Imbalance between myopic shift and the minimum amplitude of accommodation: a hypothesis for the pathogenesis of ocular hypertension secondary to drug-induced bilateral acute ciliochoroidal effusion
Shan-Cheng Si*, Jia-Teng Lin2*, Min Zhang3, An-Ming Chen, Lei Wang, Meng-Qi Cui2, Yun-Tao Hu
1Eye Center, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University, Beijing 102218, China; 2Department of Ophthalmology, Rongcheng Eye Hospital, Weihai 264333, Shandong Province, China; 3Department of Ophthalmology, Beijing Hepingli Hospital, Beijing 100013, China
Abstract
•AIM:To report 5 cases with drug-induced bilateral acute ciliochoroidal effusion (DBACE) and myopic shift, with or without ocular hypertension (OHT), summarize patients’ clinical characteristics and recovery process of DBACE, and investigate the possible pathophysiological mechanism.
•METHODS:A retrospective observational case study conducted from June 2017 to February 2021. The included patients were subjected to a series of ocular examinations listed as follows:1) best corrected visual acuity; 2) intraocular pressure (IOP); 3) slit-lamp microscopy; 4) fundus photography; 5) ultrasound biomicroscopy (UBM); 6) subjective optometry; 7) axial length and anterior chamber depth . All patients were followed up every 2d until the diopters were completely restored to the state before the disease onset.
•RESULTS:In total, 5 patients aged 10-45 years old, including 3 female and 2 male patients, were enrolled in this study. All patients were bilaterally involved (5/5), and had myopic shift (5/5), of whom 3 patients had OHT (3/5). With the increase of age, myopic shift decreased, while OHT increased. Based on OHT, the dynamic aggravation process of DBACE was subdivided into 2 stages, stage 1 (myopic shift without OHT) and stage 2 (myopic shift with OHT). With the deterioration of DBACE, when myopic shift approached or exceeded the minimum amplitude of accommodation (MAA), IOP gradually rose, and DBACE progressed from stage 1 to stage 2. With the recovery of DBACE after discontinuing the suspicious drugs, DBACE in stage 2 first returned to stage 1, and then returned to normal.
•CONCLUSION:Pathophysiological mechanism of DBACE was subdivided into 2 stages, including stage 1 (myopic shift without OHT) and stage 2 (myopic shift with OHT). The transition between the two stages depends on the imbalance between myopic shift and MAA.
•KEYWORDS:drug-induced ciliochoroidal effusion; minimum amplitude of accommodation; swollen eyelid; myopic shift; low-concentration atropine; allergic conjunctivitis; ocular hypertension
Citation:Si SC, Lin JT, Zhang M,etal. Imbalance between myopic shift and the minimum amplitude of accommodation: a hypothesis for the pathogenesis of ocular hypertension secondary to drug-induced bilateral acute ciliochoroidal effusion.GuojiYankeZazhi(IntEyeSci) 2023;23(12):1935-1942
INTRODUCTION
Secondary uveal effusion may be accompanied by complications induced by pulmonary hypertension[1-3], amyloidosis[4], pregnancy-induced hypertension[5], monoclonal gammopathy[6], and pan-retinal photocoagulation[7]. In addition, it is associated with severe ocular side effects induced by some drugs, including immune checkpoint inhibitors[8], paracetamol[9], escitalopram[10], acetazolamide[11], chlorthalidone[12], bupropion[13], topiramate[14-15], and travoprost eye drops[16]. The etiology of secondary uveal effusion caused by systemic diseases is complex, but drug-induced secondary uveal effusion has a similar pathogenesis. Due to rare cases and various triggers, the exact mechanism and natural course of drug-induced bilateral acute ciliochoroidal effusion (DBACE) remain elusive.
In the present study, 5 cases diagnosed as DBACE and myopic shift, with or without ocular hypertension (OHT) were reported. Patients’ clinical characteristics and recovery process were summarized, and the possible pathogenesis was proposed.
METHODS
StudySubjectsThis was a retrospective observational case study conducted from June 2017 to February 2021. The study followed the Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Beijing Tsinghua Changgung Hospital (Beijing, China, No.22577-6-01). All enrolled patients signed an informed consent form before ocular examinations.
