Endoscopic vs radiologic gastrostomy for enteral feeding: A systematic review and meta-analysis
Evellin Souza Valentim dos Santos, Guilherme Henrique Peixoto de Oliveira, Diogo Turiani Hourneaux de Moura, Bruno Salomao Hirsch, Roberto Paolo Trasolini, Wanderley Marques Bermardo, Eduardo Guimaraes Hourneaux de Moura
Abstract BACKGROUND Percutaneous endoscopic gastrostomy (PEG) and percutaneous radiological gastrostomy (PRG) are minimally invasive techniques commonly used for prolonged enteral nutrition.Despite safe, both techniques may lead to complications, such as bleeding, infection, pain, peritonitis, and tube-related complications.The literature is unclear on which technique is the safest.
Key Words: Gastrostomy; Adverse events; Meta-analysis; Percutaneous endoscopic; Radiological gastrostomy
INTRODUCTION
Patients unable to tolerate oral intake for a prolonged period have an indication for an alternative route of enteral feeding,such as gastrostomy[1].Gastrostomy involves connecting the stomach to an outflow in the skin with a tube, providing an alimentary route.
The first gastrostomy was performed in the 19thcentury, and Stamm's technique, surgical gastrostomy described in 1894, was long considered standard for performing a prolonged enteric access.The surgical technique became less performed with the emergence of the endoscopic technique.The method of percutaneous endoscopic gastrostomy (PEG)was first used in 1980 by Gauderer and Ponsky[2].The technique was developed as a minimally invasive feeding route for neurologically impaired patients.
In 1981, percutaneous radiologic gastrostomy (PRG) was described[3], expanding the options available.This was an important development for scenarios such as head and neck tumors, where endoscopy is sometimes not an option, due to upper obstruction.
Endoscopic and radiological gastrostomy are both considered effective, safe and minimally invasive[4,5].The preferred method is often based on specialist opinion or institution preference.We aim to perform a systematic review of the literature and meta-analysis to establish which approach has the lowest complication rate.
MATERIALS AND METHODS
Protocol and registration
This study was performed in conformity with the Preferred Reporting Items for Systematic Reviews and Meta-analyses(PRISMA) guidelines[6] and was registered in the International Prospective Register of Systematic Reviews (PROSPERO)under the file number CRD42022377213.
Information source and literature search
The electronic databases searched were MEDLINE (via PubMed), Embase, Scopus, LILACS, the Cochrane Library (via BVS), and Google Scholar from inception until November 2022.The search was performed with the following mesh terms: [(Gastrostomy or Gastrostomies) and (Endoscopic)].
Eligibility criteria
The selection criteria were studies that contained patients undergoing gastrostomy, that compared the two interventions(PEG and PRG) and that included the following outcomes: Bleeding, infection, pain, peritonitis, tube-related complications with their results in absolute values.
Eligibility assessment was performed independently and standardized by 2 authors according to PRISMA guidelines[6].Discrepancies between reviewers were resolved by consensus.A third reviewer was consulted in case of disagreements.
Case reports, reviews and letters were excluded.Studies that exclusively analyzed patients under 18 years of age,compared other techniques or did not consider the desired outcomes were excluded.Studies with the pediatric population were excluded because of anatomical differences with the adult population and consequently different complications.
To assess the quality of eligible studies we used The Risk of Bias in Nonrandomized Studies (ROBINS-I)[7] to analyze the comparative studies and the Cochrane risk-of-bias tool for randomized trials (RoB2)[8] to analyze the randomized studies.The quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria using the GRADE pro Guideline Development Tool software (Mc Master University,Ontario, Canada)[9].
Data analyses
The randomized controlled trials (RCT) studies were analyzed separately from the observational studies since they have different levels of evidence.This allowed us to compare the outcomes separately and to make a global analysis of the results.
The analysis was performed using Review Manager (RevMan 5.4) from the Cochrane Informatics & Knowledge Management Department website.Risk differences for dichotomous variables were computed using a fixed-effects model and the respective forest and funnel plots were obtained.Data on risk differences and the 95% confidence intervals (CI)for each outcome were calculated using the Mantel-Haenszel test.Inconsistency (heterogeneity) was qualified and reported using the Chi-squared (Chi2) and Higgins methods and was termedI2.I2values > 50% were considered to indicate substantial heterogeneity.We performed an analysis using a funnel plot to identify possible outliers.If the sample became homogeneous after excluding possible outliers, the studies were permanently excluded.We used random effects to reduce the influence of heterogeneity on the final result[10].Outcome measures are described as the mean difference or risk difference (RD), with their corresponding 95%CI.
