Systematic review of diagnostic tools for peritoneal metastasis in gastric cancer-staging laparoscopy and its alternatives
Si Ying Adelina Ho,Kon Voi Tay
Abstract BACKGROUND Gastric cancer is one of the leading causes of cancer burden and mortality,often resulting in peritoneal metastasis in advanced stages with negative survival outcomes.Staging laparoscopy has become standard practice for suspected cases before a definitive gastrectomy or palliation.This systematic review aims to compare the efficacy of other diagnostic modalities instead of staging laparoscopy as the alternatives are able to reduce cost and invasive staging procedures.Recently,a radiomic model based on computed tomography and positron emission tomography (PET) has also emerged as another method to predict peritoneal metastasis.AIM To determine if the efficacy of computed tomography,magnetic resonance imaging and PET is comparable with staging laparoscopy.METHODS Articles comparing computed tomography,PET,magnetic resonance imaging,and radiomic models based on computed tomography and PET to staging laparoscopies were filtered out from the Cochrane Library,EMBASE,PubMed,Web of Science,and Reference Citations Analysis (https://www.referencecitationanalysis.com/).In the search for studies comparing computed tomography (CT) to staging laparoscopy,five retrospective studies and three prospective studies were found.Similarly,five retrospective studies and two prospective studies were also included for papers comparing CT to PET scans.Only one retrospective study and one prospective study were found to be suitable for papers comparing CT to magnetic resonance imaging scans.RESULTS Staging laparoscopy outperformed computed tomography in all measured aspects,namely sensitivity,specificity,positive predictive value and negative predictive value.Magnetic resonance imaging and PET produced mixed results,with the former shown to be only marginally better than computed tomography.CT performed slightly better than PET in most measured domains,except in specificity and true negative rates.We speculate that this may be due to the limited F-fluorodeoxyglucose uptake in small peritoneal metastases and in linitis plastica.Radiomic modelling,in its current state,shows promise as an alternative for predicting peritoneal metastases.With further research,deep learning and radiomic modelling can be refined and potentially applied as a preoperative diagnostic tool to reduce the need for invasive staging laparoscopy.CONCLUSION Staging laparoscopy was superior in all measured aspects.However,associated risks and costs must be considered.Refinements in radiomic modelling are necessary to establish it as a reliable screening technique.
Key Words: Gastric cancer;Peritoneal metastases;Computed tomography;Positron emission tomography;Magnetic resonance imaging;Staging laparoscopy
INTRODUCTION
Gastric cancer is the fifth most common malignancy worldwide,the most common malignancy in many South-Central Asian countries and the fourth most common cause of cancer-related deaths,according to GLOBOCAN 2020 data[1].Peritoneal carcinomatosis is the most common[2-4] type of metastasis secondary to gastric cancer,and its presence is associated with a higher risk of mortality,disease progression and poorer survival rates[4-6].Currently,computed tomography (CT) scans and staging laparoscopy are the two most commonly utilised modalities for detecting peritoneal metastases[7,8].This is attributed to CT scans having high rates of sensitivity and specificity,short scanning time,as compared to other imaging modalities such as positron emission tomography (PET) and magnetic resonance imaging(MRI)[9-11].This review aims to investigate the efficacy of multi-imaging modalities in detecting peritoneal metastasis prior to management planning and during surveillance to detect disease recurrence.
The identification of peritoneal carcinomatosis is difficult as its presentation is commonly asymptomatic and hence,discovered late[12].The detection of peritoneal metastasis on CT is dependent on visualising unique features such as ascites,omental caking and peritoneal thickening[13],but smaller deposits (< 5 mm) such as peritoneal nodules may be missed on imaging[14].To rule out peritoneal metastasis prior to oncological gastrectomy,staging laparoscopy is commonly performed,especially in advanced gastric cancer patients.In this systematic review,we aim to investigate current evidence to determine if CT scans can yield comparable detection rates of peritoneal metastasis secondary to gastric cancer,with the goal of reducing the routine practice of staging laparoscopy.
PET and MRI scans are valuable non-invasive imaging techniques that are often used as alternatives to CT scans.PET scans detect cancer dissemination by mapping radioactive tracers,usually F-fluorodeoxyglucose (FDG)[15].They are frequently used in oncological staging in primaries such as lymphoma and lung cancer[16],due to the high metabolic rate of these malignancies,which tend to have increased uptake of the tracers[15].However,it is important to note that PET scans may not be as suitable for malignancies with low avidity for FDG,and infective or inflammatory sites may be mistaken for malignancies[17].Since up to 90% of primary gastric malignancies have significant FDG uptake visible on PET[18],excluding patients with tumours of low FDG avid signet ring cells histology[19],we intend to find out if PET scans can be a useful modality in the diagnosis of peritoneal metastases.
As for MRI scans,its main advantage lies in its superior sensitivity,which provides better soft tissue definition,particularly when coupled with non-radioactive contrast[20].Disadvantages to using MRI include its inability to be used in patients with magnetic implants,allergy to gadolinium,its high cost,longer scanning duration and high rate of motion artifacts[21-23].Hence,we also evaluated the efficacy of PET and MRI scans as an alternative to CT scans in the detection of peritoneal metastasis secondary to gastric cancer.Although other forms of diagnostic modalities,such as ultrasound scanning,have been considered,it has proven to be inferior in sensitivity and specificity for the detection of peritoneal metastases.This has been attributed to the acoustic impedance of gas and fat,which decreases visualisation through bowel,omentum,mesentery and adipose tissues[7,24].Endoscopic ultrasound has shown to be a valuable tool in predicting the T stage of tumours and local invasion.However,its efficacy in detecting distant peritoneal metastasis remains limited.Recent animal studies conducted in 2022 have shown promising results in imaging and scoring peritoneal metastasis,but this is still in the trial phase and requires further validation.
The use of PET/MRI scans have also gained attention in recent years as it has shown better detection of peritoneal metastasis secondary to primary abdominopelvic malignancies compared to PET/CT.A recent systematic review demonstrated that PET/MRI scans exhibited better sensitivity for detecting peritoneal metastasis in gastric cancer than PET/CT scans.However,this systematic review was limited to five papers,each assessing a small cohort of 10-15 patients,thereby making it difficult to draw definitive conclusions regarding the efficacy of peritoneal metastasis detection until further studies are conducted.
