Comparative outcomes of the pathogen in cultured Jones tubes used in lacrimal bypass surgery according to follow up periods
Bo Hyun Park, Hui Kyung Kim, Yeon Ji Jo, Jong Soo Lee
Department of Ophthalmology, Pusan National University School of Medicine & Medical Research Institute of Pusan National University Hospital, Pusan 49241, Republic of Korea
Abstract
● KEYWORDS: Jones tube; lacrimal bypass surgery; Pseudomonas aeruginosa; Proteus mirabilis;Staphylococcus aureus
INTRODUCTION
Conjunctivodacryocystorhinostomy (CDCR) or lacrimal bypass surgery originally described by Jones in 1962[1]is the standard treatment for canalicular obstruction.In practice,this surgical procedure is used in cases of less than 8 mm of residual canaliculi, congenital agenesis of the punctum or canaliculi, permanent paralysis of the lacrimal pump and lacrimal canalicular obstruction caused by trauma, tumor,systemic chemotherapy and radiation therapy[2-4].
Once lacrimal tubes are inserted, they can be retained lifelong in case of no complications.Complications associated with the lacrimal tube include extrusion, tube displacement, obstruction,infection, granuloma and strabismus[5-7].These complications can eventually lead to tube removal, thus affecting the success rate of lacrimal surgery.
Since the tube used for lacrimal bypass surgery is exposed directly to the nasal cavity and conjunctiva, there is highly risk of infection or inflammation.Kreiset al[8]reported periorbital emphysema associated with Jones tube.Vaidyaet al[9]reported a case of Jones tube infection by multiple microorganisms includingCorynebacterium kroppenstedtii.Kimet al[10]reported on the successful treatment of methicillin-resistantStaphylococcus aureus(MRSA) infection associated with Jones tube.However, there are only a few reports on the pathogens isolated from lacrimal tubes used in lacrimal bypass surgery.Therefore, we evaluated the pathogens isolated from Jones tube by culture and antibiotic sensitivity test according to the postoperative durations.These results will be useful to prevent and control infection of the lacrimal tube.And it will be useful for invention of a functional lacrimal stent with releasing antibiotics drug.

Table 1 Demographics and clinical data of subjects enrolled in this study mean±SD
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective observational analysis was performed in adherence with the Declaration of Helsinki and approved by Institutional Review Board (IRB No.2009-018-095).Our report is a retrospective study, so we did not obtain informed consent from subjects.
PatientsSeventy-one patients (81 eyes) who underwent removal of the Jones tube associated with lacrimal bypass surgery from Nov.2006 to Jan.2020 were enrolled in this study.The indications for Jones tube removal were ocular discomfort, infection, inflammation, tube migration or malposition.The procedure of tube removal was performed under local anesthesia for outpatients or inside the operation room.The tube was immediately sent to the microbiology laboratory in a transport medium tube.Then the removed Jones tubes were cultured to identify the bacteria and fungi using sheep blood agar, MacConkey agar, Chocolate agar, Sabouraud dextrose agar and Sabouraud dextrose chloramphenicol agar respectively.
Antibiotic sensitivity test (vancomycin, penicillin, erythromycin,gentamicin, clindamycin, oxacillin, ampicillin, amikacin,ciprofloxacin, ceftazole, tobramycin, aztreonam, and piperacillinetc.) was also performed.
Surgical TechniqueSurgery was performed following a previously reported method[11].In summary, the Bowman’s probe was introduced through an incision on the caruncle and was advanced smoothly across the lacrimal bone into the anterior portion of the middle turbinate through the incised caruncle.Then, Bowman’s probe #0 was pushed to penetrate the lacrimal bone between the lacrimal sac and nasal mucosa.Penetration size of the lacrimal bone was widened with a punctal dilator for insertion of the Jones tube, which was introduced over the probe into the nasal cavity and the probe was pulled out superiorly from the inserted tube.The bypass Jones tube was held stable with a prolene 8-0 or 9-0 (Ethicon;Somerville, NJ, USA) suture passed through a hole in the flange and attached to the adjacent edge of the caruncle.The size of the tube was measured by estimating the length of the Bowman’s probe from the caruncle to the tip of the probe,located about 2 to 3 mm above the nasal mucosal surface.
OutcomesThe results of the culture and antibiotic sensitivity test were compared according to the duration of tube removal after surgery: Group 1: within 1y, Group 2: from 1 to less than 5y, Group 3: from 5 to less than 10y, Group 4: over 10y.Fisher’s exact test was used for the comparison of parameters.AP-value ≤0.05 was considered statistically significant.
