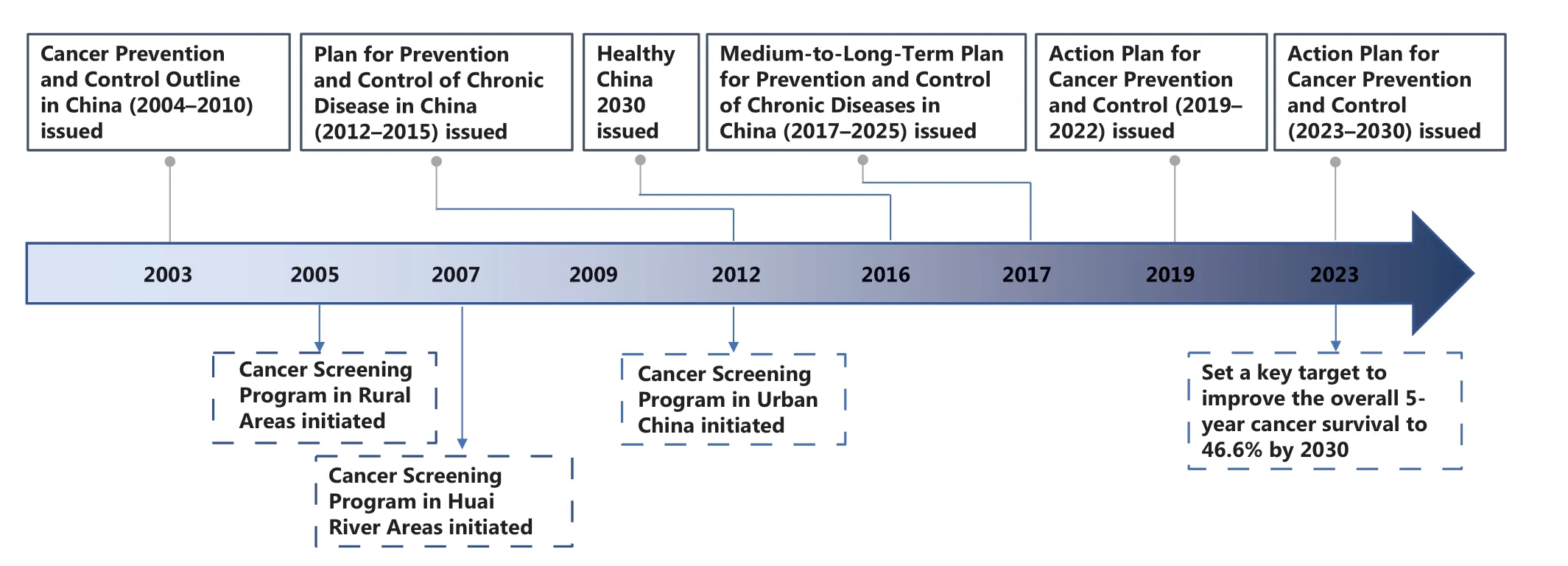
Figure 1 Key milestones for gastrointestinal cancer screening in China.
Research in regions with a high global incidence of upper GI cancers indicated that early screening can reduce the incidence and mortality.Moreover, evidence from CRC screening in the United States suggests that 50% of the decline in the mortality rate of CRC is due to early diagnosis and treatment9.
Over the past few decades, China has implemented a series of cancer prevention and control measures that have somewhat reduced the global burden of GI cancers.The Cancer Prevention and Control Outline in China (2004-2010),which was released in 2003 by the Chinese government10,initiated the following three large-scale national population-based cancer screening programs: the Cancer Screening Program in Rural Areas, which was initiated in 2005; the Cancer Screening Program in Huai River Areas, which was initiated in 2007; and the Cervical Cancer and Breast Cancer Screening Program for Women in Rural Areas, which was initiated in 200911.With the subsequent release of the Plan for Prevention and Control of Chronic Disease in China(2012-2015) in 201212, the Cancer Screening Program in Urban China (CanSPUC) was launched, which focused on non-high-incidence areas for cancer screening.These four national early cancer diagnosis and treatment programs laid the foundation for large-scale population-based cancer screening projects in China and are currently ongoing.Guided by the Healthy China 203013, the Medium-to-Long-Term Plan for Prevention and Control of Chronic Diseases(2017-2025), and the Plan for Cancer Prevention and Control (2019-2022)11were released.In the most recently released Action Plan for Cancer Prevention and Control(2023-2030)14, China announced strengthening the capacity of cancer screening and early diagnosis and set a key target to improve the overall 5-year cancer survival to 46.6% by 2030(Figure 1).Indeed, China has entered a new era in cancer prevention and control.This article summarizes 30 years of GI cancer screening and early detection practices in China,discussing the disease burden trends, to guide the formulation of cancer screening strategies in China and other developing countries.