InclusionCriteria1) patients who experienced unexplained myopic shift and took suspicious drugs within 2wk before the myopic shift onset; 2) confirmation of DBACE through ultrasound biomicroscopy (UBM); 3) all case studies started on the first day of the disease onset reported by the patients.
OcularExaminationsAll enrolled patients were subjected to a series of ocular examinations listed as follows: 1) best corrected visual acuity (BCVA) assessment, the results of which were converted to the Snellen eye chart; 2) intraocular pressure (IOP) assessed by a non-contact tonometer (NCT); 3) slit-lamp microscopy; 4) fundus photography; 5) UBM (Suoer Electronic Co., Ltd., Foshan, China); 6) subjective optometry; 7) measurement of axial length (AL) and anterior chamber depth (ACD) by Lenstar (Haag-Streit AG, Köniz, Switzerland). All enrolled patients were followed up every 2d until the diopters were completely restored to the state before the disease onset.
RESULTS
DemographicandCharacteristicsofeachCasewithDrug-inducedBilateralAcuteCiliochoroidalEffusionontheFirstDayoftheDiseaseOnsetIn the present study, 5 patients aged 10-45 years old, including 3 females and 2 males, were recruited. The ALs ranged from 21.67 to 24.55 mm, with an average of 23.14 mm. All patients were bilaterally involved (5/5). All patients had myopic shift (5/5), of whom 3 patients had OHT (Cases 1, 3, and 4). With the increase of age, myopic shift gradually decreased, while the possibility of OHT increased. Patients’ demographic and clinical characteristics (e.g., gender, age, NCT, ACD, AL, visual acuity, subjective optometry) on the first day of DBACE onset are listed in Table 1.
SuspiciousMedications,ComprehensiveDiagnosis,Management,andRecoveryCharacteristicsofeachPatientwithDrug-inducedBilateralAcuteCiliochoroidalEffusionSystemic and topical medications for each patient were reviewed at the first visit. Suspicious drugs causing DBACE included oral metamizole sodium tablets (Case 1), anorexiant medications (Cases 3 and 4), sulfonamide diuretic (Case 5), and topical eye drops (Case 2). It is noteworthy that the suspicious topical medication for case 2 included the homemade 0.01% atropine eye drops (0.05% injectable atropine solution and preservative-free sodium hyaluronate eye drops were mixed with a ratio of 1∶4). In addition to DBACE, the atropine eye drops also caused severe contact allergic conjunctivitis. DBACE mainly occurred at 1-10d after the application of the suspicious drugs, showing two characteristics of myopic shift and OHT. Rapid recovery of OHT (about 2.3d) occurred earlier than the recovery of myopic shift (about 5.2d) in all patients after discontinuing the suspicious drugs, with or without combining with other medications, including intravenous mannitol, oral prednisone and topical ocular hypotensive or cycloplegic eye drops. Suspected medications, comprehensive diagnosis, managements, and recovery characteristics of each case with DBACE are listed in Table 2.
