Effect of corneoscleral lenses on visual acuity and corneal parameters in patients with keratoconus
Ali Ayatollahi1,Haleh Kangari1,Saeed Rahmani1,Seyyed Mehdi Tabatabaie
Abstract
•AIM:To investigate the effect of wearing corneoscleral contact lens on visual acuity,and corneal parameters in keratoconus patients.
•METHODS:In this prospective study,43 cases (83 eyes) with keratoconus were included and examined. A corneoscleral contact lens was fitted,and thorough exams were carried out at baseline,3 and 6 mo after wearing lenses,including slit lamp examination,objective and subjective refraction,uncorrected visual acuity (UCVA),and best-corrected visual acuity (BCVA),keratometry (Kmax,K1 and K2),central corneal thickness and endothelial cells count.
•RESULTS:Mean BCVA (LogMAR) improved from 0.34±0.23 with the spectacles to 0.03±0.05 with the corneoscleral contact lenses in 6 mo (P<0.001).Kmax changed from 52.80±5.93 D to 51.51±5.64 D in 6 mo (P<0.001),central corneal thickness changed from 483.84±34.69 μm to 476.28±35.38 μm (P<0.001),and endothelial cell count changed from 2559.18±275.7 cells/mm2 to 2572.73±274.3 cells/mm2 after wearing corneoscleral contact lens for 6 mo (P<0.001).
•CONCLUSION:Corneoscleral lenses could significantly increase visual acuity,since there were no clinical noticeable changes in the corneal parameters,this lenses can be used safely in patients with keratoconus.
•KEYWORDS:corneoscleral contact lens; keratoconus; corneal topography; corneal thickness
INTRODUCTION
Keratoconus is a bilateral and asymmetric corneal degeneration which is characterized by local corneal thinning.Both the inferior-temporal region and the center of the cornea often experience this corneal thinning[1-4].According to recent meta-analysis that included more than 50 million individuals from different countries determined that the worldwide prevalence of keratoconus was 1.38 per 1 000 people[5].By developing irregular astigmatism and corneal abnormalities,this disease reduces patient’s vision[2-3,6].Keratoconus management usually depends on the severity and degree of the disease[7].Most people with keratoconus need to use contact lenses to increase visual acuity[1].Rigid contact lenses (RGP; corneoscleral,scleral) cover corneal irregularities using tear film,and increase the quality of vision[2,3,8-10].A reduction in the need for surgery was reported following the use of contact lenses[5].Despite good vision that a corneal rigid gas permeable contact lens provides for a person,because of issues including decentration,excessive movement,prismatic effect-induced binocular problems,and discomfort for the user,they may decide not to wear it[1,5,8,11-12].
In order to fit properly,corneoscleral contact lenses with a diameter of 12.50 mm to 15.00 mm should not come into contact with the cornea[1,13-14].This prevents mechanical stress from being placed on the corneal surface[15-16].Since the fluid rests between corneoscleral contact lens and cornea,a better quality of vision versus corneal contact lenses is expected[17].Regarding the stability of these lenses and their proper centration,the high-order aberrations of the eye are reduced and the quality of vision is increased[17-18].
Due to the large size and hard materials used in the manufacture of these lenses,it is expected to cause many short-term changes in the cornea[18].Furthermore,few studies were conducted on the performance of corneoscleral lenses,especially with diameters smaller than 13.00 mm,and their effect on the cornea is not clear[17].Due to the interstitial diameter of the lenses,they may be an option to improve the quality of vision and comfort in patients who cannot tolerate RGP corneal lenses or have difficulty with handling of scleral lenses[19].
This study aims to investigate the effect of using 12.60 mm diameter corneoscleral lenses on the visual performance,and corneal parameters of the patients with keratoconus so that they can be examined for safety and health.
SUBJECTS AND METHODS
EthicalApprovalThis research was approved by the ethics committee of Shahid Beheshti University of Medical Sciences under the code IR.SBMU.RETECH.REC.1400.605.A written informed consent was obtained from all participants.
In this prospective study,83 eyes of 43 patients with keratoconus were examined.The diagnosis of keratoconus was based on corneal tomography,keratometry findings and also presence of at least one sign in slit-lamp examinations including stromal thinning,observation of Fleischer rings,and Vogt’s striae.
After the definite diagnosis of keratoconus,the advantages,and disadvantages of using corneoscleral lenses and the follow-up rate of the study were explained to the patients,and if willing,the consent form was filled out by the patient.The inclusion criteria were:the absence of movement-limiting issues,the ability to properly care for contact lenses,the absence of unfavorable environmental conditions for the wearer,and the patient’s absence of other eye issues such as retinal and vitreous issues,increased intraocular pressure,colobomas in various parts of the eye,uveitis,and the lack of any eye surgery and systemic diseases are among the inclusion criteria.