EC
Epidemiology and disease burden
China, a high-risk country for EC, accounted for approximately 55% of global EC cases in 2020.EC is the 5thmost common cause of cancer-related deaths and the 6thmost prevalent cancer type in China.The incidence of EC in males is 1.6-fold higher than females.From 2000-2016, the annual percentage change (APC) in the EC incidence decreased by 3.9% in males and 6.4% in females, while the mortality rate decreased by 4.1% in males and 6.3% in females15.This downward trend was more pronounced among females.EC is comprised of two main pathologic types [ESCC and esophageal adenocarcinoma (EAC)].EAC is common in western countries, whereas ESCC accounts for > 90% of EC cases and is more prevalent in east asian countries, particularly in China16.The Henan, Hebei, and Shanxi provinces around the Taihang Mountains are the high-risk regions for EC in China17.In economically developed areas like Beijing, EC ranks ninth among male cancer cases but does not enter the top ten for females.The age-standardized incidence rate of EC in Beijing is 3.59 per 100,000, lower than the national average of 11.13 per 100,00018.Currently, the 5-year relative survival of EC in China is 30.3%19, but early-detected EC can exceed 90%20.Detecting EC at an earlier and potentially curable stage is crucial for improving patient survival.
EC screening in China
In Lin County, Henan Province, China has developed early detection methods for EC (esophageal balloon and sponge cytology) since the late 1960s11.Regional EC screening programs that involve performing endoscopic screening for residents 40-69 years of age in rural high-risk areas were initiated in 2005.EC screening is still included in the subsequent Huai River program and CanSPUC11.Over the past 30 years,China has established a screening modality for EC involving endoscopy with iodine staining and indicative biopsy for individuals with high risk and those with precursor lesions21.Research in high-risk rural areas has shown that endoscopic screening for precursor lesions, along with endoscopic resection or ablation of dysplastic lesions, reduces ESCC development and mortality22.In a 10-year cohort in Cixian County, Hebei Province, screening reduced EC cumulative incidence and mortality rates by 29.6% and 33.7%, respectively, compared to the control group23.In Hua County,Henan Province, the screening group displayed a 47% and 66% reduction in cumulative EC incidence and mortality,respectively24.However, the abovementioned research was based on cohort studies in areas with very a high incidence of EC.Evidence on the benefits of EC screening from randomized control trials are still lacking in China.Based on evidence from high-risk field studies spanning three decades,the current screening strategy in China prioritizes high-incidence areas or high-risk populations25.In regions with limited endoscopic resources, accurate identification of highrisk individuals is crucial for EC screening.Unlike GC, which is an infection-associated malignancy, there are currently no definite high-risk factors for EC3.To enhance the benefits from ESCC screening, Li et al.26proposed a “two-step”precision screening modality in China.First, before baseline screening, a model evaluating individual risk for “currently carrying malignant lesions in the esophagus” was adopted to identify high-risk subgroups.After the initial screening,a risk prediction model based on multiple factors, including the pathologic diagnosis and iodine staining status at baseline screening, was applied to evaluate the risk of progression of precursor lesions to malignant lesions.This protocol notably increased the protection rate of surveillance for severe dysplasia cases that had been missed with traditional pathology-based surveillance.One limitation of this study was that extrapolation of the results was restricted.
Nevertheless, the two-stage ESCC screening strategy effectively identified more EC patients while saving resources.As the number of individuals undergoing opportunistic screening increases27, this strategy can also be applied to follow-up monitoring and management of those who undergo baseline EC screening.Despite the rapid development of liquid biopsy and multi-omics technologies, there are currently no recommended biomarkers for EC screening28.