In recent years,there has been a growing interest in the use of big data and artificial intelligence,to develop radiomic models that can accurately predict peritoneal metastasis based on preoperative CT and PET scans[25].These models may also have the potential to prognosticate and estimate recurrence rates based on deep learning of retrospective cohorts[26].As such,we have also included radiomic analysis in our search strategy in order to see the latest development in the diagnosis of peritoneal metastases.
In this paper,we investigate whether there are non-invasive alternatives that can provide comparable accuracy to the current standard of peritoneal metastases detection,staging laparoscopy.This is an important question,as staging laparoscopy is an invasive procedure that carries risks for patients.Identifying non-invasive alternatives that are equally effective would represent a significant advance in the field of peritoneal metastases detection and could improve patients’management and safety outcomes.
MATERIALS AND METHODS
Search strategy
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.The Cochrane Library,EMBASE,PubMed,Web of Science libraries andReference Citations Analysis(https://www.referencecitationanalysis.com/) were searched using the following search terms: Stomach neoplasms,gastric cancer,peritoneal neoplasms,peritoneal metastasis,peritoneal carcinomatosis,laparoscopy,CT,PET,and MRI.The respective search terms are detailed in the appendix as Supplementary Tables 1 and 2.After reviewing the references in the reports and articles for CT and staging laparoscopy,no additional relevant studies were identified.
Studies were considered in the review if they met the inclusion criteria: (1) Prospective or retrospective comparative papers;(2) Diagnosis of peritoneal metastases secondary to gastric cancer;and (3) Compared CT against PET or MRI or staging laparoscopy.
Studies were excluded if the following were met: (1) Articles were not in English;(2) Articles were case reports,guidelines,letters,non-comparative studies,protocols;or meta-analyses;(3) Patients were already diagnosed with metastatic disease;(4) Diagnostic modality used was none of laparoscopy,CT,PET nor MRI;and (5) Comparison was not made for peritoneal metastases.
Quality assessment
The risk of bias was assessed as low,moderate,or high based on the Newcastle-Ottawa scale (NOS)[27] for nonrandomised studies based on cohort selection,comparability,and outcomes.All 17 studies were determined to be of low risk of bias as they all scored a seven on the NOS.Two points were lost as the studies did not standardise the age and sex of the cohort involved,and some subjects were lost to follow-up in the study by Burbidgeet al[28],while the other nine had no clear description of follow-up rates.
Data collection:The following data were extracted from the included studies: (1) Patient demographics;(2) Tumour characteristics;(3) The specific type of diagnostic modality used;and (4) Statistical outcomes in the detection of peritoneal carcinomatosis.
RESULTS
CT vs staging laparoscopy
Figure 1 shows the flow chart for the article selection process.Eight relevant articles for CT and staging laparoscopy were identified and included for review.Search details are reflected in Supplementary Table 1.

Figure 1 Flowchart for the selection of articles comparing computed tomography to staging laparoscopy in this systematic review.
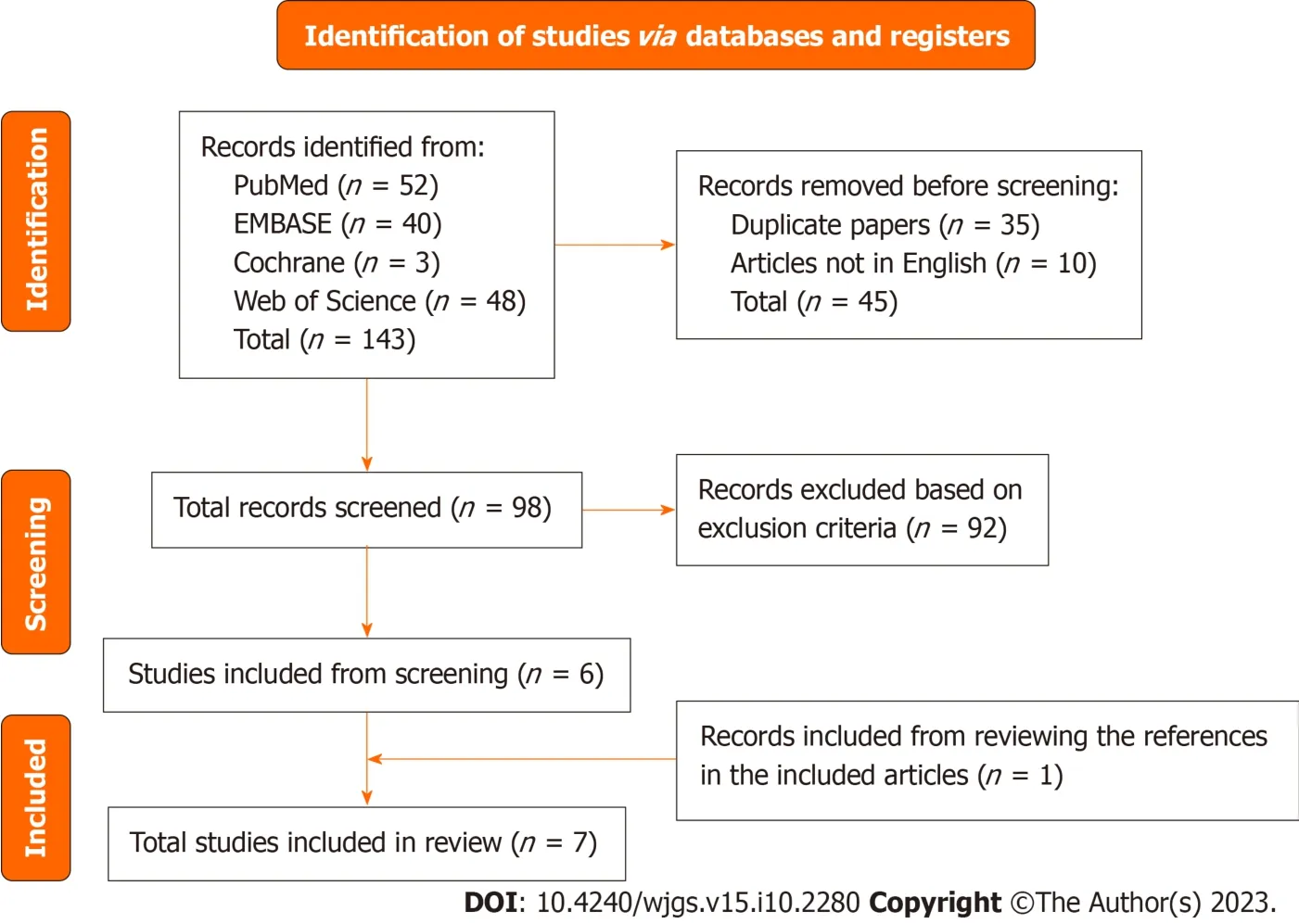
Figure 2 Flowchart for the selection of articles comparing computed tomography to positron emission tomography in this systematic review.