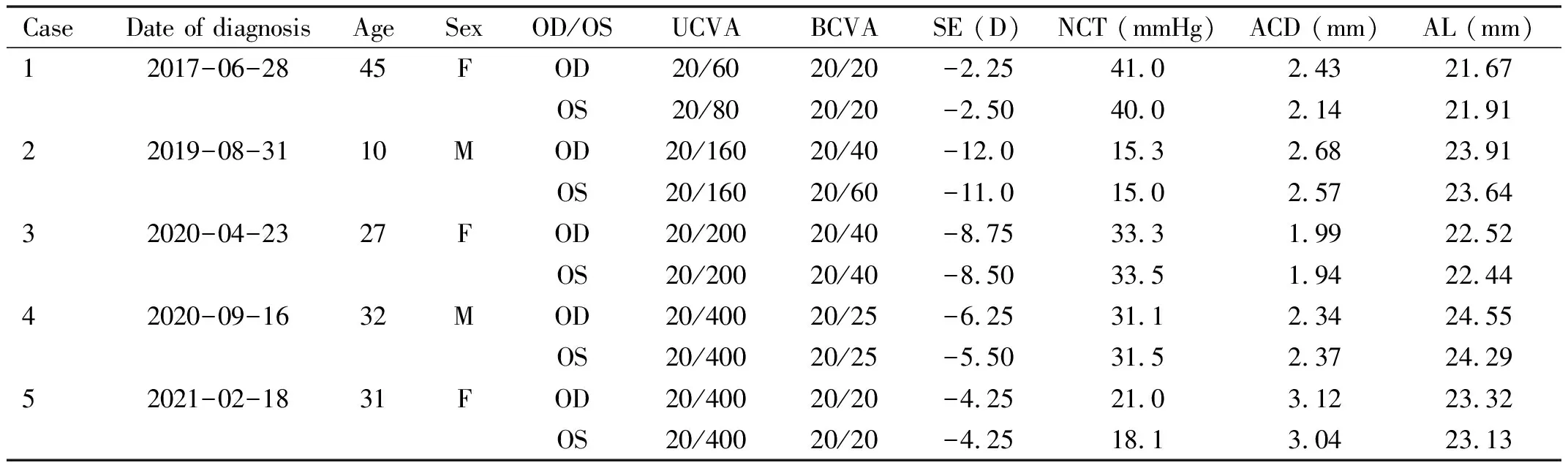
Table 1 Characteristics of each case with drug-induced bilateral acute ciliochoroidal effusion on the first day of disease onset
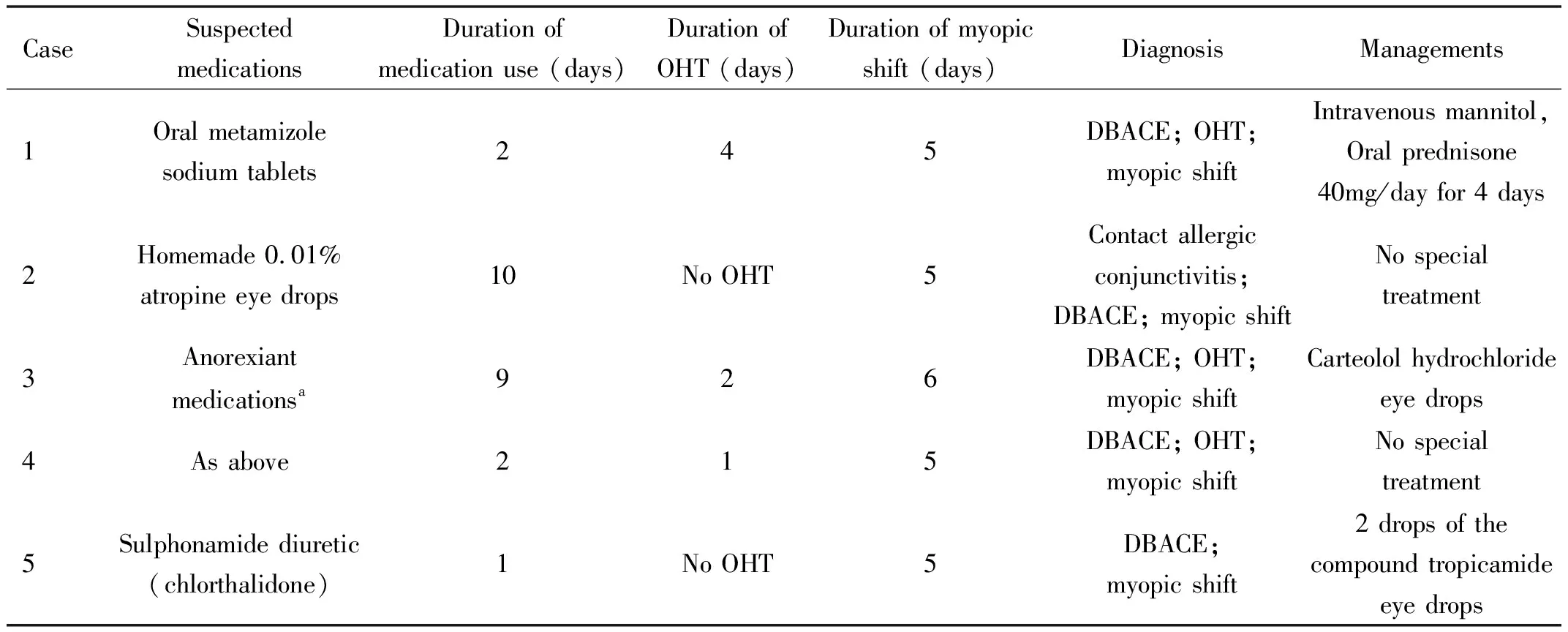
Table 2 Suspected medications, comprehensive diagnosis, managements and recovery characteristics of each case with drug-induced bilateral acute ciliochoroidal effusion
RelationshipbetweenMyopicShift&OcularHypertensionandMinimumAmplitudeofAccommodation&AnteriorChamberDepthTwo patients (Cases 2 and 5) without OHT showed no shallow ACD, and the extent of myopic shift was lower than the minimum amplitude of accommodation (MAA) calculated with the Hofstetter’s equation (15-0.25×age) on the first day of disease onset. However, the other 3 patients (Cases 1, 3, and 4) with OHT showed shallow ACD, and the myopic shift extent was close to or higher than the MAA on the first day of disease onset. When the myopic shift extent of 3 patients (Cases 1, 3, and 4) was lower than the MAA during the subsequent follow-up, their OHT immediately returned to normal. The details of relationship between myopic shift &OHT and MAA &ACD during the follow-up are summarized in Table 3.
TwoStagesofDrug-inducedBilateralAcuteCiliochoroidalEffusionIn all patients, the presence of DBACE was confirmed by UBM (Figure 1). According to the presence of OHT, pathophysiological mechanism of DBACE was subdivided into 2 stages, stage 1 (myopic shift without OHT) and stage 2 (myopic shift with OHT). Younger patients tended to stay in stage 1 (Cases 2 and 5), while older patients progressed to stage 2 (Cases 1, 3, and 4). The youngest patient (Case 2) in stage 1 had the greatest myopic shift (9.25 D), but no OHT; the oldest patient (Case No.1) in stage 2 had the least myopic shift (4.0 D) and OHT. With the deterioration of DBACE, when myopic shift approached or exceeded the MAA (Cases 1, 3, and 4), ACD tended to become shallower and IOP gradually risen, and DBACE progressed from stage 1 to stage 2 (Figure 2). With the recovery of DBACE after discontinuing the suspicious drugs, DBACE in stage 2 (Cases 1, 3, and 4) first returned to stage 1, and then, returned to normal (Figure 2). The details of the relationship between the two stages of DBACE and management of each stage are presented in Table 4.
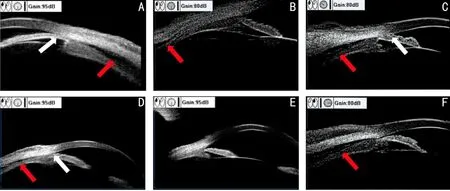
Figure 1 The results of ultrasound biomicroscopy of all 5 patients. A,C,D,F: On the first day after disease onset, ultrasound biomicroscopy of cases 1, 3, 4, and 5 showed drug-induced bilateral acute ciliochoroidal effusion (red arrow) to varying degrees with or without closure of the anterior chamber angle (white arrow); B: On the third day after disease onset, ultrasound biomicroscopy of case No.2 suggested mild drug-induced bilateral acute ciliochoroidal effusion without closure of the anterior chamber angle; E: 2d after discontinuing the suspicious drugs, ultrasound biomicroscopy of case No.4 indicated gradually recovered drug-induced bilateral acute ciliochoroidal effusion and widened anterior chamber angle.