RESULTS
The initial search showed 15585 results, after removing the duplicate articles, 6490 remained.A total of twenty studies passed the screening stage and were included in qualitative synthesis, seventeen studies met criteria to be included in the metanalysis, two were prospective randomized studies and fifteen were retrospective cohort studies.The search strategy can be visualized in the following diagram (Figure 1).
Study characteristics
Seventeen studies were included in the systematic review, including two RCTs, one prospective, and 14 retrospective cohort studies.A total of 465218 individuals, with 273493 received PEG and 191725 PRG.The characteristics of the studies can be seen in Table 1[11-27].Early outcomes were analyzed.
Risk of bias within studies
The ROBINS-I and ROB-2 scoring system were used to evaluate risk of bias for observational[12-18,20-27] and randomized studies[11,19], respectively (Table 1).We identified a low risk of bias in the two RCT studies (Figure 2), and a strong methodological quality.As for the observational studies, we note that 5 of them present serious risk of bias[13,15,25,27] and 5 moderate risk[12,14,18,21,23], mostly due to issues in the dissemination of results (Figure 3).
Quality of evidence
The objective criteria of GRADE analysis to evaluate the quality of evidence identified moderate certainty for pain and infection, low certainty for peritonitis and very low certainty for bleeding and pneumonia (Figure 4).
Infection