Morphological FindingsThe bacteria cultured from removed Jones tube were inoculated in the liquid medium,2.5% lysogeny broth (Becton Dickinson and Company,Sparks MD, USA) and shaking incubated overnight at 37℃.Then incubated bacteria sample was fixed 1:1 with 1%glutaraldehyde (JUNSEI, Tokyo, Japan) for 30min.A fixed sample of 6 μL was pipetted onto a 100 mesh copper grid with carbon-coated formvar film (EMS, Hartfield, USA) and incubated for 10min.Excess liquid was removed by blotting.The grid was washed twice by brief contact with 100 μL distilled water, followed by blotting to remove excess liquid.Next, the grid was placed on 30 μL of 1% uranyl acetate (SPI,Westchester, USA) for 12s.After removing excess liquid by blotting, the sample was examined with a transmission electron microscope (JEM-1200EX II, JEOL, Tokyo, Japan).
RESULTS
Seventy-one patients (81 eyes) were included in this study.The mean age was 62.5±10.7y (range, 24-81y).There were 47 female patients (66.2%).The mean Jones tube removal period was 41.1±41.0mo (range, 1-153mo) after surgery.Of the 81 eyes studied, Jones tube was removed in 23 eyes within 1y, in 38 eyes 1y or more but less than 5y, in 11 eyes 5y or more but less than 10y, and in 9 eyes 10y or more than 10y (Table 1).The causes of Jones tube removal were patient’s discomfort,infection or inflammation and tube malposition including migration.The tube was removed in 17 eyes (21.0%) due toocular discomfort such as pain, foreign body sensation, and itching; in 20 eyes (24.7%) due to infection or inflammation,and in 44 eyes (54.3%) due to tube migration or malposition(Table 2).
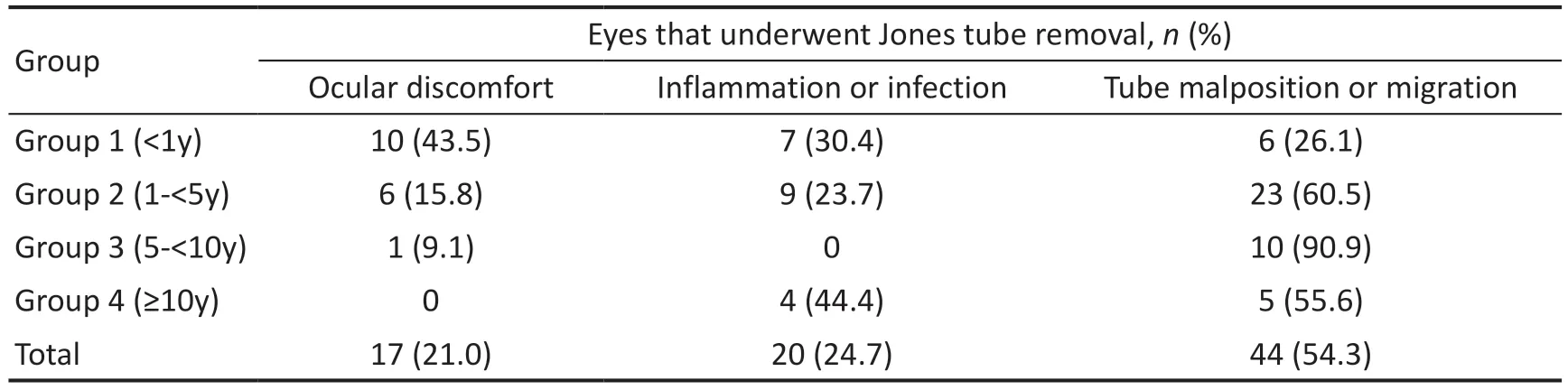
Table 2 Causes of Jones tube removal

Table 3 Cultured organisms found in Jones tubes after lacrimal bypass surgery according to the duration of tube removal
Among the 81 eyes, bacteria were isolated from 69 eyes(85.2%).Gram-positive bacteria in 49 eyes (71.0%) and Gram-negative bacteria in 20 eyes (29.0%).Among the cultured bacteria,Staphylococcus aureus(S.aureus) was the most common bacterium (28 eyes, 40.6%) followed byPseudomonas aeruginosa(P.aeruginosa, 8 eyes 11.6%).Table 3 shows the culture pattern according to the duration of tube removal.When comparing each group divided by the implanted period, Gram-positive bacteria were found more often than Gram-negative bacteria in the group within 10y of lacrimal bypass surgery withS.aureusbeing the most common bacterium.However, more than 10y after the surgery,Gram-negative bacteria were more significantly found than Gram-positive bacteria comparing the whole group frequency(Fisher’s exact test,P=0.035).AndProteusmirabilis(P.mirabilis) was the most common bacterium in the same number asS.aureusin Jones tube removed 10y after surgery(Figure 1).