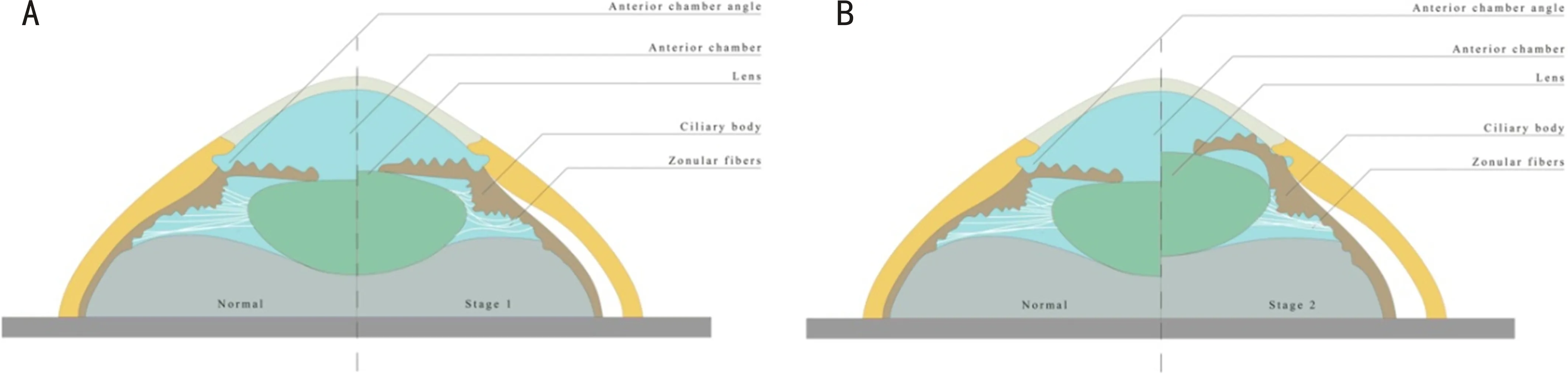
Figure 2 Characteristics and transformation of two stages of drug-induced bilateral acute ciliochoroidal effusion. A: When drug-induced bilateral acute ciliochoroidal effusion occurs, the suspensory ligament of lens becomes relaxed, and the lens may elastically retract to compensate for the relaxation of the suspensory ligament, which leads to thickening of the lens and myopic shift, namely stage 1; B: With the deterioration of drug-induced bilateral acute ciliochoroidal effusion, when the myopic shift approaches or exceeds the minimum amplitude of accommodation, the elastic retraction of the lens cannot compensate for the relaxation of the suspensory ligament, which eventually leads to anterior movement of the lens-iris diaphragm and subsequently shallower anterior chamber depth and ocular hypertension, namely stage 2.
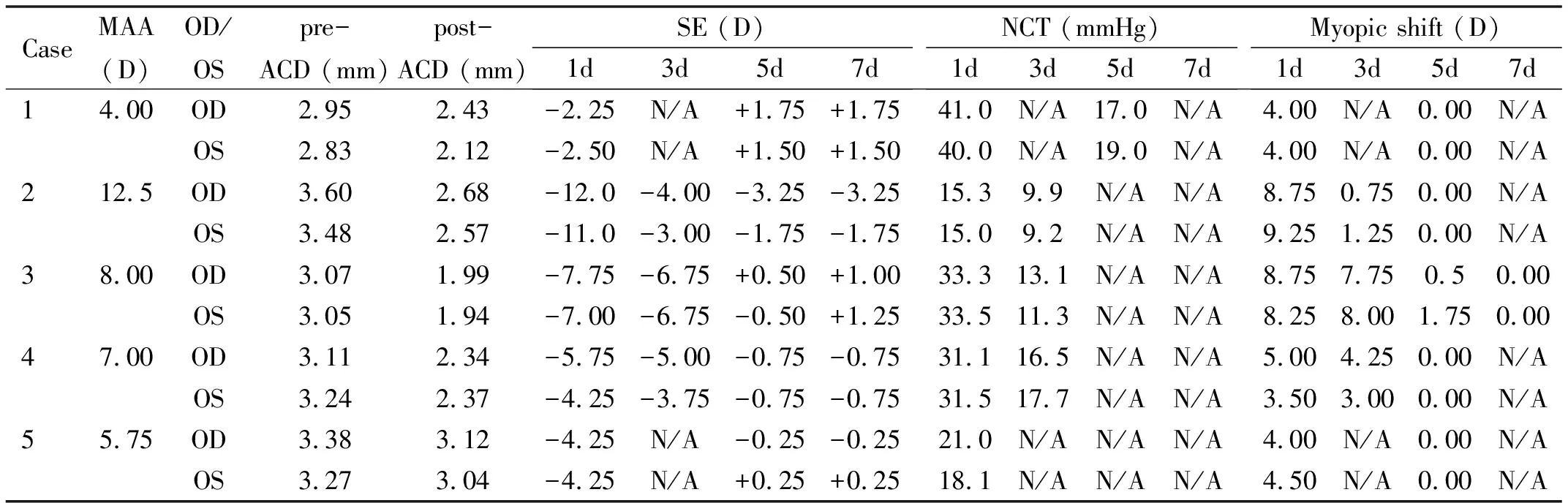
Table 3 The relationship between myopic shift &ocular hypertension and minimum amplitude of accommodation &anterior chamber depth during the follow-up

Table 4 The relationship between two stages of drug-induced bilateral acute ciliochoroidal effusion and main managements of each stage
DISCUSSION
In contrast to the most drug-induced uveal effusions with OHT[8-16,18], in the present study, 2 of the 5 patients had never been complicated by OHT during the whole follow-up (Cases 2 and 5). The average age of the 2 patients (20.5 years old) was younger than that of the other 3 patients (34.7 years old). Young patients may present with isolated myopic shift without OHT, which had been previously reported[17]. We hypothesized that the main reason is that young patients’ lenses are very elastic. Therefore, when DBACE and forward rotation of ciliary body occur, and then the suspensory ligament is relaxed, the anterior segment is mainly manifested as the increased curvature of lens surface in stage 