GC
Epidemiology and disease burden
The incidence and mortality rates of GC rank 3rdamong all cancer types in China, with an estimated male-to-female incidence ratio of approximately 2:1.The annual percentage change for the incidence of GC in China decreased by 3.0%in males and 2.9% in females, whereas the mortality rate decreased by 3.4% in males and 4.2% in females from 2000-201615.GC has been divided anatomically into two main subsites: cardia GC, arising from the gastroesophageal junction; and non-cardia GC, arising from more distal regions of the stomach (also referred to as distal GC)29.Distal GC is more common in the Chinese population, for whichH.pyloriinfection is a main risk factor.In recent decades, the incidence of distal GC has decreased, likely due to improved hygiene standards, increased intake of fresh fruits and vegetables, reduced consumption of salt-preserved foods, andH.pylorieradication30.The age-standardized rate (ASR) for GC mortality was 40.8 per 100,000 in males and 18.6 per 100,000 in females between 1990 and 199231.The ASR for GC mortality decreased to 17.77 per 100,000 in males and 7.13 per 100,000 in females in 201615and is expected to continue to decline in the future.Currently, the 5-year relative survival for GC in China is 35.1%19.Japan and South Korea are also high-incidence countries for GC, but report a much higher 5-year survival due to a higher proportion of early-stage diagnosis32.
GC screening in China
In China, scientific pilot study related to GC screening lags behind that of EC screening.The Peking University Cancer Hospital initiated a pilot population-based program for the early diagnosis and treatment of GC in Linqiu County,Shandong Province, a high- incidence area in China, in 198333.The regional GC screening program began in 2005 in rural areas.Based on this program, three high-incidence areas for GC (Linqu County in Shandong Province, Zhuanghe County in Liaoning Province, and Wuwei County in Gansu Province)were sellected as high-risk sites34.The cancer screening program for GC in the Huai River was launched in 2007.In the subsequent CanSPUC, which was launched in 2012, GC screening were also included in the screening programs.The target population expanded from rural high-incidence areas to high-risk populations in urban areas where the risk was low-to-moderate.In the aforementioned National Polit GC Screening Programs in China, the questionnaire-based risk assessment tool was used as the first step to select high-risk individuals.The second step involved an endoscopic examination in a designated hospital.The baseline examination findings directed follow-up recommendations for each individual21.In a multicenter population-based cohort study in high-risk areas for upper GI cancer in China, one-time endoscopic screening reduced the mortality of non-cardia GC by 61% in males and 64% in females35.Another population-based study in Linqu, China showed that receiving endoscopic screening significantly decreased the risk of invasive GC [ageand gender-adjusted relative risk (RR): 0.69, 95% confidence interval (Cl): 0.52-0.92] and GC-specific mortality (RR: 0.33,95% Cl: 0.20-0.56), particularly for non-cardia GC36.Unlike the risk factors for EC,H.pylori-induced gastritis is likely to be a major step in the development of GC, and therefore, serum markers associated with chronic atrophic gastritis and intestinal metaplasia are used as potential indicators for identifying high-risk individuals.
Consequently, population-basedH.pylori“test and treat”strategies37were used in the high-risk field with a focus on serologic determination of five biomarkers (PGI, PGII,PGI:PGII ratio, anti-H.pyloriantibodies, and gastrin-17)34,38.Patients with different risks underwent various endoscopy screening modalities based on risk stratification strategies29.A meta-analysis of seven randomized controlled trials (RCTs)involvingH.pylorieradication in healthy individuals demonstrated a 46% decrease in the incidence of GC.Among the four studies that assessed subsequent mortality, there was a significant decrease in cancer-specific mortality among treated individuals39.
瘦客户机(thin client)与传统PC机的功能相似,不同的是瘦客户机其实就类似于一个无盘工作站,数据和应用都存储在后台服务器上。瘦客户机自身只包含嵌入式高运算处理器、本地闪存、网卡、显卡和一些常用的外设等硬件。正是由于瘦客户机硬件配置简单优质的特性和后台服务器高速运算处理能力,才使得瘦客户机能够快速替代传统PC机得以推广应用。目前,瘦客户机作为服务器客户终端被应用在教育、政务、医疗等多个领域中,多媒体教学和计算机实训教室的应用是高校云终端最主流的应用场景。
CRC
Epidemiology and disease burden
CRC is the 2ndmost commonly diagnosed cancer and 4thleading cause of death in China15.A westernized lifestyle,which is characterized by excessive consumption of processed meats, overweight/obesity, and prolonged sedentary behavior, is a risk factor for the development of CRC2.The annual percentage change in the incidence of CRC in China increased by 2.4% in males and 1.2% in females from 2000-2016, with a 1.3% increase in the mortality rate in males and no significant increase in the mortality rate in females15.The ranking of CRC deaths is positively correlated with the level of economic development.According to cancer mortality burden data from the Chinese Center for Disease Control and Prevention in 2020, CRC ranked as the 2ndleading cause of cancer-related deaths in males in Beijing and Shanghai,3rdin Jiangsu and Guangzhou, and lower in other provinces.Among females, the ranking of deaths also exhibits similar characteristics to that of males across different economic development regions8.
