Outpatient hybrid endoscopic submucosal dissection with SOUTEN for early gastric cancer, followed by endoscopic suturing of the mucosal defect: A case report
Renma Ito, Kazuhiro Miwa, Yutaka Matano
Abstract
Key Words: Outpatient treatment; Hybrid endoscopic submucosal dissection; Multifunctional snare; Early gastric cancer; Endoscopic suturing; Case report
INTRODUCTION
Endoscopic submucosal dissection (ESD) is becoming increasingly common for early gastric cancer[1]. ESD requires more advanced techniques and a longer duration of treatment than endoscopic mucosal resection and is potentially associated with more complications. Hybrid ESD performed with multifunctional snare (SOUTEN, Kaneka Medics, Tokyo, Japan)(Figure 1), has been reported to be clinically effective for endoscopic treatment of colorectal lesions and to reduce the duration of treatment[2-4]. Moreover, endoscopic suturing of post-ESD mucosal defects can reduce complications, such as bleeding and perforation[5-7].
Herein, we report a case of early gastric cancer in which outpatient hybrid ESD with SOUTEN was performed in an elderly man with a history of delirium during hospitalization, after which the mucosal defect was sutured endoscopically to reduce complications.
CASE PRESENTATION
Chief complaints
No complaints.
History of present illness
An 86-year-old male diagnosed with early gastric cancer confirmed by esophagogastroduodenoscopy and biopsy was referred to our hospital for ESD. The medical history included Alzheimer’s disease, chronic kidney disease, and dyslipidemia.
History of past illness
The patient’s past medical history was non-contributory.
Personal and family history
The patient had no family history of gastric cancer and was neither a smoker nor a drinker.
Physical examination
Physical examination did not reveal abnormalities and the Eastern Cooperative Oncology Group performance status score was 1, which was relatively good.
Laboratory examinations
Laboratory examination results were within the normal range.
Imaging examinations
Esophagogastroduodenoscopy revealed a 10-mm flat, depressed lesion on the posterior wall of the gastric antrum that was identified as a demarcation line and had an irregular microvascular pattern detected by magnifying endoscopy with narrow-band imaging (Figure 2). The lesion had already been diagnosed as gastric cancer on the basis of a biopsy performed in a previous hospital.