1 (Figure 2A), rather than anterior movement of the lens-iris diaphragm in stage 2 (Figure 2B)[9]. The increased curvature of lens surface without shallow ACD and subsequent OHT in stage 1 indicate isolated myopic shift, which is mainly less than the MAA calculated using the Hofstetter’s equation (15-0.25×age)[19]. It is noteworthy that there was no obvious shallow ACD and OHT during the follow-up of the 2 patients (Table 3).
The other 3 older patients were clinically manifested as myopic shift plus OHT (Cases 1, 3, and 4). The possible reason is that the elasticity of the lenses gradually decreases with age. Under these circumstances, if DBACE and forward rotation of ciliary body occur, and then the suspensory ligament is relaxed, the curvature of lens surface may only increase slightly. The elastic retraction of the lens cannot compensate for the relaxation of the suspensory ligament, which eventually leads to anterior movement of the lens-iris diaphragm and the subsequent shallower ACD and OHT in stage 2 (Figure 2B). During the whole stage 2, myopic shift from severe anterior movement of the lens-iris diaphragm and slightly increased curvature of lens surface may approach or exceed the MAA (Table 3). The pathophysiological mechanism, including two stages, has a clear boundary line, that is, whether there is an increase of IOP (Figure 2). The details of relationship between the two stages of DBACE are listed in Table 4.
With the recovery of DBACE (Figure 2) after discontinuing the suspicious drugs, with the suspensory ligament pulling of the lens back, anterior chamber deepened, OHT disappeared, and the curvature of lens surface decreased; subsequently, myopic shift was improved (Cases 1, 3 and 4). As a result, the abnormality in stage 2 first returned to stage 1, and then, returned to normal (Cases 1, 3 and 4). The details of the recovery course of DBACE are summarized in Table 3.