Of adults aged 50-75 years, 58% underwent colonoscopy screening in the US in 2013, prompting a national campaign in 2014 that aimed to increase the CRC screening prevalence to 80% in the eligible population by 201840.Reaching this goal is estimated to avert 280,000 new cases and 200,000 deaths of CRC by 203041.The latest data show that since the nationwide CRC screening recommendation in the United States, the mortality rate for CRC decreased by 55% among males and 61% among females42.The CRC screening experience in the United States warrants adoption in China.
CRC screening in China
Significant benefits can be obtained from CRC screening because grossly visible lesions typically take 10-15 years to progress to CRC, leaving a wide time window for early diagnosis43.Screening can remove precancerous lesionsviacolonoscopy or detect cancer at an earlier stage, thereby reducing the incidence and mortality, and alleviating the CRC burden44.Adenomas and serrated polyps, the two primary subtypes of lesions, are precursors to most sporadic CRCs,85%-90% of which evolve from adenomas2.A sequential screening program combining high-risk factors and fecal occult blood testing (FOBT) has been implemented in the general population of Jiashan County, Zhejiang Province,China since 198945.The individual with a positive result will then undergo further colonoscopy screening.Fecal immunochemical testing (FIT) was not initially used as the primary screening method for high-risk individuals in the CanSPUC.Instead, those individuals identified as high risk based on questionnaire were referred to designated hospitals for colonoscopy screening46.However, recognizing that the FIT can improve compliance with colonoscopy screening in high-risk populations47, the FIT and questionnaires were included as the primary screening methods to identify high-risk individuals for CRC in CanSPUC beginning in 201648.Although FIT has been recommended as a first-step population screening approach in China, the accuracy of FIT is low.FIT-DNA is more sensitive for detecting advanced precancerous lesions and CRC than FIT, but has more false-positive results and is expensive49.Consequentlly, FIT-DNA is not recommended for use in China’s National Cancer Screening Programs.Although comprehensive CRC screening strategies have been implemented in European countries and in the United States for decades, China lacks a nationwide CRC screening plan.Furthermore, there is still no evidence from large-scale population screening in China demonstrating that colonoscopic screening for CRC can reduce mortality rates.
The best evidence to support the use of colonoscopy in China Guidelines for the Screening, Early Detection, and Early Treatment of Colorectal Cancer (2020, Beijing) was limited to meta-analysis results from 5 cohort studies, which estimated that colorectal screening was associated with a 56%decrease in the incidence of CRC and a 57% decrease in the risk of death50.Most evidence released based on the National Screening Program in China always focus on the uptake and early detection rates of precancerous lesions and cancer47.The National Cancer Center of China initiated a randomized controlled trial for CRC screening in 2019 but the results have not been published51.
Challenges for GI cancer screening
China has a vast territory and large population with significant variations in GI cancer disease burden and healthcare resources.National pilot cancer screening programs and population-based cohort studies launched over the past three decades have played an essential role in exploring suitable screening modalities in China11.However, many barriers and challenges have not been addressed.
Identification of high-risk individuals
There are no nationwide screening recommendations for GI cancers in the general population in China50.A two-step screening strategy (i.e., a non-invasive or minimally invasive approach to select high-risk individuals and those who should undergo endoscopy) for GI cancer screening in high-incidence areas is cost-effective.The accurate identification of high-risk individuals who may benefit the most from screening is crucial in low- and moderate-risk areas47.Currently,high-risk population assessment methods used for specific age groups in national GI cancer screening programs, including questionnaires11,46, risk prediction models33, and bloodbased biomarkers50, all have limited sensitivity and positive predictive values.Moreover, the cost-effectiveness of these assessment methods in population settings remains unclear.New emerging technologies, such as multiomics combined with artificial intelligence for cancer screening, are still in the research stage.Some marketed products are expensive and have not reached a level for widespread use in population screening52.