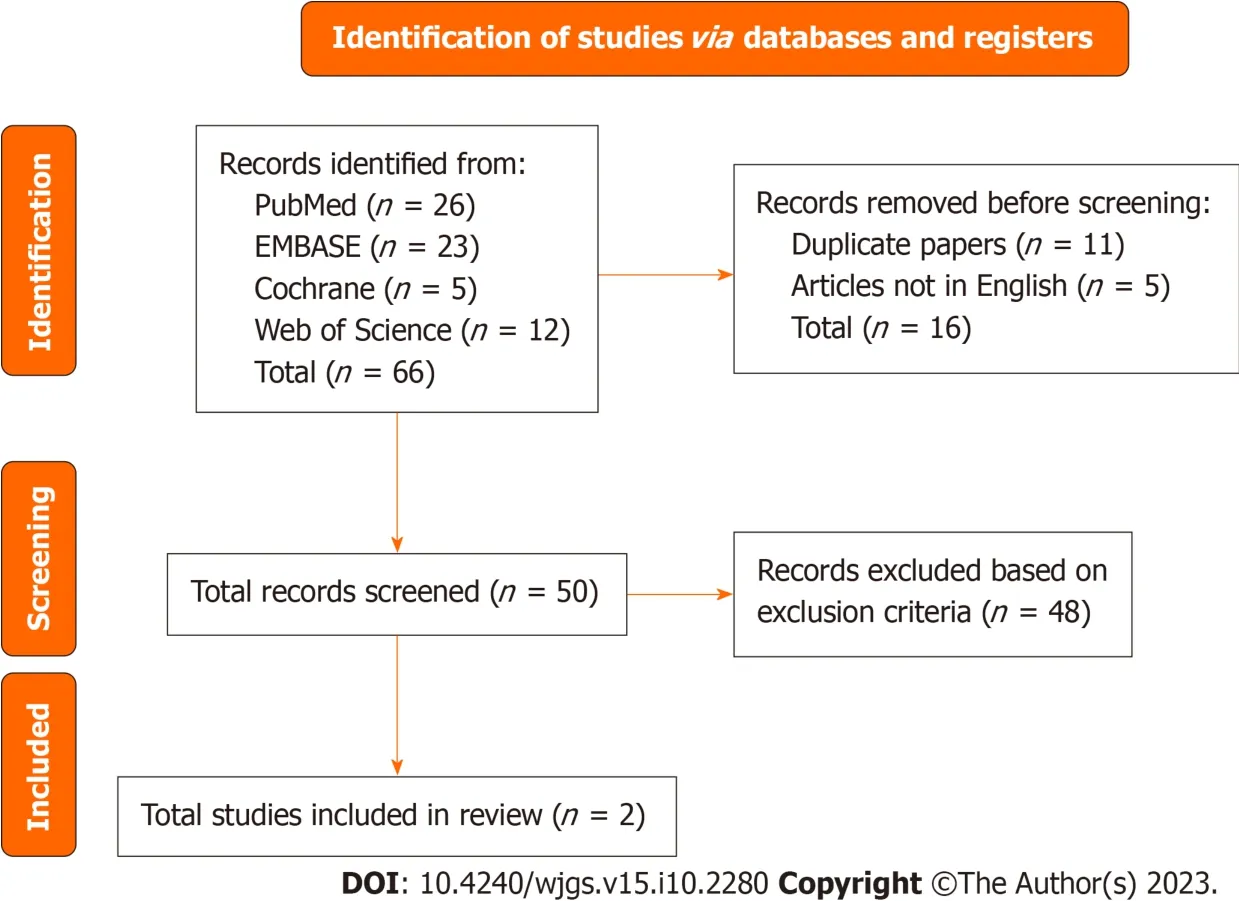
Figure 3 Flowchart for the selection of articles comparing computed tomography to magnetic resonance imaging in this systematic review.
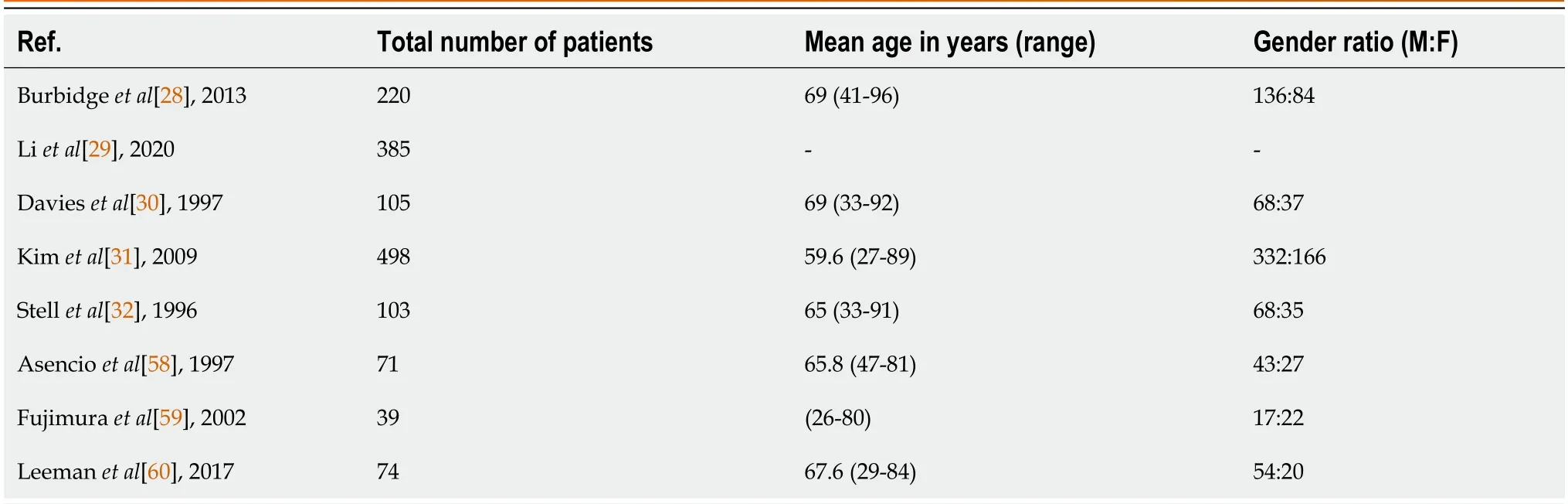
Table 1 Patient demographics
A total of five retrospective studies and three prospective studies were included.A summary of the patient demographics (Table 1),tumour characteristics and type of CT used (Table 2) and outcome parameters (Table 3) are included below.