In addition, 6 (7.40%) of the 81 eyes showed fungi such asTricosporon inkin(1 eye),Alternaria(1 eye),Aspergillus flavius(1 eye) andCandida parasilosis(3 eyes).
The antibiotic sensitivity test showed that 89.3% ofS.aureushad penicillin resistance and 46.4% ofS.aureuswere MRSA.S.aureuswas sensitive to trimethoprim/sulfamethoxazole (TMP/SMX) and vancomycin, whereas piperacillin, amikacin, and gentamicin inP.aeruginosa.All ofP.mirabilisin the Jones tubes implanted for more than 10y was sensitive to gentamicin,TMP/SMX, amikacin, and imipenem.Overall, vancomycin is sensitive toS.aureusandStreptococcus pneumoniae(S.pneumoniae), compared withP.aeruginosaandP.mirabilisresponded to amikacin.TMP/SMX showed sensitivity toS.aureus,S.pneumoniae, andP.mirabilis(Table 4).
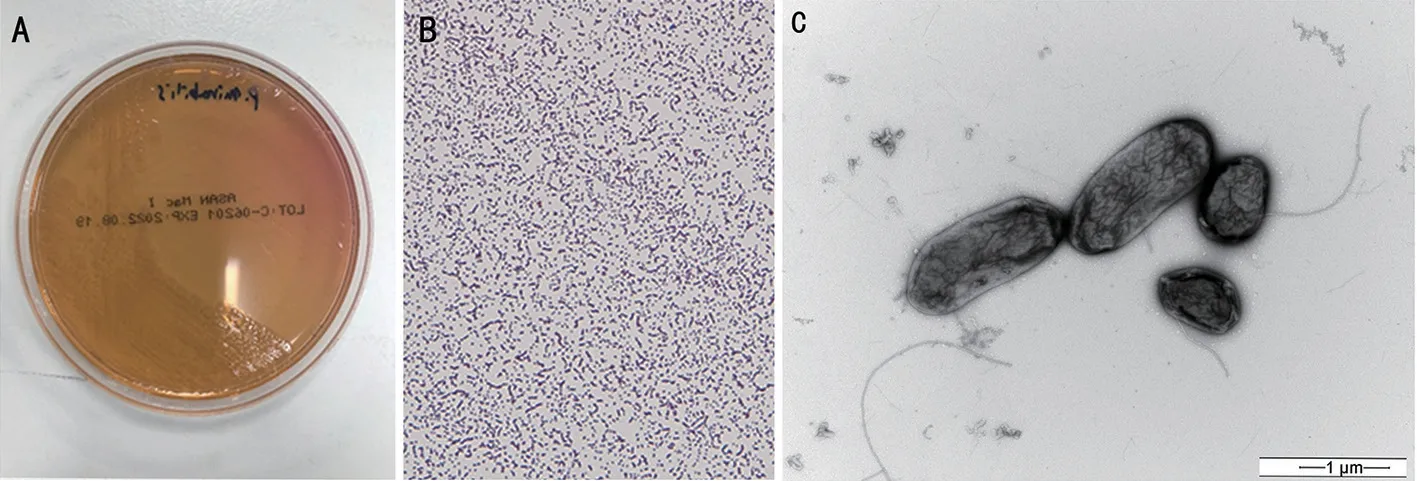
Figure 1 Morphological findings of P. mirabilis pathogens cultured in a Jones tube removed Colonial morphology, cell morphology and transmission electron microscophic morphology of P. mirabilis. P. mirabilis was cultured in removed Jones tube.A: The colonical morphology of P. mirabilis cultured in Macconkey agar medium.In this medium, the bacteria forms distinctive colonies different from the swarming colonies found in blood agar.B: The appearance of P. mirabilis after Gram staining with an optical microscope.P. mirabilis is gram negative bacterium.A pale reddish stained bacteria was distributed in pairs in optical microscope image (×400).C: The appearance of P. mirabilis using a transmission electron microscope.The bacteria showed a rod shape and had a few peritricheous flagella (Swimmer cell type).The average length of the bacteria was 1.5 μm (negative stain, original bar length: 1 μm, ×20 000). P. mirabilis: Proteus mirabilis.