A total of 465198 patients from 17 studies[12-27] were analyzed.There was no difference in the incidence of infection in retrospective (95%CI: -0.01 to 0.00;P< 0.00001;I2= 74%) or randomized (95%CI: -0.06 to 0.04;P= 0.68;I2= 0%) studies.In the overall analysis there was no difference in the meta-analysis of observational and RCT studies combined (95%CI: -0.01 to 0.00;P= 0.56;I2= 70%) (Figure 5A).
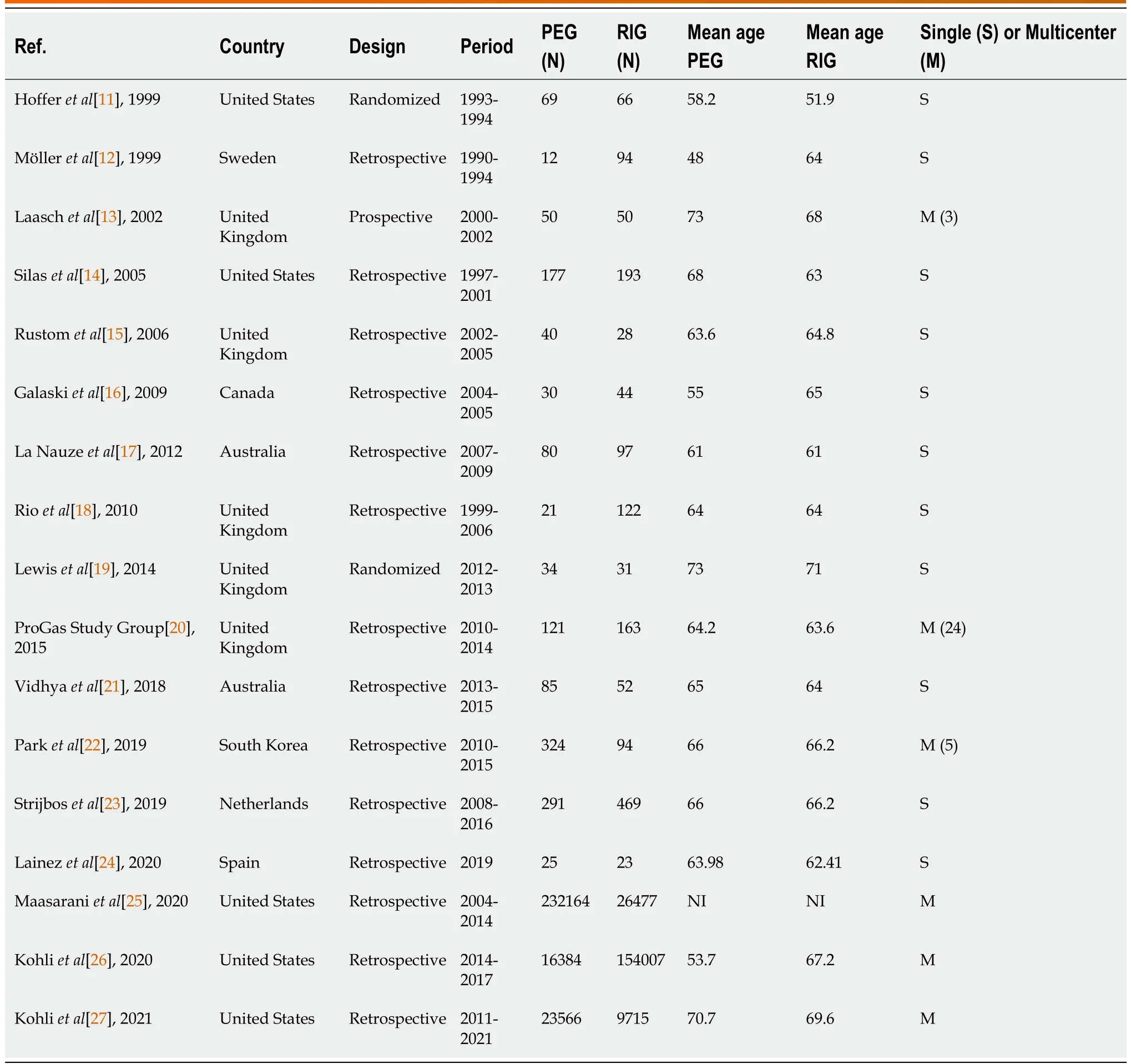
Table 1 Early outcomes were analyzed
Bleeding
A total of 464618 patients from fourteen[11-13,16,17,19-27] studies were analyzed.There was no difference in the incidence of bleeding in observational studies (95% CI: -0.00 to 0.00;P< 0.00001;I2= 76%) or RCTs (95%CI: -0.06 to 0.02;P= 0.43;I2= 0%).In the overall analysis there was no difference in the meta-analysis of observational and RCT studies combined (95%CI: -0.00 to 0.00);P= 0.81;I2= 73%) (Figure 5B).
Pneumonia
A total of 1796 patients from eight[11,13,17,19-21,23,24] studies were analyzed.There was no difference in the incidence of pneumonia in comparative studies (95%CI: -0.00 to 0.04;P= 0.28;I2= 20%) or RCT (95%CI: -0.10 to 0.10;P= 0.39;I2= 0%)studies.In the overall analysis there was no difference in the meta-analysis of observational and RCT studies combined(95%CI: -0.00 to 0.03;P= 0.44;I2= 0%) (Figure 5C).
Peritonitis
A total of 34461 patients from five[12,17,21,23,27] were analyzed.There was no difference in the incidence of peritonitis in retrospective (95%CI: -0.02 to 0.01;P< 0.0001;I2= 86%) studies.It was not possible to evaluate the peritonitis outcome in RCT studies because this outcome was not included in these studies (Figure 5D).
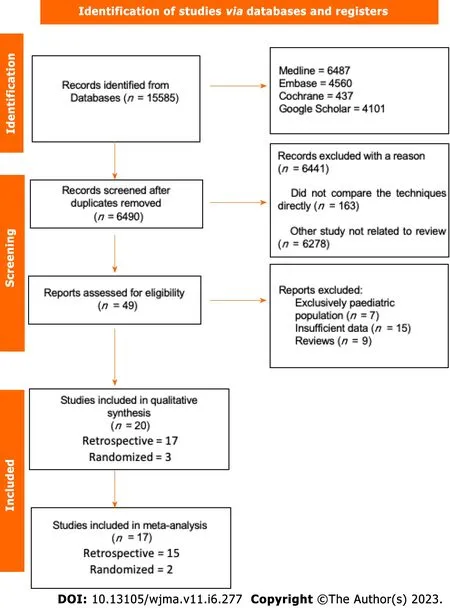
Figure 1 Flow diagram showing study selection process.
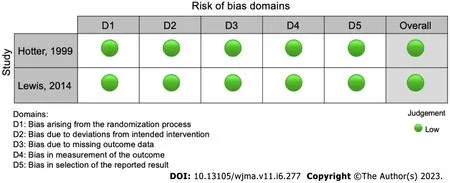
Figure 2 Risk of bias according to ROB-2.