FINAL DIAGNOSIS
The lesion was believed to be mucosal; therefore, the diagnosis of early gastric cancer was further confirmed at our hospital, where ESD was deemed necessary.
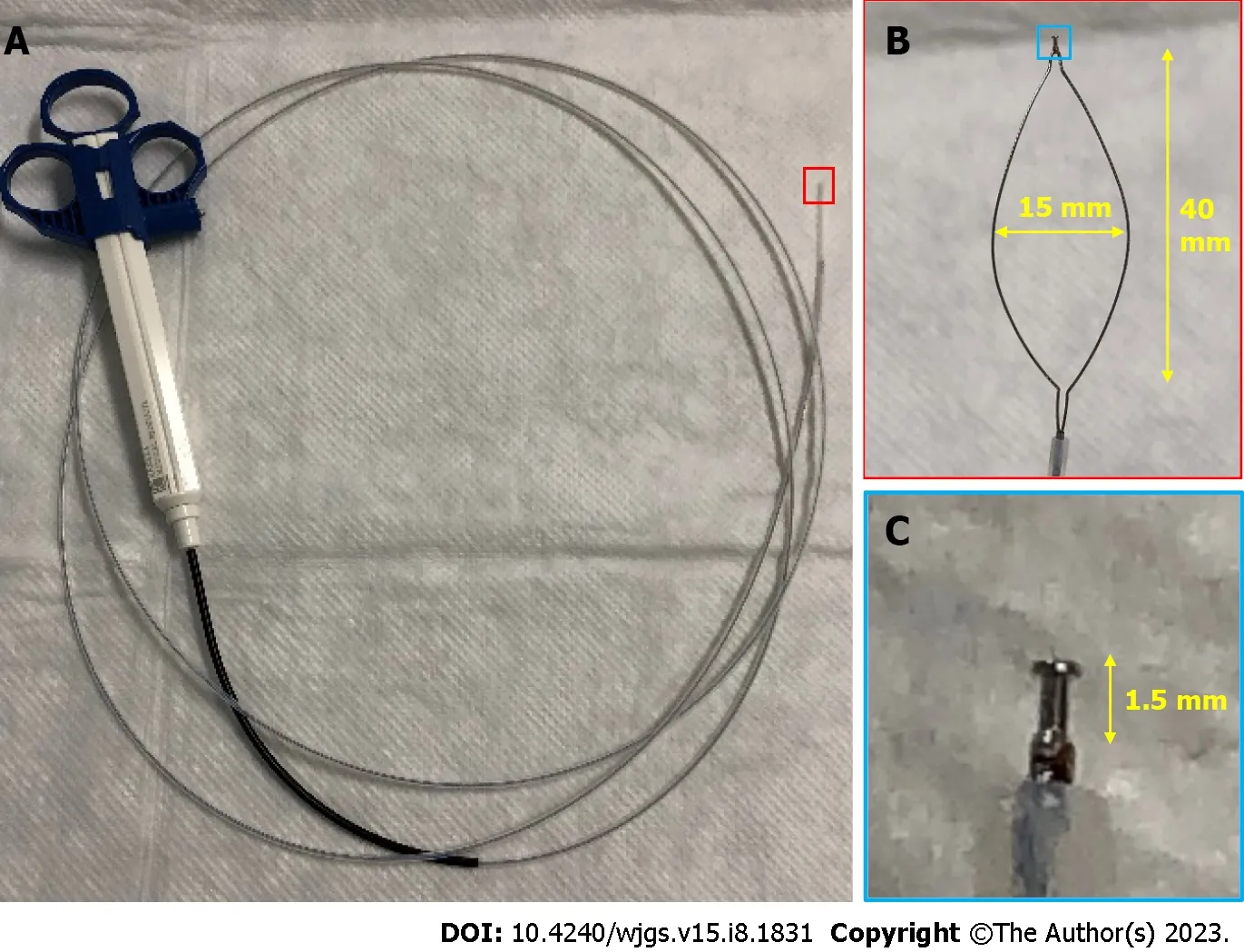
Figure 1 Details of the SOUTEN device, a multifunctional snare. A: Full view of the SOUTEN device; B: The long diameter of the snare is 40 mm, and the short diameter of the snare is 15 mm; C: A 1.5-mm needle knife with a knob-shaped tip is attached to the top of the snare.

Figure 2 Endoscopic view of the 10-mm flat-depressed lesion on the posterior wall of the gastric antrum. A: Distant view of the lesion under white-light imaging; B: Non-expansion view of the lesion using magnifying endoscopy with narrow-band imaging; C: Weak-expansion view of the lesion using magnifying endoscopy with narrow-band imaging; D: Strong-expansion view of the lesion using magnifying endoscopy with narrow-band imaging.
TREATMENT
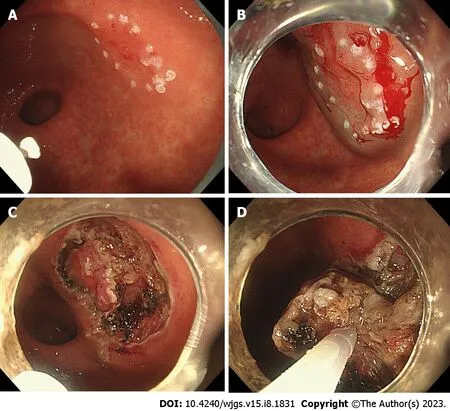
Figure 3 Hybrid endoscopic submucosal dissection process with SOUTEN. A: A knife attached to the top of the snare is used to mark the lesion; B: A mixture of hyaluronic acid and saline is injected into the submucosa around the lesion; C: A knife attached to the top of the snare is used to dissect the submucosal around the lesion; D: Resection of the lesion with the snare.
The patient was unaware of the early gastric cancer diagnosis due to the symptoms of Alzheimer’s disease. The patient’s family wanted him to undergo ESD; however, they refused hospitalization due to a history of delirium before admission.Therefore, we planned outpatient hybrid ESD with SOUTEN to reduce the duration of treatment, followed by endoscopic suturing of the post-ESD mucosal defect to reduce complications. Informed consent was obtained from all patients and their families. The patient was administered vonoprazan (20 mg/d) for 8 wk from the day of ESD. We performed an outpatient hybrid ESD for early gastric cancer with SOUTEN (Figure 3) and endoscopically sutured the post-ESD mucosal defect using strings and clips (Figure 4). The procedure time was 62 min. We instructed the patient’s family that the patient should only drink fluid on the day of outpatient ESD and eat soft food the next day. Regular meal consumption was resumed 1 wk after outpatient ESD.