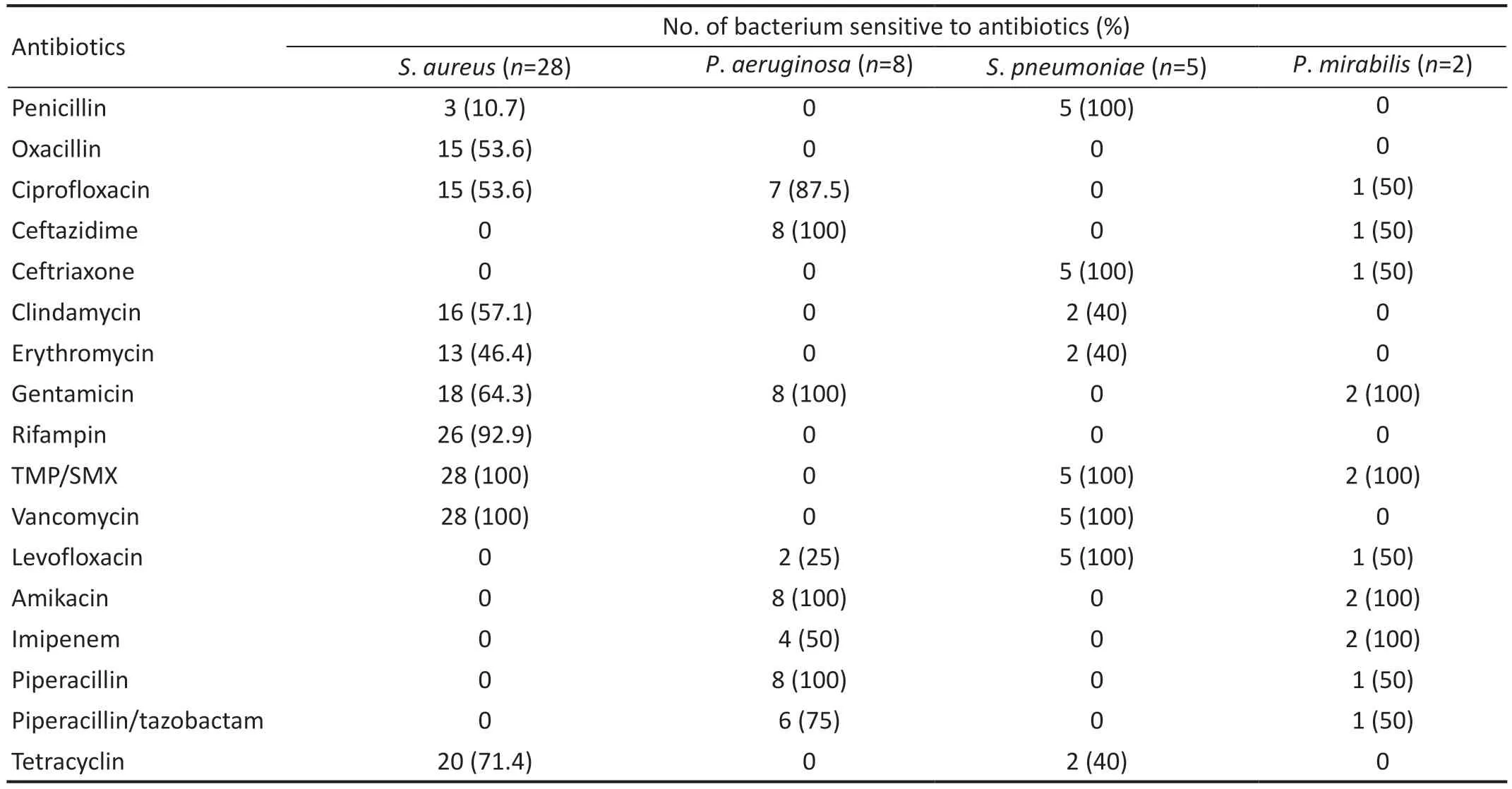
Table 4 Antibiotic sensitivity test of cultured organism from Jones tubes
DISCUSSION
The CDCR or lacrimal bypass surgery are used for treating disturbing epiphora due to a permanent failure of the canaliculi requiring a new passage for bypassing the lacrimal canaliculi and sac.Since its first description by Jones[1], it has been an acceptable and effective surgical technique with a high rate of surgical success.However, there are various complications of lacrimal surgery caused by the tube such as extrusion,malposition, obstruction, infection, and discomfort[12].Among the complications, extrusion (5%-51%) and malposition (6%-33%) are the most common[13].This is consistent with the result of our study that the most common cause of tube removal is associated with the location of the tube (54.3%).