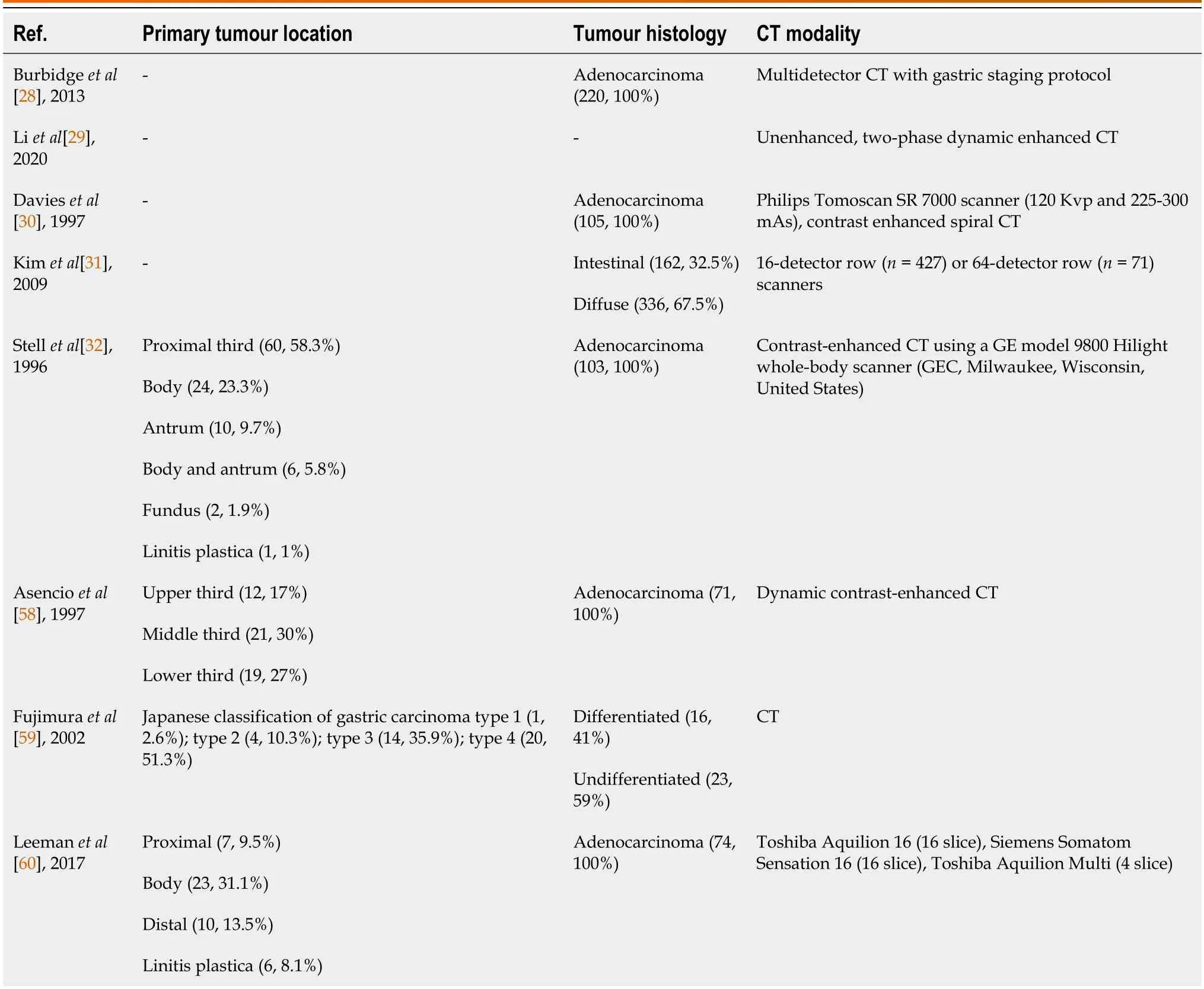
Table 2 Tumour characteristics and computed tomography modality used
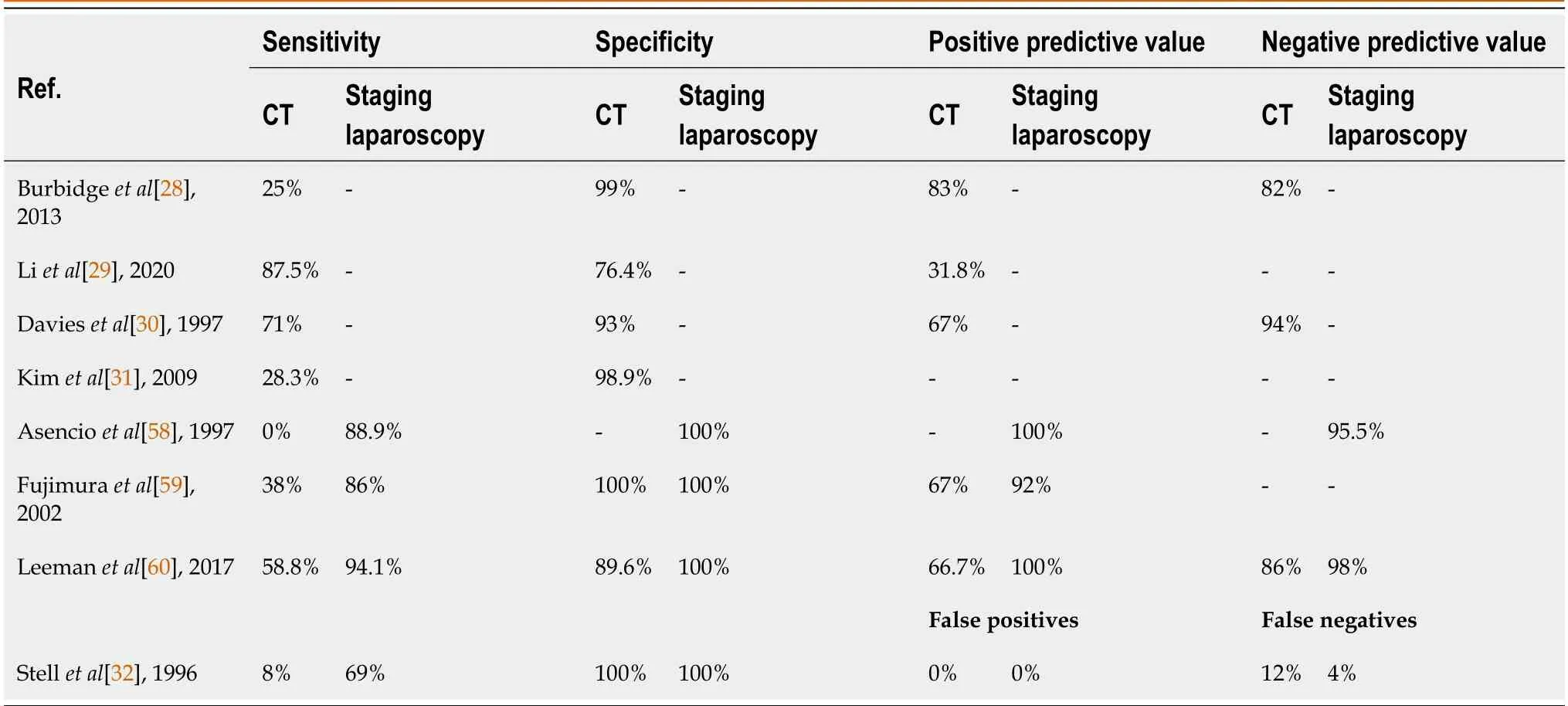
Table 3 Statistical results of computed tomography and staging laparoscopy
A total of 1495 patients with synchronous peritoneal metastases were included in the studies.Excluding the participants from Liet al[29] as the gender proportion was not provided,718 (64.7%) were male and 391 (35.2%) were female.The age distributions of the participants are also described in Table 1.
The details of the distribution and histological subtypes of the tumours are listed in Table 2,along with the type of CT scanner used.The findings of the study indicate that the source of the primary tumour does not exhibit any discernible pattern,although the histological subtype of lesion typically presents as an adenocarcinoma.The anatomical distribution of the primary lesion was not listed by Burbidgeet al[28],Davieset al[30],Kimet al[31] and Liet al[29] Histologicalsubtypes were not mentioned by Liet al[29].
Among the studies that compared the sensitivities of both CT and laparoscopy,staging laparoscopy consistently yielded better results at an average of 58.3%.Staging laparoscopy also demonstrated an average of 3.5% better specificity compared to CT in all studies that compared the two.Similarly,staging laparoscopy exhibited better positive and negative predictive values,with an average improvement of 29.2% and 12% respectively.Stellet al[32] reported false positive and false negative rates instead,in which staging laparoscopy had less or equal numbers of incorrect reporting.This study did not note any false positives,and CT reported an average of 8% more false negatives.In the papers by Burbidgeet al[28],Davieset al[30],Kimet al[31] and Liet al[29],statistics for staging laparoscopy were not provided as laparoscopy was used to confirm the provisional diagnosis derived from CT scanning.
CT vs PET or MRI
Following this discovery,we proceeded to evaluate whether PET or MRI scans are accurate enough to be used as alternatives to CT scans for the purpose of minimising the need for invasiveness of staging laparoscopy,while simultaneously maintaining high detection rates.
Figures 2 and 3 show the flow chart for the article selection process.Seven relevant articles comparing CT to PET and two articles comparing CT to MRI were identified and included for review.Search details are reflected in Supplementary Table 2.