OUTCOME AND FOLLOW-UP
No complications were observed, including delirium, and follow-up after the procedure was uneventful. Histopathological examination of the resected lesion revealed well-differentiated adenocarcinoma with mucosal depth and no lymphatic or vascular invasion. The margins were negative, indicating complete resection of the lesion. One month after outpatient ESD, esophagogastroduodenoscopy revealed that the ulcer had almost healed and only a part of the ulcer floor was visible (Figure 5).
DISCUSSION
To the best of our knowledge, this is the first report of outpatient hybrid ESD performed for early gastric cancer with SOUTEN and endoscopic suturing of a post-ESD mucosal defect. Treatment was successful and no complications were observed. Hybrid ESD has been reported to achieve a shorter procedure time than ESD with similaren-blocresection rates and adverse events for colorectal lesions[8]. SOUTEN, a device specialized for hybrid ESD, is a multifunctional snare with two features (a high-frequency knife and a snare). Hybrid ESD with SOUTEN is clinically useful for the treatment of colorectal epithelial tumors[2-4]. However, for gastric lesions, it is useful to reduce endoscopic treatment time in basic research, not clinical research[9]. Although we have shown the clinical usefulness of hybrid ESD with SOUTEN for early gastric cancer in this case report, further research is recommended to elucidate its clinical application in gastric lesions.