Inflammation including infection occurs approximately 10% in lacrimal bypass surgery showing a lower incidence compared with complications related to the location of the tube[12-13].However, it can lead to chronic inflammation of the conjunctiva, cornea, and lacrimal sac as well as serious complications such as endophthalmitis[14-16].Thus,it is important to investigate the pathogenic strains and their antibiotic sensitivity for prevention and treatment of inflammation related with an implanted Jones tube.We previously investigated the pathogens in cultured Jones tube and their antibiotic sensitivities for a few years, but there was some limitation of size of study and long term follow up period[11,17].Thus, we collected a larger number of cases compared to the previous study and then analyzed the microbiological spectrum and antibiotic sensitivity profile of extubated Jones tube following lacrimal bypass surgery.
Among the 81 eyes that we studied, bacteria were found in 69 cases (85.2%), fungi in 6 cases (7.40%) and no organism in 6 cases (7.40%).Similar to a previous study[11], gram-positive bacteria were more frequently found than gram-negative bacteria within 10y of lacrimal bypass surgery.However, after 10y, Gram-negative bacteria were more common than grampositive bacteria.It was statistically significant (Fisher exact test,P=0.035).
S.aureus, an independent pathogen, was the most common bacterium found in 28 eyes (40.6%).This result was consistent with that of previous studies[10,13,17].Kimet al[10]reported that all patients suffered from tube infection were diagnosed with MRSA infection.Limet al[13]reported that all of the infection of Jones tube were caused byS.aureus.
But, there is a difference from our previous study.In previous study,P.mirabiliswas isolated most frequently after 10y of lacrimal bypass surgery[11].But in this study,S.aureusandP.mirabiliswas isolated in the same number after 10y of lacrimal bypass surgery.So,S.aureuswas the most common bacteria in all periods in present study.Thus, if a person who underwent lacrimal bypass surgery shows signs of tube associated inflammation, regardless of the tube removal period,S.aureusshould be considered as the primary pathogen for treatment.According to the antibiotic sensitive test, 89.3% ofS.aureuswere resistant to penicillin and 46.4% ofS.aureusto oxacillin(MRSA).So, vancomycin is an effective antibiotic for tube associated infection.However, in patients who have undergone lacrimal bypass surgery over 10 years ago, if vancomycin treatment is ineffective, the possibility of Gram negative bacteria includingP.mirabilisinfection should be considered.P.aeruginosawas the second most common bacterium found in 8 eyes (11.6%).And most of the gram-negative bacteria wasP.aeruginosa.In the antibiotic sensitivity test,P.aeruginosawas found to be susceptible to gentamicin,amikacin, ceftazidime and piperacillin.So, based on our study results, aminoglycoside antibiotics (gentamicin or amikacin),ceftazidime and piperacillin may be recommended as the second-line therapy.S.pneumoniae, which was identified in 5 eyes (7.25%) in this study, was the third most common bacteria.They were sensitive to TMP/SMX, vancomycin,levofloxacin and ceftriaxone.So, considering the antibiotics commonly used in ophthalmology, vancomycin is sensitive toS.aureusandS.pneumonia, compared withP.aeruginosaandP.mirabilisresponded to amikacin.
Recently, normal microbiota of eye and nose have been studied by using sequencing technology based on 16s rRNA.The most prevalent phyla in ocular surface areActinobacteria,Proteobacteria,andFirmicutus.And, at the genus level,Corynebacterium,Pseudomonas,Staphylococcus,Streptococcus,Acinetobacter,Propionibacterium,Agrobacterium,Sphinogomonas,CutibacteriumandEnhydrobacterare found in normal ocular surface[18-19].
