Deep insight into the B-cell associated tertiary lymphoid structure and tumor immunotherapy
Jilong Yang*, Jin Xu*, Haotian Liu, Wanyi Xiao, Gengpu Zhang
1Department of Bone and Soft Tissue Tumor, Tianjin Medical University Cancer Institute & Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, Tianjin’s Clinical Research Center for Cancer,Key Laboratory of Molecular Cancer Epidemiology, Tianjin 300060, China; 2Department of Anaesthesiology, Tianjin University Tianjin Hospital, Tianjin 300211, China
Bod et al.1recently published a study inNaturethat garnered attention to B cell- associated anti-tumor immunity and immunotherapy of melanoma and other tumors1.As a promising supplemental immunotherapy to mainstream methods that target T and natural killer (NK) cells, B cell-associated anti-tumor immunotherapy is promising, especially for patients who have failed treatment or are resistant to immune checkpoint inhibitors.Knowledge pertaining to B cell functions and associations with tertiary lymphoid structures (TLSs) requires further investigation to provide a thorough understanding of their roles in tumor immunity.The perspective herein focused on B cell roles in TLSs and associated anti-tumor activities to facilitate clinical application of this new treatment option.
Tumor-associated B cell types and functions
The roles of B cells in various stages and histologic types of malignancies are not fully understood.Some tumor- associated B cells may be indispensable allies of T cells in fighting cancer cells and are the main cell type in the initiation and maintenance of anti-tumor responses, especially in the form of TLSs1(Table 1).
Plasma cells
The role of plasma cells in tumor immunity is controversial.In high-grade ovarian cancer, CD20+ B, CD4+ T, CD8+ T,and plasma cell invasion is associated with better survival2.However, B cell-generated antibodies deposited at the tumor site can form immune complexes, activate receptorsviaFcγ,and recruit myeloid cells and macrophages.B cells also secrete pro-angiogenic factors and immunomodulatory cytokines,and thus accelerate tumor progression2.
Antigen-presenting B cells
B cells can act as antigen-presenting cells (APCs) and contribute to activating naive CD4 T cells.In lung cancer patients,activated B cells marked by CD69+HLA-DR+CD27+CD21+are associated with the CD4+ effector T cell response, indicating a catalytic role of antigen-presenting B cells in anti-tumor immune responses3,4.
Regulatory B cells (Bregs)