A total of five retrospective studies and two prospective studies were included for CTvsPET scans.One retrospective and one prospective study were included for CTvsMRI scans.A summary of the patient demographics (Table 4),tumour characteristics and type of CT used (Table 5),and outcome parameters (Tables 6 and 7) are included below.Following the review of the references in the reports and articles available,the study by Simet al[33] was also included.
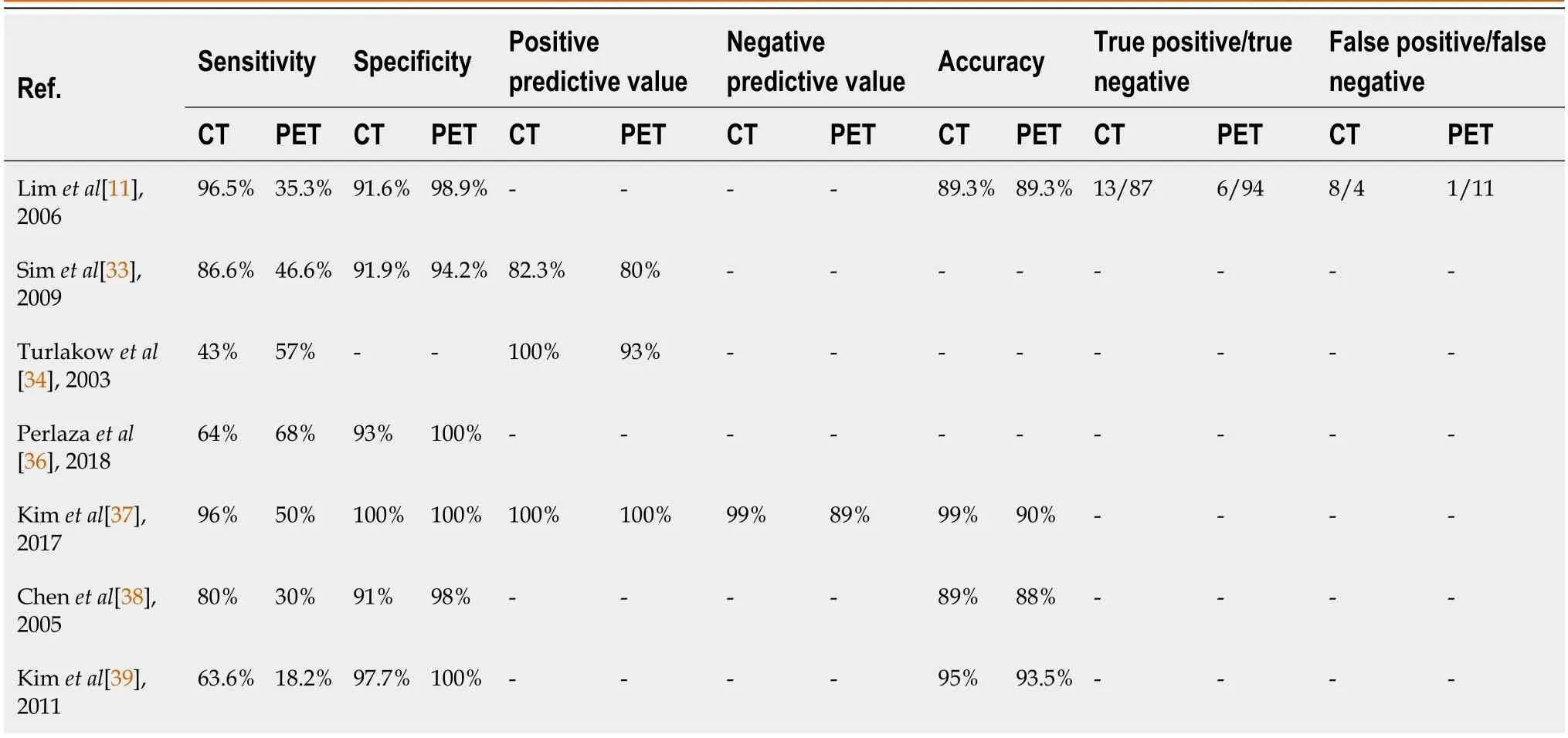
Table 6 Statistical results of computed tomography and positron emission tomography
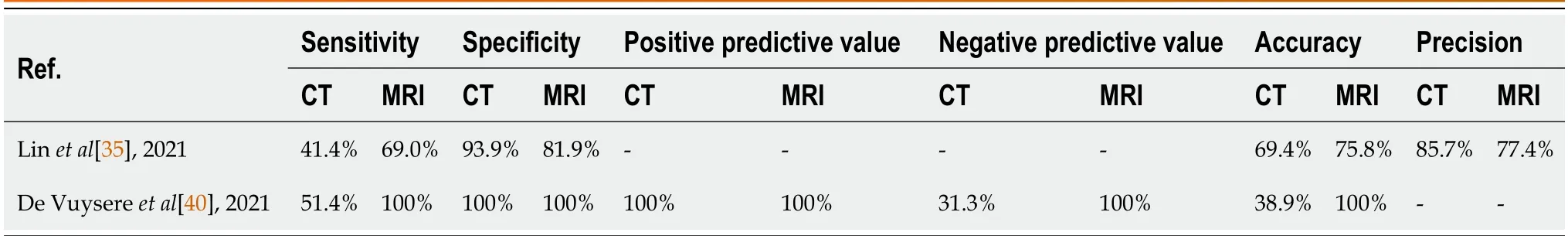
Table 7 Statistical results of computed tomography and magnetic resonance imaging
A total of 474 and 94 patients with metachronous peritoneal metastases identified by CT or PET and CT or MRI respectively were included in the studies.A total of 288 (60.8%) were male and 186 (39.2%) were female in the CTvsPET group.In the CTvsMRI group,42 (44.7%) patients were male and 52 (55.3%) were female.The age distributions of the participants are also described in Table 4.
The origin of the primary tumour in these two populations also does not seem to exhibit a discernable pattern but among the studies that have reported histology,the histological subtype of the lesion is typically an adenocarcinoma.The details of the distribution and histological subtypes of the tumours are listed in Table 5,along with the type of CT,PET or MRI scanner used.The studies by Turlakowet al[34] and Linet al[35] did not specify the histology of gastric cancer in their patients.
The sensitivity of CT seems to be superior to PET in all studies except in Perlazaet al[36] and Turlakowet al[34].Conversely,the specificity of PET is superior to CT in every study except in Kimet al[37],where both had 100%specificity.This parameter was not measured by Turlakowet al[34].Positive predictive value (PPV) was only calculated by Kimet al[37],Simet al[33] and Turlakowet al[34] where CT slightly outperformed PET by an average of 3.1%.Negative predictive value (NPV) was only reported by Kimet al[37] where CT was better than PET by 10%.The accuracy of CT was also marginally greater than or equal to PET in the studies by Chenet al[38],Kimet al[39],Kimet al[37] and Limet al[11]by an average of 2.875%.True positive,true negative,false positive,false negative values were only reported by Limet al[11],where CT was better at picking up true positive cases (13vs6) and had lower false negative rates (4vs11).PET was better than CT at picking up true negative cases (87vs94) and had lower false positive rates (8vs1).