We believe that hybrid ESD with SOUTEN and endoscopic suturing is advantageous for smaller lesions as in this case,but disadvantageous for large lesions because snaring and suturing large lesions is difficult. Additionally, such treatment might be more difficult for gastric lesions than colorectal lesions because snaring is difficult in some parts such as the angle in the stomach.
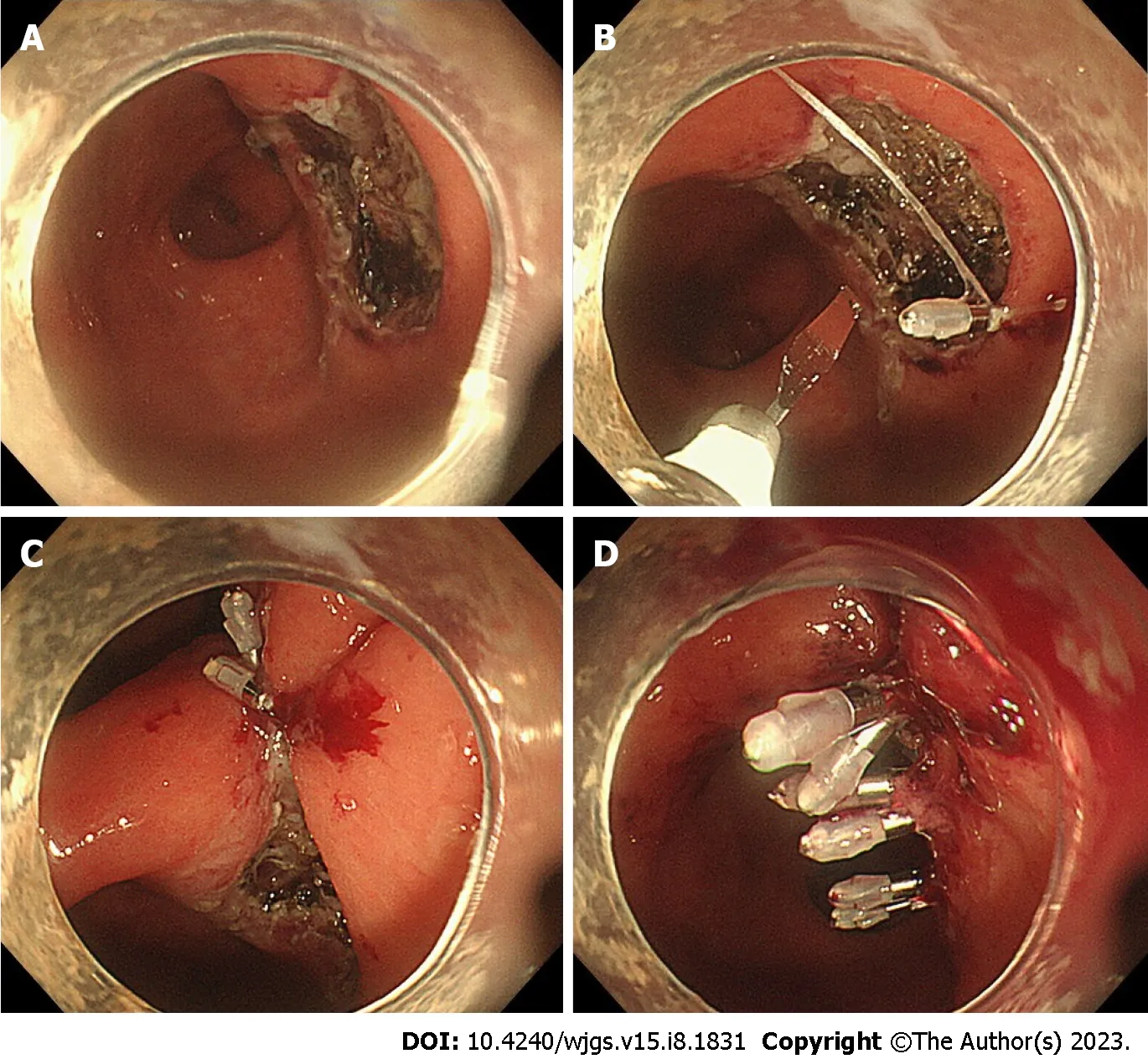
Figure 4 Endoscopic suturing process for a mucosal defect after endoscopic submucosal dissection. A: Post-endoscopic submucosal dissection mucosal defect in the posterior wall of the gastric antrum; B: A clip with a string attached to the tip is first attached to the anal aspect of the mucosal defect, and an additional clip is attached to the oral aspect of the mucosal defect while sandwiching the string; C: Bring both ends of the mucosa closer by pulling the string out of the mouth; D: Suturing the mucosal defect completely by attaching additional clips to both sides of the mucosal defect and finally burning off the string with the knife of SOUTEN.
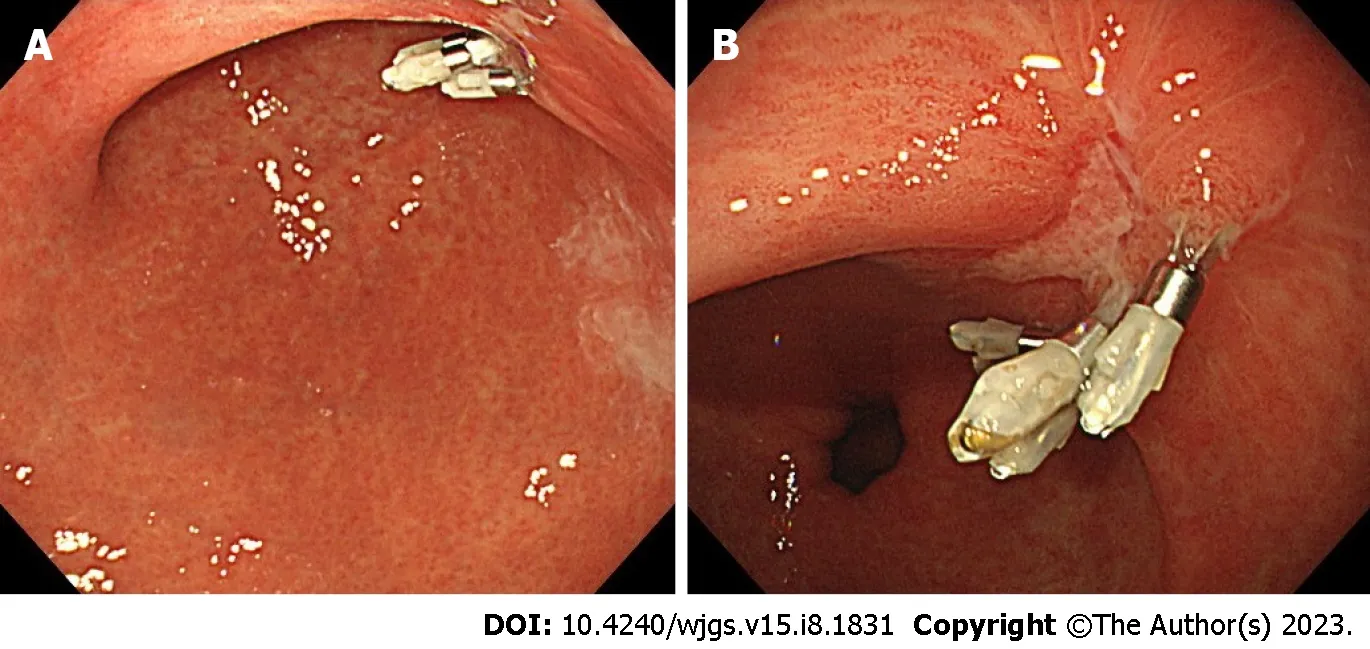
Figure 5 Endoscopic view of the ulcer one month after endoscopic submucosal dissection. A: Distant view of the ulcer; B: Close-up view of the ulcer.