Bregs are a subpopulation of B cells with unique immunomodulatory and immunosuppressive properties.Bregs have an important role in peripheral tolerance2.Bregs inhibit dendritic cell (DC) differentiation, as well as Th1 and Th17 cell proliferation, and induce differentiation of Tregs by secreting IL-10.The secretion of IL-10 and TGF-β by Bregs inhibits CD8+ T cell activation, proliferation, and production of effectors, such as IFN-γ, TNF-α, and granzyme B, in cancer patients.Clearance of Bregs and elimination of inhibitory cytokines, such as IL-10 secreted by Bregs, are possible strategies against B cells2, but these strategies are in the early stages of investigation.
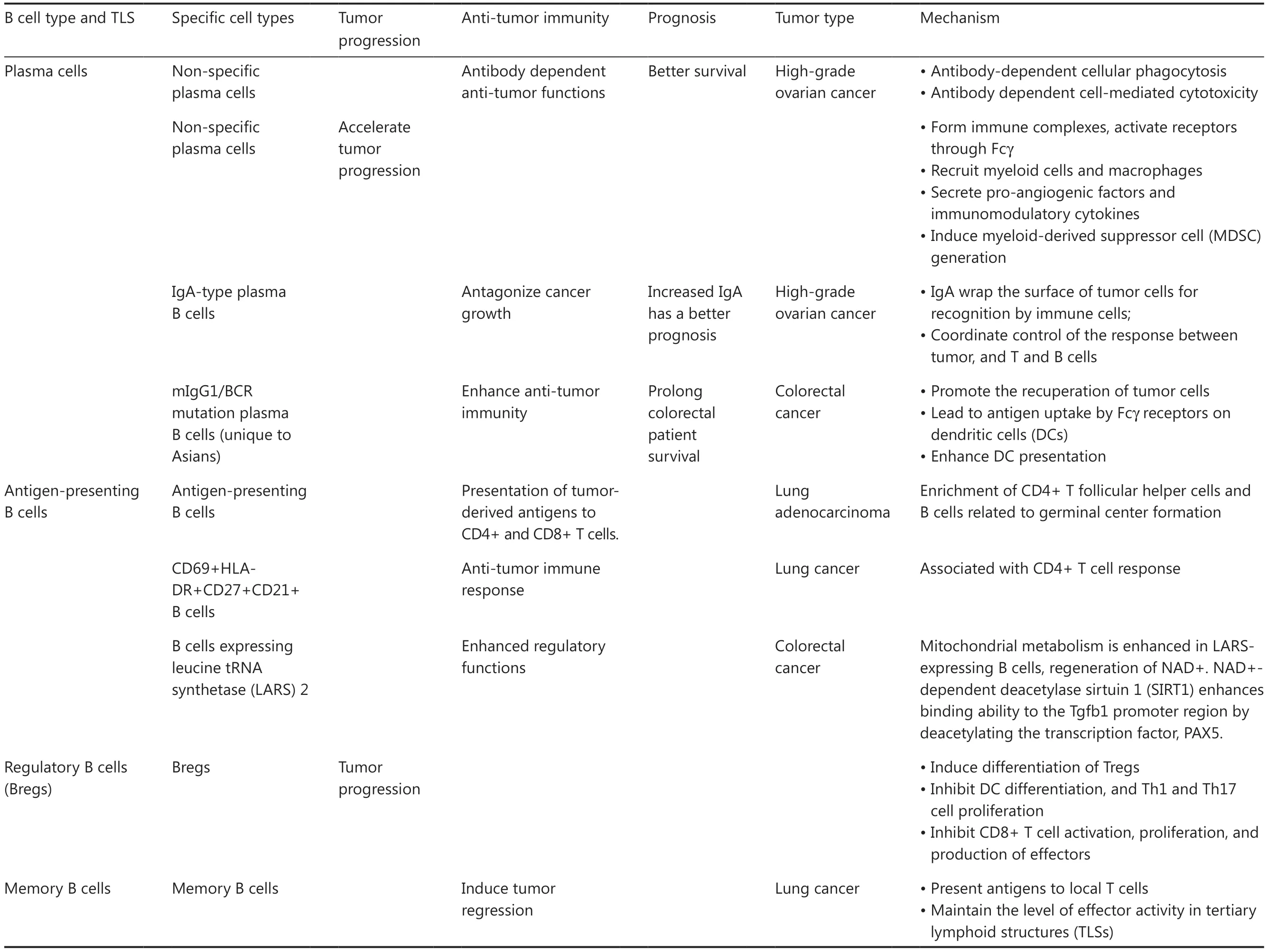
Table 1 Role of B cells and TLS in tumor immunity and immunotherapy

Table 1 Continued
Memory B cells
Memory B cells are a dynamic population of mature B cells that re-enter the germinal center and TLSs in response to persistent tumor antigens.Memory B cells present antigens to local T cells and cause tumor regression.This effect may be particularly important in TLSs, where T cells receive activation signals and maintain effector activity3,4.Of note,memory B cell function in lymphomas may be reversed.Entry of B cells into germinal centers is associated with acquisition of malignant features and is required for disease progression.Additionally, diffuse B cell lymphomas originate in abnormal memory B cells.
Tumor-infiltrating B cells
Tumor-infiltrating B cells scatter within tumors or cluster in well-structured mature TLSs, which suggests different functional statuses.As an important part of TLSs in tumor tissues,clustered infiltration and the number of B cells in TLSs are positively correlated with a good prognosis in the majority of tumor patients and predicts the response of patients to immune checkpoint inhibitor (ICI) treatment2,5.However,the infiltrated but scattered B cells easily release cytokines after interacting with other cell types in the tumor to inhibit T cell activity while promoting tumor growth.These B cells also provide nutrients for tumor cells by promoting neoangiogenesis,which facilitates tumor progression.
Controversial roles of B cells in tumor immunity
The role of B cells in tumor-associated immunity is controversial.B cells have differing roles during tumor stages.In an analysis of 69 studies, > 50% of the studies that included 19 tumor types concluded that tumor infiltration by B cells is associated with a positive prognosis compared to < 10% of studies that exhibited the opposite trend6.