And, at genus and species level, the normal nasal microbiota includeStreptococcus(S.pneumoniae,Streptococcus mitis),Staphylococcus(Staphylococcus saccharolyticus,Staphylococcus epidermidis,Staphylococcus capitis,S.aureus),Moraxella(Moraxella catarrhalis) andHaemophilus(Haemophilus influenza)[20].We found that normal ocular and nasal flora such asCorynebacterium,Staphylococci,Streptococcus,Acinetobacter,Sphinogomonaswere identified in our culture test.And our culture test results showed a similar pattern of bacterial identification in other study[21].
Bacterial biofilms are serious global health concern due to their abilities to tolerate antibiotics, host-defence systems and other external stresses[22].Therefore, an increasing number of diseases including ocular infection have been suggested to be biofilm related[23-24].As other medical devices, Jones tube and lacrimal stent may provide with a surface for biofilm formation[24-27].Parsaet al[25]demonstrated the presence of bacterial biofilms in culture-negative Jones tube as a cause of chronic infection.Balikoglu-Yilmazet al[26]reported that 90%of lacrimal stent removed 8wk after dacryocystorhinostomy revealed the presence of biofilm with cocci and/or rod shape bacteria.Kimet al[27]succeeded in making a biofilm on the lacrimal stent withS.aureusandP.aerugionosa.Although there is a question whether the presence of biofilm is the cause of the infection, it is important to find out the pathogen to from biofilm and their antibiotic sensitivity due to its difficulty of treating biofilm related infection[22,28].Since some of the bacteria found in our study can form biofilm[27], our study results may help preventing biofilm related infection.
Normal ocular surface include 65 different fungal genera includingAspergillus,Setosphaeria,Malassezia,Haematonectria,Candida etc[28].In our study, six eyes(7.40%) were found in fungus,Candida parasilosis(3 eyes),Aspergillus flavius(1 eye),Tricosporon inkin(1 eye), andAlternaria(1 eye).So if various antibiotics do not respond to treatment, it is necessary to consider infection caused by fungi,especiallyCandidaspecies.In this case, first of all, topical eye drops such as amphotericin B 0.15%, natamycin 5%,voriconazole 1% and systemic administration of antifungal drug series like azoles are recommended[29].
In conclusion, this study identified various strains in the culture of Jones tube after lacrimal bypass surgery and their antibiotic sensitivity.S.aureus,P.aeruginosa,S.pneumoniae,P.mirabiliscan lead to Jones tube related infection.And 46.4%ofS.aureuswere MRSA.For antibiotics commonly used in ophthalmology, vancomycin is sensitive toS.aureusandS.pneumoniae, compared withP.aeruginosaandP.mirabilisresponded to amikacin.TMP/SMX showed sensitivity toS.aureus,S.pneumoniaeandP.mirabilis.The results of this study will help prevent lacrimal tube related infection and use antibiotics properly.Furthermore, our study will serve a potential role in the development of special functional lacrimal tubes such as the biofilm inhibitory or antibiotic drug-releasing lacrimal tubes.
ACKNOWLEDGEMENTS
Conflicts of Interest: Park BH,None;Kim HK,None;Jo YJ,None;Lee JS,None.
CORRIGENDUM
Nintedanib induces apoptosis in human pterygium cells through the FGFR2-ERK signalling pathway
Yan Gong,Yan-Hong Liao,Quan-Yong Yi,Meng Li,Li-Shuang Chen,Yan-Yan Wang(Int J Ophthalmol2023;16(4):505-513, DOI: 10.18240/ijo.2023.04.03)
The authors wish to add the foundations as follow:
Foundations:Supported by Zhejiang Provincial Health Science and Technology Plan (No.2021PY073); Traditional Chinese Medicine Science and Technology Project of Zhejiang Province (No.2021ZB268); Zhejiang Medical and Health Science and Technology Plan (No.2023KY1141); Science and Technology Project in Agriculture and Social Development Field of Yinzhou District (No.2021AS0058).
The authors apologize for any inconvenience caused by this error.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel pathogenic splicing mutation of RPGR in a Chinese family with X-linked retinitis pigmentosa verified by minigene splicing assay
- Vault predicting after implantable collamer lens implantation using random forest network based on different features in ultrasound biomicroscopy images
- Multiple evanescent white dot syndrome relapse following BNT162b2 mRNA COVID-19 vaccination
- Acute micro-macular hole associating with extensive intraoperative rotation of implantable collamer lens without ophthalmic viscosurgical device assistance: a case report
- Effectiveness of conjunctival bleb scarring by knockdown of heat shock protein 47 in rat model
- Effect of miR-27b-3p and Nrf2 in human retinal pigment epithelial cell induced by high-glucose