Endoscopy examination
The performance quality of GI cancer screening by endoscopists varies significantly in different healthcare and resource-level areas of China58.The protective effects of colonoscopy and subsequent surveillance strategies may vary according to endoscopist performance.A study assessed 259,885 colonoscopies by 361 endoscopists in the Austria quality assurance program for screening colonoscopies.The study revealed higher CRC mortality rate when the endoscopist had an adenoma detection rate (ADR) < 25%59.A current issue in China is a lack of professional endoscopists with high-performance quality, which is especially pronounced in economically underdeveloped areas.The Chinese Preventive Medicine Association released a plan to train physicians and program coordinators from county-level hospitals and cancer screening institutions in 2020 to improve the capacity and performance quality of cancer prevention and management60.
Follow-up and endoscopic surveillance
Currently, population-based follow-up for cancer screening in China is inadequate.High-risk individuals’ follow-up after baseline examination at most cancer screening sites in China relies on passive linkage with outcomes from the population-based cancer registry or death certification database.Precise follow-up of individuals with abnormal findings after baseline screening is crucial for GI cancer screening with a focus on identifying precursor lesions.Another issue is to release clear recommendations regarding the surveillance intervals.The natural history of esophageal, gastric, and colorectal cancers follows the process from precursor lesions to cancer, which is quite different.Therefore, personalized surveillance intervals should be established for different types of cancer and pathologic characteristics based on the histologic type at baseline screening.There is a lack of high-level evidence in the Chinese population regarding the endoscopic surveillance interval28,50,61.
Screening policies
Population coverage is crucial for the effectiveness of cancer screening in China.Given the large population and limited resources, regular cancer screening of the entire eligible population in China can be unrealistic.Although the National Cancer Screening Program’s coverage is gradually expanding,population-level coverage for the top 5 cancers in China is still< 1%11,19.The government should take various measures to increase the proportion of the screening population, including improving the proportion of the awareness of core knowledge on cancer prevention and control among Chinese residents and encouraging opportunistic cancer screening.
Conclusions
Over the past three decades, China has implemented a series of cancer prevention and control measures, contributing to a global reduction in cancer burden.Despite significant progress, continuous exposure to risk factors, such as obesity and population aging in China, may increase the health burden of GI cancers in the future.To address this, China should persist in promoting EC screening in high-incidence areas, explore sensitive biomarkers and risk prediction models for GC and CRC, and investigate non-invasive screening alternatives for endoscopic examination to improve uptake rates.Additionally,efforts should be made to enhance the quality of large-scale population screening data, strengthen data sharing and cooperation, and increase research funding for GI cancers.
Grant support
This work was supported by grants from the Clinical Need Oriented Basic Research Project of Inner Mongolia Academy of Medical Sciences (Grant No.2023GLLH0132), Scientific Research Fund for the Demonstration Project of Public Hospital Reform and Quality Development (Gastrointestinal Tumor) that is approved by Peking University Cancer Hospital[Inner Mongolia Campus (Grant No.2023SGGZ068)], and the Beijing Hospitals Authority Youth Programme (Grant No.QML20211102).
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the contents: Xiaotian Zhang and Jiafu Ji.
Retrieved and selected the literature: Xinpu Lu, Fanghui Gu,and Ning Wang.
Wrote the paper: Lei Yang, Li Feng, and Yong Zhu.
 Cancer Biology & Medicine2024年3期
Cancer Biology & Medicine2024年3期
- Cancer Biology & Medicine的其它文章
- Erratum to Treatment strategies for patients with HER2-positive gastric cancer
- DNA damage response-related immune activation signature predicts the response to immune checkpoint inhibitors: from gastrointestinal cancer analysis to pan-cancer validation
- Bronchoalveolar lavage fluid assessment facilitates precision medicine for lung cancer
- A retrospective analysis of mature T- and NK-cell lymphomas
- Current status of early gastric cancer screening research
- Cervical cancer prevention in China: where are we now,and what’s next?