The values obtained by Linet al[35] were the calculated average value between the two types of CT and MRI scanners used.The decimal values in Linet al[35] were converted to percentages in the calculation of average scores.
The sensitivity of MRI was superior to CT in both papers by an average of 38.1%.Conversely,CT had better or equal specificity than MRI by an average of 6%.In the study by De Vuysereet al[40],PPV was equally high at 100% but MRI had much greater NPV at 68.7% better.MRI also had better accuracy by an average of 33.75%.Precision was only reported by Linet al[35],where CT was 8.3% better.Iodinated contrast (Telebrix,Xenetix,Omnipaque) were used in both studies,and T2-weighted,diffusion-weighted images were obtained.
Radiomic modelling is a cutting-edge technique that employs artificial intelligence and a quantitative approach to augment medical imaging data,thereby improving diagnostic accuracy.The use of radiomic analysis and deep learning is gaining traction in the diagnosis of peritoneal metastases,with several preliminary papers demonstrating its potential.However,there is currently a lack of comparative studies that evaluate the efficacy of radiomic models.In the study by Jianget al[14],the performance of radiomics was significantly better than conventional clinicopathological factors [Area under the curve (AUC) range,0.51-0.63].It also had value as an independent predictor of occult peritoneal metastases.In a separate paper by Jianget al[41],radiomic modelling was able to predict peritoneal recurrence (AUC: 0.857,0.856 and 0.843) and disease-free survival independently in all three cohorts stated (C-index 0.654,0.668 and 0.610).The paper by Huanget al[26] affirms this possibility as radiomic modelling has been demonstrated to be an independent predictor of peritoneal metastases,with AUC values of 0.751,0.802 and 0.745.Xueet al[42] have reported promising performance with the radiomic model,achieving an AUC of 0.90 in the training cohort and 0.88 in the validation cohort respectively.Ultimately,radiomic modelling is still in a developmental phase,requiring the multidisciplinary coordination of physicians,computers and data scientists in order to interpret the imaging data and analysis.