The eye examinations carried out include slit lamp examinations,the measurement of uncorrected visual acuity (UCVA),and best-corrected visual acuity (BCVA),objective refraction with auto-refractometer and retinoscopy,subjective refraction,corneal topographic analysis using the Pentacam AXL Eye Scanner (Oculus Inc.,Wetzlar,Germany),determining the central thickness of cornea using ultrasound pachymetry,determining the corneal endothelium cells count using Specular microscopy (EM-3000,Tomey Inc.,Japan).
The lenses (Iran Lens Gostar Company,Iran) used in this study were corneoscleral with a diameter of 12.60 mm and a curvature of 6.80-8.00 mm and a refractive power between +8.00 D and-14.00 D.These lenses were aspheric and consist of three curvatures:central base curve,midperipheral curvature and peripheral curvature.Their ingredients are BOSTON XO and Hexafocon A,which are placed in the category of Fluoro-silicone acrylate materials and have DK/T=100.
Trial lenses are used for fitting corneoscleral lenses based on the manufacturer’s instructions.First,based on central corneal keratometry,a lens with a base curve suitable for corneal keratometry (0.1 flatter than the flattest corneal meridian) is placed on the patient’s eye and the lens stays on the cornea for 30 min,then examinations started using fluorescein and cobalt light with slit lamps.The midperipheral and peripheral curves should be chosen after the central curve has been produced for a good fit.The lenses were examined to see whether they were properly fitted,including their positioning on the cornea,movement,and the presence of tears under the lens.The lens should not be in touch with the cornea in any part,and should not put pressure on the limbus.After choosing the right curves,correct lens power is obtained using the objective and subjective method.After determining the right lens,the wearer was fully taught how to wear and remove the lens correctly and how to maintain it,as well as how to start using the lens gradually during the first days,after that they started to use the lenses in the form of full daily schedule.Follow-up examinations included 1 wk,1,3,and 6 mo after the first session.Complete examinations,such as slit lamp examinations,measurements of UCVA and BCVA,objective and subjective refraction,corneal topography using a Pentacam device,corneal central thickness determination with pachymetry,and corneal endothelium cell count by specular microscopy,are performed in the sessions scheduled 3 and 6 mo later.The examinations were repeated at least twice,and if necessary,they were performed more times,and one of the two similar ones was chosen.G Power software was used to determine the sample size.All data were eventually entered into the tables and analyzed by SPSS-18.To compare the possible changes during the follow-up sessions,repeated measure test was done.Also,for pairwise comparisons before and after the contact lens fit (baseline,3 and 6 mo),pairedt-test were used,and if any variable was not normal,Wilcoxon test were used to compare the mean before and after the contact lens fit.
RESULTS
Based on inclusion criteria,83 eyes from 43 cases with virgin keratoconus were examined.The mean age of patients was 29.55±6.74 years.There were 26 males (60%) and 17 females (40%).None of the patients had serious problems using contact lenses.Figure 4 shows the contact lens fitted on a patient’s eye.Two cases had mild discomforts and conjunctival hyperemia,which were treated with corticosteroid eye drops and a brief suspension of contact lens use.Table 1 shows the characteristics of visual acuity and cornea of patients in the first examination session.Repeated measure test showed that all parameters significantly changed during the follow-up sessions.
VisualAcuityThe mean BCVA (LogMAR) using spectacles was 0.34±0.23,and the average BCVA (LogMAR) using corneoscleral contact lenses was 0.06±0.07.Therefore,there was a statistically significant difference between the two types of correction (P<0.001; Table 2).Furthermore,the mean BCVA (LogMAR) at 3 and 6 mo after corneoscleral contact lens insertion were 0.04±0.06 and 0.03±0.05,respectively.
KeratometryThe average of Kmax before wearing contact lenses was 52.80±5.93 D,while it was 52.02±5.79 D and 51.51±5.64 D at 3 and 6 mo after using contact lenses,respectively.Statistically,keratometry changes were significant before contact lens insertion,and 3 mo after contact lens insertion,as well as before contact lens insertion and 6 mo after contact lens insertion (P<0.001).There is no significant difference between over 29 years old patients with the group under the age (P=0.1).
There is a significant difference between the average K1 (flat meridians) before lens insertion and 3 mo after lens wear,as well as before lens insertion and 6 mo after corneoscleral contact lens wear (P<0.001).
From a statistical point of view,there is no significant difference between the average K2 (steep meridians) before lens insertion,and 3 mo after using a corneoscleral lens (P=0.12),but there is a significant difference between the average K2 before lens insertion and 6 mo after wearing corneoscleral lenses (P<0.001; Figure 1).