Anti-tumor activity of B cells
Anti-tumor B cell functions mainly rely on the following methods.First, B cells present anti-tumor-associated antigens (TAAs) to CD4+ and CD8+ T cells.However, the specific underlying mechanism has not been elucidated.It was recently reported that in tumor antigen-specific B cells promote differentiation of tumor-specific CD4+ T follicular helper cells and control tumor growth in lung adenocarcinoma by secreting the cytokine, interleukin-21, thereby enhancing the CD8+ T cell response and producing granzyme B7.Second, tumor-infiltrating B cells exhibit antigen-driven clonal expansion, class switching, and affinity maturation in the cancer microenvironment to change the antigen targets and increase the inhibitory effect on cancer cells.In triple-negative breast cancer(TNBC), increased CD20+CD27+IgD- subtype-converted B cells upregulate the expression of BCR pathway molecules(FOS and JUN) and the germinal center chemokine regulator(RGS1), then activate CD69 and TNFα signalingviaNFκB8,9.Third, tumor- infiltrating B cells promote the recuperation of tumor cells, lead to antigen uptake by Fcγ receptors on DCs,and enhance DC presentation.In high-grade ovarian cancer,IgA produced by IgA type B cells wrap the surface of tumor cells for recognition by immune cells and coordinate control of the response between tumor, and T and B cells to antagonize ovarian cancer growth10.Patients with B cell infiltration and increased IgA had a better prognosis10.In a similar fashion, the mIgG1/BCR mutation, which is unique to Asians, enhances anti-tumor immunity and significantly prolongs colorectal cancer patient survival11.Fourth, tumor-infiltrating B cells activate complement- dependent cytotoxicity (CDC) to kill tumor cells12.A breast cancer study showed that a population of ICOSL+ B cells in TLSs after chemotherapy has an important role in anti-tumor immune responses, and the complement regulatory protein, CD55, regulates production of this cell population, which in turn determines whether tumor B cells have an immune-promoting or immunosuppressive role12.Fifth, tumor-infiltrating B cells exert anti-tumor effects mediated through antibody-dependent cellular phagocytosis (ADCP) and antibody dependent cell-m ediated cytotoxicity (ADCC).Sixth, tumor-infiltrating B cells secrete IFN-γ and IL-12 for cytotoxic immune responses, kill tumor cellsviagranzyme B and tumor necrosis factor-related apoptosisinducing ligand (TRAIL), and exert tumor-immunosuppressive effects through the tumor immune microenvironment and immunomodulation.
Roles of B cells in tumor progression
B cell infiltration is associated with a poor prognosis in patients with renal cancer and glioblastomas, suggesting that B cells promote tumor progression6.B cells produce IL-10, TGF-β,IL-35, IL-21, and TNF-β, thereby exerting a tumor-promoting effect by activating the complement cascade, differentiating into Bregs, and inhibiting CD8+ CTL and NK cell function.Moreover, B cells synthesize and secrete the neurotransmitter, GABA, which induces macrophages to secrete IL-1013.Furthermore, some antibodies produced by plasma B cells and the immune complexes formed by TAAs induce MDSC generation, which in turn inhibits anti-tumor immunity.
B cells in TLSs and the role in tumor immunotherapy
T-cell immunoglobulin mucin-1 (TIM-1) on the surface of B cells has an important role in B cell-mediated anti-tumor immunotherapy1.In the B16F10 melanoma model, conditional knockout of other co-inhibitory molecules, such as PD-1, TIM-3, TIGIT, and LAG-3 on B cells, has little effect on tumor burden, whereas selective knockout of Havcr1, which encodes TIM-1, effectively inhibits tumor growth and enhances effector T cell actions.Therefore, inhibition of TIM-1 on B cells enhances the T cell response and promotes the anti-tumor immune response1.This B cell-associated anti-tumor immunotherapy has great prospects, especially for patients who have failed treatment or are resistant to T cell-specific ICIs.Furthermore, B cells and associated TLSs might also have important value in anti-tumor immunotherapy (Table 1).
B cell infiltration and TLS formation
B cells also have important roles in the establishment of TLSs and anti-tumor immunity14-16.A TLS is usually composed of B cells forming the internal core, T cells wrapping the B cell region, and B and T cells forming the main structure17.The likelihood of T follicular helper (Tfh) cells among T cells is relatively high, but Th1 cells, cytotoxic CD8+ T cells, or Tregs may also be present.TLSs also contain other cell populations,such as DCs, including CD21+ FDCs, which are essential for germinal center formation and B cell affinity maturation, and CD83+ DCs (DC-LAMP+ DCs), which are mainly localized in the T cell region.Additionally, CD68+ macrophages in a TLS might have a role in clearing apoptotic cells.In addition to the above cellular components, a large number of stromal cells act similar to follicular reticular cells in secondary lymphoid tissues by anchoring TLSs to chronic inflammatory sites.Furthermore, high endothelial venules provide a route for lymphocytes to enter a TLS17.By analyzing a large number of clinical cohort samples, it was shown that B cell infiltration and TLS formation are positively correlated to the response to immunotherapy.Specifically, immunotherapy is more effective when TLSs in tumor tissue show B cell-forming clumps14,16,18,19.