DISCUSSION
The mean age of participants falls between 58 to 69 years,which is in line with the peak age where gastric cancer and peritoneal metastasis are reported[2,43].Most of the participants in the studies were male,except in those by Fujimuraet al[59],Kimet al[37] and Linet al[35],which is converse to current literature.In the 2021 systematic review by Rijkenet al[44],peritoneal metastases were noted more frequently in females.Tanet al[45] also reported similar findings in their retrospective review[45].
Although the location of the primary tumour in the studies included did not show any distinct distribution pattern,most of the lesions arise from non-cardia areas,which corresponds to literature by Rijkenet al[44] and Sanjeevaiahet al[46] It is frequently reported that signet ring cell or diffuse type tumours have a greater risk of peritoneal metastases but the majority of cases seen in the studies are adenocarcinomas[44,47,48].This may be attributed to the vast majority of gastric cancers being adenocarcinomas or intestinal types[49,50].
The use of staging laparoscopy has demonstrated superior or comparable results to CT scans in all domains of measurement,namely sensitivity,specificity,PPV,NPV,false negative and false positive rates.These findings are consistent with current research indicating that staging laparoscopy more accurately reflects the actual M stage of patients,leading to a significant reduction in unnecessary laparotomies[51].A systematic review by Gigeret al[51]suggested the number of diagnostic laparotomies performed can be lowered by up to 63% by performing staging laparotomy prior.
However,the risks of staging laparoscopy were not properly assessed in the studies.The most significant risk appeared to be port-site metastasis as seen in the five cases reported by Shoupet al[52],one case by McCullochet al[53]and one case by Davieset al[54] Despite these findings,all three papers suggest that the value of diagnostic laparoscopy far outweighs the risks,and such occurrences are rare and unlikely.
The results from comparing between CT and PET scans were not as clear cut.CT scans performed marginally better than PET scans in most aspects,namely sensitivity,PPV,NPV,accuracy,and the detection of true positive cases with lower false negative rates.However,PET scans offered slightly better specificity and greater identification of true negative cases with lower false positive rates.These findings are consistent with the study by Dromainet al[55],which found that PET scans did not perform as well as CT scans in detecting peritoneal metastases in gastrointestinal malignancies.The limited FDG uptake due to the small (< 2 mm) and even microscopic size of peritoneal metastasis could be a contributing factor to this discrepancy[55].
MRI scans had outperformed or performed equally well to CT scans in all areas of comparison except when comparing specificity and precision,where CT scans were superior.This includes sensitivity,PPV,NPV and accuracy.Similar results were also reported by Lowet al[22],where MRI scans were found to be more successful than CT scans in detecting peritoneal metastasis in all cases of low,moderate and large tumour burden.However,it should be noted that the significant downsides of using MRI scans include the high cost and time necessary for the procedure,along with the motion artefacts that can compromise image quality.
The use of PET/MRI has become increasingly prevalent and has demonstrated its effectiveness in detecting peritoneal metastasis.The degree of peritoneal involvement is a crucial factor in determining the resectability and prognosis of the tumor.However,the detection rate of 18-fluorothymine-FDG in peritoneal metastasis is often poor due to its low level of FDG uptake,leading to potential underestimation of the degree of involvement.In a recent study by Wanget al[3,9],[68Ga]Ga-FAPI-04 PET MRI/CT was found to be 100% sensitive in detecting peritoneal metastasis in gastric cancer.This success may be attributed to the fibrotic reaction of tumor cells invading the peritoneum,and the targeting of fibroblast activating protein (FAP) by FAPI.By improving the detection rate of peritoneal metastasis,clinicians can more accurately assess disease involvement and evaluate treatment response.
In the same vein,recent advances in PET radiotracers have shown promise in addressing the limitations of imaging FDG non-avid tumours,such as early stage,diffuse type,and mucinous tumours.Some examples of novel PET radiotracers that have shown potential in this regard include 18-fluorothymine,FAPI,and DOTA-FAPI PET.Further research is needed to fully understand the potential of these radiotracers,but early results are encouraging.
The use of radiomic modelling has also emerged as a potential tool for diagnosing peritoneal metastasis with the aid of CT and PET scanning,as shown by the papers by Jianget al[14,41],Huanget al[26],and Xueet al[42].Chenet al[25] also reported encouraging results in their preliminary evaluation of radiomics in the use of non-invasive peritoneal metastases diagnosis by studying three types (R_IU model for iodine uptake images,R_MIX model for mixed images,R_comb model for the combined radiomics model) of radiomics models in dual-energy CT scanning.The retrospective paper by Kimet al[56] has further shown the possibility of using texture analysis and entropy in CT scans to detect occult peritoneal metastases.When the cut-off value for entropy was applied,the sensitivity and specificity were found to be 80% and 90%respectively.With further research,deep learning and radiomic modelling can be refined and potentially applied as a preoperative diagnostic modality,thereby reducing the need for invasive staging laparoscopy.
Limitations
The lack of homogeneity in the methodology of studies included in the review is a key concern that could have contributed to some disparity as different types of data were reported.For instance,while the paper by Stellet al[32]reported false negative and false positive rates,other papers reported PPV and NPV instead.Additionally,papers by Burbidgeet al[28],Davieset al[30],Kimet al[31] and Liet al[29],did not report the statistical values representing staging laparoscopies,as they utilized laparoscopy to confirm the preoperative diagnosis made by CT scans,basing the statistical values reported for CT scans on laparoscopy.This implied that staging laparoscopy was assumed to have maximum accuracy and remained the standard of care prior to definitive gastrectomy based on features such as poorly differentiated adenocarcinoma on histology,linitis plastica,large sized type 3,or equivocal CT findings for peritoneal dissemination[57].However,it is important to acknowledge that heterogeneity among studies is a common occurrence,particularly when papers are produced by various institutions that adhere to different reporting guidelines and compare different methods of diagnostic tools.
The type of CT,PET and MRI scanners used also varied from study to study.With different types of scanners used,the cut of the images obtained will also vary,potentially affecting the accuracy.The quality of images obtained will also vary,which could result in inconsistencies in the level of human error when reading the scans.
Similarly,the staging laparoscopy procedures were performed by different surgeons with differing levels of competency and proficiency with the laparoscope.This difference in ability could have altered the accuracy rates yielded as well.However,considering that many of the statistics obtained from the papers are 100%,the margin of error in this aspect appears to be limited.