It was reported that 4 patients (Cases 1, 3, 4 and 5) suffered from DBACE caused by oral medications, possibly due to the combination of drug metabolites and uveal tissues that induced an immune response[16]. The oral drugs involved in our cases were all previously described[9,12,20-21]. The youngest patient (Case 2) suffered from DBACE caused by low-concentration atropine eye drops, and no similar report has been published yet. However, we found several articles[16,22-25]related to topical travoprost, latanoprost and brinzolamide eye drops causing DBACE. Previous studies[16,22]demonstrated that the possible mechanism is that prostaglandin, as an inflammatory mediator, increases the permeability of choroidal blood vessels, which causes swelling of the ciliary body and anterior movement of the lens-iris diaphragm, eventually leading to OHT. It is easy to understand the contact allergic conjunctivitis of a patient (Case 2) induced by atropine eye drops. In fact, allergic conjunctivitis, which is characterized by the swollen eyelid and conjunctival hyperemia and caused by atropine eye drops, is not rare, and the incidence reaches 4.1%, however, it is essential to indicate whether the allergy occurs in association with the concentration of atropine eye drops[26]. It is noteworthy that atropine is a hydrophilic drug that can easily penetrate the sclera and reach the choroid[27]. Therefore, atropine may cause a delayed allergic reaction or choroidal vasodilation characterized by uveal effusion in choroidal tissues[27-28]. This may be the first report that atropine eye drops cause high myopic shift with uveal effusion. However, with the widespread use of atropine eye drops in controlling the progression of myopia[28], more similar cases will be reported in the future.
As reported previously[18,21], the mean recovery time of myopic shift was about 5.2d in all patients after discontinuing the suspicious drugs, combined with other medications or not, including intravenous mannitol, oral prednisone and topical ocular hypotensive or cycloplegic eye drops. Abtahietal[18]found that some patients could present with vitreitis, and the majority of them responded to glucocorticoids. To date, no standard treatment for DBACE has been presented, and termination of suspicious drugs is the only effective choice.
It is noteworthy that our research has certain limitations. First, only 5 cases were included in our study because few cases were reported from June 2017 to February 2021. Second, although we searched to figure out the entire natural course, no similar description was found. Thus, our conclusion remains to be verified. Third, the retrospective nature of the study may be a source of bias. Fourth, all patients were diagnosed by UBM, while no long-term follow-up was conducted. Hence, further research needs to be conducted to eliminate the above-mentioned limitations and to confirm our findings.
DescriptionofoneRepresentativeCaseNo.2A 10-year-old young patient was referred to our hospital for sudden onset of binocular blurred vision and swollen eyelids for 3d. Immediately before the event, the patient had used the homemade 0.01% low-concentration atropine eye drops (0.05% injectable atropine solution and preservative-free sodium hyaluronate eye drops were mixed with a ratio of 1 to 4) to prevent the rapid progression of myopia one time per night for 1wk. The patient had no history of ocular and systemic diseases except for the binocular mild myopia.
External eye examination showed bilateral severe hyperemia and edema of the bulbar conjunctivas,as well as swollen eyelids (Figure 3A). Visual acuity could be corrected to 20/20 OD and 20/20 OS with -4.00 OD and -3.00 OS, from uncorrected vision of 20/400 in both eyes. Besides, IOP was 9.9 mmHg OD and 9.9 mmHg OS. Slit lamp examination of both eyes revealed transparent cornea, moderate ACD, round pupil, sensitive pupil light reaction, and transparent lens. Fundus photography displayed a grayish-white macular region with spotted yellow-white lesions of the left eye (Figure 4A). Fundus fluorescein angiography (FFA) did not suggest an abnormal fluorescence, while indocyanine green angiography (ICGA) revealed mottled hyperfluorescence for less than 8-9min on both eyes (Figure 4B). UBM showed mild choroidal detachment at 6 o’clock of the right eye (Figure 1B) and striped dark areas in the suprachoroidal space at 12 o’clock of the left eye (Figure 4C). Optical coherence tomography (OCT) revealed serous retinal detachment (SRD) in macular region of the left eye (Figure 4D), while no SRD was found in the right eye.
Next, we reviewed his medical records from a local hospital 2d before his admission. The data showed that he had a high myopic shift. Visual acuity can only be corrected to 20/40 OD and 20/60 OS with -12.00 OD and -11.00 OS, from uncorrected vision of 20/160 OD and 20/60 OS. IOP was 15.3 mmHg OD and 15.0 mmHg OS. External eye examination suggested bilateral severe hyperemia and edema of the bulbar conjunctivas, as well as swollen eyelids. Slit lamp examination of both eyes suggested moderate ACD. OCT indicated no SRD in the macular region of the left eye. Subsequently, some necessary checkups were added. The central ACD measured by the Lenstar was 3.48 mm OD and 3.37 mm OS; the AL of the eye was 23.91 mm OD and 23.64 mm OS.