CornealThicknessThe average corneal central thickness before wearing corneoscleral contact lens was 483.84±34.69 μm,which changed to 478.55±35.58 μm and 476.28±35.38 μm at 3 and 6 mo after using the contact lens using pachymetry (Table 3).Statistically,the changes in the corneal central thickness were significant before contact lens insertion and 3 mo after use,as well as before contact lens insertion and 6 mo after contact lens use (P<0.001; Figure 2).The thinnest point of cornea with Pentacam before wearing corneoscleral contact lens was 473.84±37.33 μm,which changed to 469.65±37.56 μm and 466.79±37.90 μm at 3 and 6 mo after using the contact lens,respectively.The changes in the thinnest corneal thickness were significant before contact lens insertion and 3 mo after use (P<0.000).There is no significant difference between over 29 years old patients with the group under the age (P=0.15).
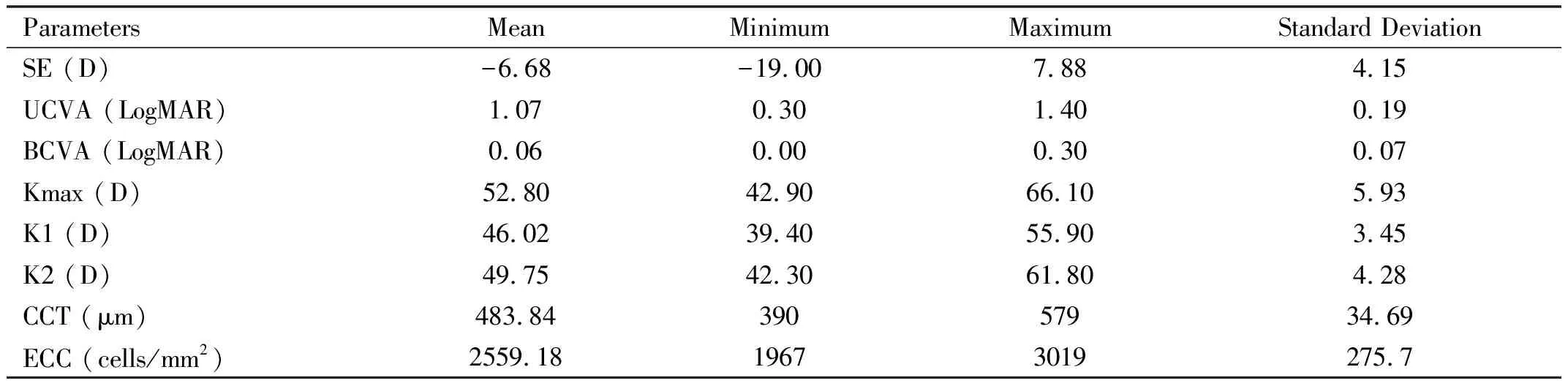
Table 1 Summary of visual acuity and corneal parameters of patients in the first examination
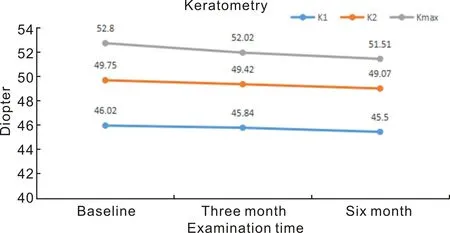
Figure 1 Differences in keratometry parameter values before the initial fitting,after 3 and 6 months of corneoscleral lens wear in the patients.
Table 3 Corneal central thickness before the initial fitting and after 3 and 6 months of corneoscleral lens wear in the patients μm
TheCornealEndotheliumCellsCountThe mean of corneal endothelium cells count before contact lens use was 2559.18±275.7 cells/mm2,and this number changed to 2575.73±274.8 cells/mm2and 2572.73±274.3 cells/mm2at 3 and 6 mo after using the corneoscleral lens,respectively (Table 4).Statistically,changes in the corneal endothelium cells count before contact lens insertion and 3 mo after wearing and before contact lens insertion and 6 mo after wearing it were significant (P<0.001; Figure 3).
DISCUSSION
The use of corneoscleral lenses is not widespread despite its benefits in the visual correction of patients with a variety of corneal abnormalities,including keratoconus.It may be presumed that its usage has been restricted due to worries about the pressure of the lens edges on the corneal limbus and stem cells[17,19-20].
The size of contact lenses leads to different placement on the eye,which in turn can affect the quality of vision and patient comfort[19,21],since the diameter of the corneoscleral lenses is smaller than scleral contact lenses and larger than RGP contact lenses,the benefits of the both types of contact lenses are achievable.