Pain
A total of 260793 patients from seven[14,17,18,20,22,23,25] studies were analyzed.There was no difference in the incidence of pain in retrospective (95%CI: -0.05 to 0.02;P< 0.00001;I2= 91%) studies.It was not possible to evaluate the pain outcome in RCT studies because this outcome was not included in these studies (Figure 5E).
Tube related complications
A total of 464689 patients from 14 studies[11-19,21-23,25,26] were analyzed.This analysis showed a significant difference in tube related complications in observational studies favoring PEG (95%CI: -0.03 to -0.08;P< 0.00001), although there was no significant difference in randomized studies (95%CI: -0.07 to 0.04;P= 0.13).In the global analysis there was a difference, favoring PEG (95%CI: -0.07 to -0.03;P< 0.00001) (Figure 6).
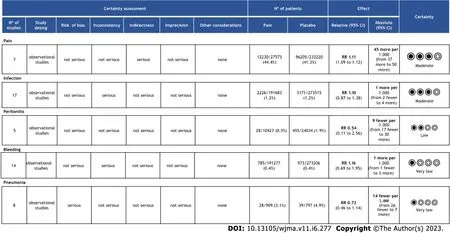
Figure 4 Quality of evidence assessed by Grading of Recommendations Assessment, Development, and Evaluation.
DISCUSSION
This meta-analysis shows that both PEG and PRG techniques are similar in terms of safety profile, except potentially in tube-related complications, which was higher for PRG in observational studies (Evidence 2A).We included 20 studies in this review (3 randomized and 17 comparative studies) and 17 in our meta-analysis, totaling 465218 individuals, with 273493 undergoing PEG and 191725 undergoing PRG.While other metanalyses compared these 2 approaches[28-34], this analysis is unique as it includes the largest number of adult patients and also separates RCT and observational studies providing further insight.This approach follows Cochrane recommendations and thus provides for a more reliable comparison.Additionally, we separated all adverse events, including pain and pneumonia, which have not been individually analyzed to date.The adverse effects chosen were based on previous publications showing the most frequent complications related to the method[4].
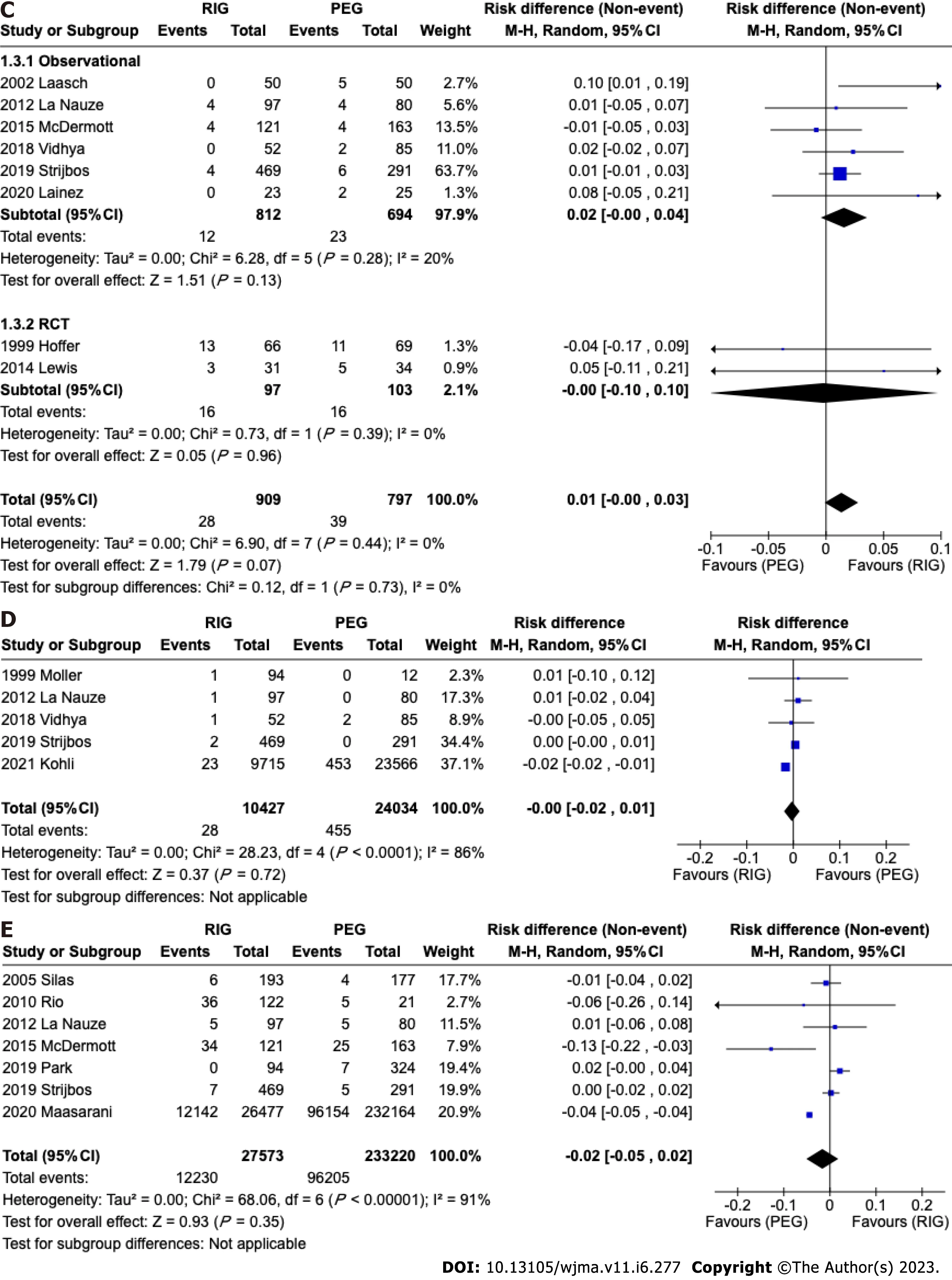
Figure 5 Forest plot studies reporting.A: Outcomes infection; B: Outcomes bleeding; C: Pneumonia; D: Outcomes peritonitis; E: Pain.
The three most common techniques for performing gastrostomy are endoscopic, radiologic, and surgical.Although surgical gastrostomy was the first described approach, it is now less used due to its invasiveness.A meta-analysis including RCT (evidence 1A) comparing endoscopic and surgical techniques demonstrated a lower number of minor complications for endoscopic procedures[35].