TLS formation, maturation, and anti-tumor immunotherapy
Given that the presence of a TLS is associated with a positive prognosis for many tumors, researchers have induced the formation of TLSs by locally expressing TLS-associated cytokines or chemokines in tissues.For example, stimulator for interferon gene (STING) agonist promotes normalization of tumor blood vessels, which leads to TLS formation.Oncolytic viral therapies may have a similar role in promoting cytokines and chemokines, favoring recruitment of all participants interacting in mature TLSs with the advantage of enhancing antigen proliferation.TNF-α of the LIGHT family [tumor necrosis factor superfamily member 14 (TNFSF 14)] also promotes TLS formation when efficiently delivered to tumor blood vessels using vascular targeting peptides.Immune checkpoint blockade therapy also induces TLS formation in tumors.T cell genetic engineering enhances Tfh cell differentiation, leading to the production of TLSs in nearly all tumors, which is associated with a significant delay in tumor progression.These results suggest that TLS formation can be utilized as an immunotherapy strategy.
An important factor leading to TLS assembly, or at least a strategy to form TLSs, involves the differentiation of activated CD4+ T cells into Tfh cells.In an ovarian cancer model, Tfh cells produce a chemokine environment that promotes spontaneous assembly of TLSs, including secretion of LIGHT and production of IL-21, which activate B cells in response to CXCL13 produced by Tfh cells.Independent studies in preclinical models of colorectal cancer confirmed the critical role of Tfh cells in TLS.There may be various ways to coordinate these lymphoid structures, but the roles of CXCL13 and Tfh cells appear to be particularly important, at least in terms of germinal center formation and maintenance.The discovery and in-depth study of TLSs have led to deeper insight into anti-tumor immunity and may provide a knowledge base by which to develop new and more effective tumor immunotherapies17,20.
Unresolved issues involving TLSs in tumors
Some urgent issues need to be resolved in the current research on TLSs.The first issue is the lack of TLS markers.Most studies have used different molecular panels to define and describe TLSs, and more efficient and simple methods are needed to evaluate TLSs.Second, our understanding of the cellular and molecular processes that drive TLS formation was derived from models of autoimmune diseases and chronic infections.An understanding of TLS formation in tumors is lacking.The third issue is how mature TLSs form.TLS development undergoes continuous stages of maturity and is divided into early, primary, and secondary, of which secondary TLSs are mature.The fourth issue is the heterogeneity of TLSs14,16,18.TLSs have significant heterogeneity within a cancer type, as well as within cancer lineages.For example, in a breast cancer study, TLSs were not detected in brain metastases.In melanoma, the maturity of the TLS varies among regions, and TLSs in germinal centers are the most mature.In a sarcoma study, TLSs were classified as early, primary, or secondary follicular TLSs because of significant heterogeneity, of which 61% were early TLSs18,19.Fifth, the TLS itself has various types.Tissue-specific expression of CXCL13 induces aggregation of B cells lacking an FDC network.Expression of TNF and CXCL12 induces a TLS with B cells mainly supplemented by a small number of T cells and DCs.CCL19 and CCL21 induce aggregates of similar composition, whereas CCL21 induces large structures17.
Future perspectives
It is likely that analysis of tumor tissue components, especially B cells and their associated TLSs after tumor resection in patients, can be used to quantitatively predict the efficacy of further immune checkpoint therapy and develop new immunotherapies.Such biomarkers are simpler, more economical,and more feasible than analyzing the tumor cell mutation burden.Another attractive strategy is B cell activation for TLS formation and maturation.Research focusing on TLS inductionviacomplex technologies, including novel biomaterials,STING, oncolytic viral therapies, TNF-α, immune checkpoint blockade therapy, and T cell genetic engineering, is ongoing and preclinical models have achieved promising preliminary results.Although these findings fall short of the reproducibility and robustness needed to enter mainstream cancer treatment, existing data have highlighted B cells and their roles in TLSs and associated anti-tumor activities to facilitate clinical development of new effective treatment options.
Acknowledgements
We thank Mitchell Arico from Liwen Bianji [Edanz (https://www.liwenbianji.cn)] for editing the language of a draft of this manuscript.
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the perspective: Jilong Yang.Drafted the manuscript: Jin Xu and Jilong Yang.Revised the manuscript: Jilong Yang, Jin Xu, Haotian Liu,Wanyi Xiao, and Gengpu Zhang.
 Cancer Biology & Medicine2024年2期
Cancer Biology & Medicine2024年2期
- Cancer Biology & Medicine的其它文章
- DNA methylation profiles in cancer: functions, therapy,and beyond
- From dichotomy to diversity: deciphering the multifaceted roles of tumor-associated macrophages in cancer progression and therapy
- Perspective on new cell-free DNA technologies for early cancer detection
- Bile acids, gut microbiota, and therapeutic insights in hepatocellular carcinoma
- Cancer-educated neutrophils promote lung cancer progression via PARP-1-ALOX5-mediated MMP-9 expression
- First-line immunotherapy for advanced non-small cell lung cancer: current progress and future prospects