Included reviews comparing MRI and CT scans were only limited to two studies by Linet al[35] and De Vuysereet al[40],reducing the quality of analysis obtained due to a small sample size.Some of the statistics obtained were nonoverlapping,which impacted the data analysis,resulting in a less robust comparison.Additionally,the study by Linet al[35] was not specific for gastric cancer.This is a clear indication for further studies specifically comparing MRI and CT scans in the detection of peritoneal metastases secondary to gastric cancer.Several studies evaluating the use of PET/MRI in detecting peritoneal metastasis in gastric cancer have been conducted,but due to the nascent nature of these studies,the use of PET/MRI may not be currently available for patients.
There were no studies comparing radiomic modelling to the conventional diagnostic modalities available at the time of the search.Hence,essential analysis of quantitative values could not be carried out and the efficacy of radiomic modelling cannot be fully assessed.Due to its high potential based on preliminary investigations,more research is necessary to provide patients with a possible non-invasive alternative to staging laparoscopy in the diagnosis of peritoneal metastases.
CONCLUSION
Overall,staging laparoscopy outperformed CT scans in every measured aspect.These findings indicate that staging laparoscopy is statistically the superior modality for the diagnosis of peritoneal metastases in patients with gastric cancer or to rule out peritoneal metastases in other patients.It is important to note,however,that staging laparoscopies are still considered an invasive surgical procedure where general anaesthesia is necessary and multiple surgeons are involved.This would implicate the risks of anaesthesia,infection,and require more time and resources,and as a result,cost per patient may increase.
As such,non-invasive imaging remains invaluable in the work-up of gastric cancer patients.Among the commonly available scanning modalities,MRI scans have demonstrated superior performance in detecting peritoneal metastases compared to CT scans,which in turn showed slightly better results than PET scans.Hence,there is potential in these scanning modalities to provide patients with a non-invasive yet accurate alternative to staging laparoscopy,especially with the addition of alternate radiotracers such as FAPI and Flurothyrmine.However,further research is imperative to enhance the sensitivity and specificity of these techniques in the diagnosis of peritoneal carcinomatosis,such that they may soon be comparable to staging laparoscopies.In the same vein,more research in radiomic modelling is pivotal in achieving the same goal,as it has shown great promise in attaining a comparable,non-invasive alternative to staging laparoscopies.
ARTICLE HIGHLIGHTS
Research background
Staging laparoscopy is currently the gold standard for diagnosing peritoneal metastasis in gastric cancer patients.However,this procedure comes with risks of general anaesthesia and surgery which are of importance in elderly and frail patients,the demographic most affected by gastric cancer.Hence,we sought to evaluate non-invasive alternatives to staging laparoscopy with comparable accuracy.
Research motivation
Staging laparoscopy remains the gold standard for diagnosing peritoneal metastasis in gastric cancer patients,which comes with risks of general anaesthesia and surgery.Many non-invasive diagnostic modalities are available in the current day and age,hence,we sought to evaluate non-invasive alternatives to staging laparoscopy that may provide us with comparable accuracy.With further research in this field,along with newer developments such as radiomic modelling and new radiotracers,there is great potential for developing such a diagnostic tool with comparable or even greater accuracy than staging laparoscopy.
Research objectives
We sought to determine if computed tomography (CT),magnetic resonance imaging (MRI) and positron emission tomography (PET) could be a potential non-invasive yet accurate alternative to staging laparoscopy.
Research methods
Data from relevant studies that reported patients with peritoneal metastasis secondary to gastric cancer diagnosed by non-invasive scans were extracted and presented according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.Significant data such as sensitivity,specificity,negative and positive predictive values were analysed and compared between diagnostic modalities in our systematic review.
Research results
Our findings suggested that staging laparoscopy still delivered the best results in terms of sensitivity,specificity,negative and positive predictive values when compared to CT scans in diagnosing peritoneal metastasis in advanced gastric cancer.MRI had generally outperformed CT scans which had in turn,generally performed better than PET scans.Despite this,the difference in performance between all the diagnostic modalities are marginal,suggesting that there is great potential for the development of the ideal diagnostic tool capable of providing us with the same or even better accuracy than staging laparoscopy,while remaining non-invasive.With additional tools such as radiomic modelling and new radiotracers,the development of such a diagnostic modality may be possible sooner than expected.
Research conclusions
Although staging laparoscopy remains superior to other non-invasive diagnostic modalities in the detection of peritoneal metastasis in advanced gastric cancer,the potential for developing a comparable or even better diagnostic tool is great.This may be achieved with new technologies such as radiomic modelling and new radiotracers,on top of the already advanced capabilities of CT,MRI and PET scans.With further research,this breakthrough may be possible sooner than expected.
Research perspectives
Given the rapid and enthusiastic development of new technologies in diagnostic tools,the development of a highly sensitive and specific non-invasive alternative to staging laparoscopy in peritoneal metastasis detection is highly likely with further research.On top of the already cutting edge diagnostic modalities,additional improvements and developments may bring us closer than ever to this goal.
FOOTNOTES
Author contributions:Ho SYA took part in screening the included studies,performed data extraction,analysed and interpreted the results,and prepared the manuscript;Tay KV led the study conception and design,took part in screening the included studies,and contributed in manuscript revision;All authors reviewed the results and approved the final version of the manuscript.
Conflict-of-interest statement:The authors have no financial conflicts or interests to disclose and no sources of funding were involved in the writing of this paper.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist,and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Singapore
ORCID number:Si Ying Adelina Ho 0009-0009-6830-3730.
S-Editor:Fan JR
L-Editor:A
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2023年10期
World Journal of Gastrointestinal Surgery2023年10期
- World Journal of Gastrointestinal Surgery的其它文章
- Gastric adenosquamous carcinoma with an elevated serum level of alpha-fetoprotein: A case report
- Giant dedifferentiated liposarcoma of the gastrocolic ligament: A case report
- Hereditary hemorrhagic telangiectasia involving portal venous system: A case report and review of the literature
- Mucocutaneous ulcer positive for Epstein-Barr virus,misdiagnosed as a small bowel adenocarcinoma: A case report
- Three-dimensional computed tomography reconstruction diagnosed digestive tract perforation and acute peritonitis caused by Monopterus albus: A case report
- Postpolypectomy syndrome without abdominal pain led to sepsis/septic shock and gastrointestinal bleeding: A case report