Until now, there is no consensus regarding the superiority of either endoscopic or radiologic gastrostomy.Our results clarify that both approaches are similar in terms of safety as shown in our meta-analysis including only RCTs.Furthermore, a recent RCT including 42 patients comparing the two techniques[36], showed similar results to this metaanalysis.Unfortunately, this RCT was not included due to a lack of data available in the published manuscript, despite our attempt to contact the author.
Local infection is a common adverse outcome of gastrostomy.For this reason, the American Society for Gastrointestinal Endoscopy[37] and the Society for Interventional Radiology[38,39] recommends administering periprocedural antibiotics.The studies utilized in this meta-analysis did not expressly state if antibiotics were administered or not, but as this is a common practice, it was likely used.Our meta-analysis did not demonstrate a significant difference regarding infection in both RCT and non-RCT analysis.
In previous publications[26,27], it has been stated that patients undergoing PEG have a higher rate of bleeding since PEG is preferentially performed in patients with diseases requiring antiplatelets or anticoagulants such as stroke and vascular dementia[27,40].We expected to prove this hypothesis, however, this meta-analysis demonstrated a low risk of bleeding due to the gastrostomy procedure, without a statistically significant difference between PEG and PRG in both RCT and observational studies.Data on antiplatelet and/or anticoagulant medications among patients who bled were not available.
This study showed no significant difference in the incidence of pneumonia.In previous studies it was observed that gastrostomy compared to nasogastric feeding has a lower incidence of pneumonia, however, this complication is a major cause of mortality in patients undergoing gastrostomy[16].It is important to state that we were not able to evaluate gastrostomy and gastrojejunostomy separately due to a lack of data.Gastrojejunostomy is associated with a theoretically lower rate of reflux and pneumonia[11,19].
Pain and peritonitis are complex outcomes to measure objectively.Since the definition of these outcomes differs in several studies[13,14,17,18,20-25].There was no statistical difference between the two methods in our study.