Results of this study show that the visual acuity increases significantly using the corneoscleral lenses,and this increase in visual acuity during the three and six-month examinations is considered clinically stable.This effect was observed in similar studies,and in most of the studies,the increase in visual acuity using contact lenses has been significant[2,8,19].
The corneal keratometry (K1,K2,Kmax) has become statistically flatter after using a corneoscleral lens,but it is not considered a significant change clinically.In a study conducted by Montaltetal[17],the average keratometry remained constant during one year of using this type of contact lenses,but in another study by Montaltetal[19],regarding the performance of corneoscleral lenses in patients with keratoconus who underwent surgery for corneal ring implementation,the average corneal keratometry increased by 1 diopter during one year.The cause of corneal steepening is not examined in this study,although it is probable that the rings present within the cornea and its steepening are to blame for the drop in corneal keratometry.More research is needed in this area to pinpoint the precise impact of corneoscleral lenses on corneal keratometry in various keratoconus patient groups.

Figure 3 Differences in endothelial cell count before the initial fitting and after 3 and 6 months of corneoscleral lens wear in the patients.
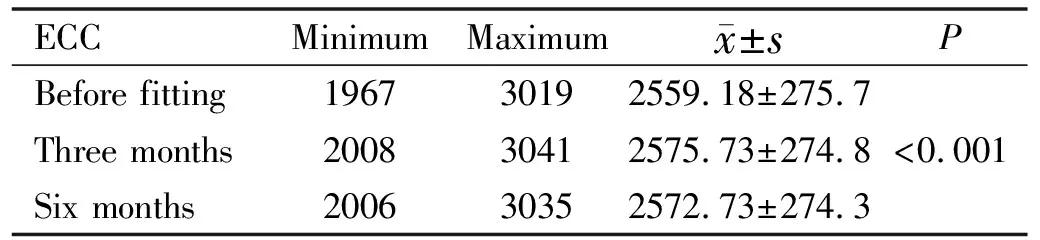
Table 4 Endothelial cell count before the initial fitting and after 3 and 6 months of corneoscleral lens wear in the patients cells/mm2
The central thickness of the cornea decreased statistically at 3 and 6 mo after using the contact lens,but this difference was not clinically significant.In a study conducted by Porcaretal[20],severe changes in the corneal central thickness were not reported and only a 5-μm decrease was observed.In another study by Montaltetal[19],keratoconus patients who underwent intraocular ring surgery experienced an average increase in corneal central thickness of four micrometers over the course of a year,in contrast to a previous study in which the average corneal central thickness decreased by only 4 micrometers after one year[17].In general,it seems that the use of corneoscleral lens does not have a significant effect on the corneal central thickness.In addition,because of progressive nature of the keratoconus,the reduction in corneal central thickness maybe due to progression of the disease.In fact,corneal thinning and cone-like protrusion of the cornea are considered as important morphological features of keratoconus.The eyes with keratoconus have thinner apical corneal epithelial thickness in comparison to the normal eyes.Total corneal thickness changes in keratoconus are associated with the changes in both epithelial and stromal thickness.In keratoconic eyes,the epithelium is known to thin over the cone and when the disorder progresses,there may be excessive epithelial thinning that can lead to a breakdown in the epithelium[22-24].
Although statistically the number of endothelium cells seems to have increased slightly after lens fitting,this could be due to the calculation of the device.As we know,it is considered that the increase in the number of corneal endothelium cells does not happen over time.In a study conducted by Porcaretal[20],no significant change was observed in the number of endothelial cells one year after the use of corneoscleral lenses.Furthermore,in two studies by Montaltetal[17,19],in two groups of patients with keratoconus and the patients with keratoconus who underwent intracorneal ring surgery,the number of corneal endothelium cells remained constant.It turns out that in the case of proper fit and correct use,corneoscleral lenses do not reduce the corneal endothelium cells count.
Few studies were conducted on the effectiveness of corneoscleral lenses in patients with keratoconus,in comparison to other forms of contact lenses.In this research,the number of analyzed samples is much more than in previous research on corneoscleral lenses that have been carried out[17,19-20].Based on the results of this study,and other studies that have been conducted in this field,if these lenses are properly fitted and used correctly,they will have good results and in terms of easier handling,high oxygen permeability and more tear circulation,it can be considered as an option in the vision correction of patients with keratoconus[17,19-20].The lack of a control group such and also wearing time of the contact lenses may be considered as limitations of this study.
In conclusion,it can be concluded that using the corneoscleral lenses significantly increases visual acuity,and due to the fact that corneal parameters were not changed noticeably during its use in patients with keratoconus,corneoscleral lenses are safe and can be used in this group of patients.