During the subsequent 2 consecutive days of follow-up in our clinic, the patient did not receive any treatment other than termination of the homemade low-concentration atropine eye drops, while his bilateral eyelids’ edema gradually eased and the double eyelid in the right eye reappeared (Figure 3B). At the same time, his abnormal diopter of both eyes was gradually reduced to the state before the onset, the spotted yellow-white lesions in the macula region of the left eye were gradually faded, and the SRD of the left eye was gradually improved (Figure 4 E-F).
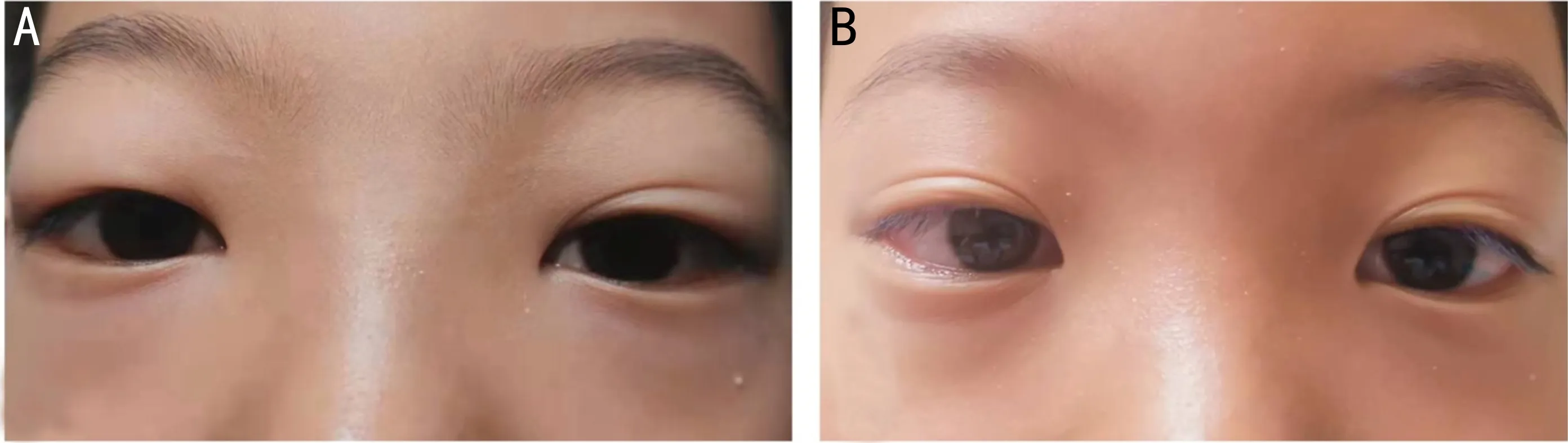
Figure 3 External photographs of case No.2, which indicated contact allergy induced by low-concentration atropine eye drops. A: On the 3rd day after disease onset, photography of the appearance of both eyes indicated severe bilateral hyperemia and edema of the bulbar conjunctivas, swollen eyelids. B: On the 5th day after disease onset, external photograph of the same patient’s both eyes showed gradual remission of bilateral eyelids’ edema and reappearance of the double eyelid in the right eye.

Figure 4 Ocular examination of case No.2, which indicated bilateral acute ciliochoroidal effusion induced by low-concentration atropine eye drops. On the 3rd day after disease onset, fundus photography, optical coherence tomography, ultrasound biomicroscopy, and indocyanine green angiography of the left eye showed a grayish-white macular region with spotted yellow-white lesions (A), mottled hyperfluorescence for less than 8min (B), striped dark areas (red arrow) in the suprachoroidal space at 12 o’clock (C), and serous retinal detachment in macular region (D), respectively. Optical coherence tomography displayed gradually improved serous retinal detachment of the left eye (E and F) during the 2 consecutive days of follow-up.