The post-ESD mucosal defect was sutured endoscopically to reduce post-ESD bleeding[6] and prevent perforation[7].In a previous report on gastric ESD, perforation occurred in 2.8% of patients and delayed bleeding that required endoscopic hemostasis occurred in 6.2%[10]. Endoscopic suturing of mucosal defects after ESD may prevent these complications. Therefore, it is desirable to endoscopically suture mucosal defects after ESD to reduce the occurrence of complications, particularly when performing outpatient ESD. Although there are some ways to suture mucosal defects using endoscopy, we believe that endoscopic suturing using a clip with a string[11] is simple and useful; therefore, we sutured the mucosal defects using this method.
Although the usefulness and safety of outpatient ESD for gastric lesions has been reported, some complications centered on delayed bleeding occurred in 1.9%-5.7%[12,13]. We believe that minimizing the occurrence of complications during outpatient ESD is important. Therefore, we used vonoprazan, which has been reported to prevent bleeding from ED-induced gastric ulcers[14]. Endoscopic suturing of the mucosal defect and the use of vonoprazan for ESD-induced gastric ulcers might be important in reducing complications in outpatient ESD.
We performed endoscopic treatment for early gastric cancer in an 86-year-old patient. The treatment of cancer in elderly patients is challenging because it is unclear whether these patients have a positive prognosis. Furthermore, elderly people are prone to developing delirium during hospitalization. Although the patient experienced psychological problems in the present case, his physical condition was relatively good. Outpatient ESD is useful for treating early gastric cancer and preventing delirium in elderly patients. We believe that endoscopic treatment for early gastric cancer in elderly patients with good physical status is beneficial and that outpatient endoscopic treatment is especially useful for elderly patients.
CONCLUSION
Outpatient hybrid ESD for early gastric cancer using SOUTEN followed by endoscopic suturing of post-ESD mucosal defects was safe and useful. This may be particularly important for outpatient endoscopic treatment.
ACKNOWLEDGEMENTS
The authors thank the staff of the endoscopy room at the Komatsu Municipal Hospital.
FOOTNOTES
Author contributions:Ito R, Miwa K, and Matano Y conceived the idea of the treatment in this case; Ito R drafted the original manuscript;all authors reviewed the manuscript draft and revised it critically.
Informed consent statement:Informed consent for inclusion in the study or equivalent was obtained from the patient’s family.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
与表8亲密关系丧失组情况对比发现,死亡凸显与亲密关系丧失对高自尊被试职业认同的影响有所不同,二者均显著降低了高自尊者的职业承诺、职业价值观和职业认知水平,但除此之外,死亡凸显还显著降低了高自尊者的职业情感,而亲密关系丧失无此效应。
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Japan
ORCID number:Renma Ito 0000-0001-7706-166X; Kazuhiro Miwa 0000-0002-5486-9137; Yutaka Matano 0000-0003-4933-5381.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
 World Journal of Gastrointestinal Surgery2023年8期
World Journal of Gastrointestinal Surgery2023年8期
- World Journal of Gastrointestinal Surgery的其它文章
- Is endoscopic mucosal resection-precutting superior to conventional methods for removing sessile colorectal polyps?
- Knowledge, attitude, and practice of monitoring early gastric cancer after endoscopic submucosal dissection
- Changing trends in gastric and colorectal cancer among surgical patients over 85 years old: A multicenter retrospective study, 2001-2021
- Enhanced recovery nursing and mental health education on postoperative recovery and mental health of laparoscopic liver resection
- Effects of ultrasound monitoring of gastric residual volume on feeding complications, caloric intake and prognosis of patients with severe mechanical ventilation
- Risk factors and their interactive effects on severe acute pancreatitis complicated with acute gastrointestinal injury