In the analyzed studies, the types, brands, and sizes of tubes were not differentiated.This heterogeneity may influence the results of this analysis.The meta-analysis of observational studies demonstrated a statistically significant difference in the incidence of tube-related complications of a PEG and PRG, such as dislocation, leak, obstruction, or breakdown,showing a higher incidence in PRG.In the RCT meta-analysis, there was no difference.However, the observational studies included 464489 patients versus 200 patients from RCT studies and this should be considered if the RCTs were underpowered to detect a small difference between the techniques.A difference may be expected due to the size difference between endoscopic and radiological techniques.PEG is usually performed using 20FR or 24FR tubes whereas PRG uses 14-16 FR[41].The size of the gastrostomy ostium influences the incidence of migration; a smaller caliber is associated with a higher incidence of migration and obstruction.The feeding tube can become blocked due to various reasons, such as the accumulation of food formula, medications, or debris.Smaller tubes increase the probability of the tube becoming blocked.Leaks can occur around the insertion site or through the tube itself, which can cause skin irritation and infection, so if the size of the skin insertion is larger than the tube caliber there is a greater chance of leakage.
Tube-related complications are usually associated with longer hospital stays, the need for further procedures, and potentially increased costs[16,33,42].Evaluating costs is challenging since procedure cost varies significantly between countries.A study comparing the two techniques published in 2009 showed that the costs of the procedures are also different, with PEGs being 43% more expensive than PRGs[16] but the costs are related only to the procedure and not to the overall cost.In Brazil, PEG has a low cost, being more cost-effective than a CT scan.Although few studies provide information regarding costs, this information would be useful, given that these procedures are performed on a large scale worldwide[11,16].
The strengths of this study include a large number of patients from different continents, dedicated analysis of RCT data, use of a validated quality assessment tool, and application of the GRADE process to assess the quality of our data.
Although systematic review and meta-analysis represent the most thorough assessment of available evidence comparing the risks of PEG and PRG, our study has limitations as discussed above.Most data was gathered from observational studies.Additionally, lack of data on tube size, antibiotic, and anticoagulant use, indications for the gastrostomy procedure, and inclusion of both gastrostomy and gastrojejunostomy all limit understanding of potential nuances that differentiate PEG from PRG.
In summary, both approaches are safe.Thus, individual evaluation is required considering several factors including local and personal experience, device availability, cost, and patient preference.
CONCLUSION
PEG and PRG present a similar safety profile.However, PRG is associated with a slightly higher rate of tube-related complications, potentially related to the small caliber of the gastrostomy tube.
ARTICLE HIGHLIGHTS
Research perspectives
This study aimed to determine which technique is safer for the patient, and both methods proved to be safe.We can conclude that the choice of technique depends on the type of patient, the experience of the service, the cost, and the availability of the method.
FOOTNOTES
Author contributions:dos Santos ESV contributed acquisition of data, analysis, interpretation of data, drafting the article, revising the article, final approval; de Oliveira GHP, dos Santos ESV and Hirsch BS contributed analysis and interpretation of data, revising the article; de Moura DTH contributed analysis of data, interpretation of data, drafting the article, revising the article, final approval;Bernardo WM contributed analysis of data, interpretation of data, drafting the article, revising the article, final approval; de Moura EGH contributed analysis and interpretation of data, drafting the article, revising the article, final approval.
Conflict-of-interest statement:The authors deny any conflict of interest.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Brazil
ORCID number:Guilherme Henrique Peixoto de Oliveira 0000-0002-1057-2390; Diogo Turiani Hourneaux de Moura 0000-0002-7446-0355; Bruno Salomão Hirsch 0000-0002-0777-0150; Roberto Paolo Trasolini 0000-0001-8059-9807; Wanderley Marques Bernardo 0000-0002-8597-5207;Eduardo Guimarães Hourneaux de Moura 0000-0003-1215-5731.
S-Editor:Liu JH
L-Editor:A
P-Editor:Zhao S
 World Journal of Meta-Analysis2023年6期
World Journal of Meta-Analysis2023年6期
- World Journal of Meta-Analysis的其它文章
- Overview of angiogenesis and oxidative stress in cancer
- Evidence relating cigarettes, cigars and pipes to cardiovascular disease and stroke: Meta-analysis of recent data from three regions
- History, origin, transmission, genome structure, replication, epidemiology, pathogenesis, clinical features,diagnosis, and treatment of COVID-19: A review
