Evaluation of Serum Vitamin D Concentration and Blood Eosinophil and Basophil Counts in Patients With Vitiligo: A Cross-sectional Study From Rafsanjan and Zarand, Iran
Razieh Taghizadeh Ghavamabadi, Reihaneh Pishgooie, Shadi Behfar,Mohammad Mohsen Taghavi, Abdolreza Babaee, Zahra Taghipour,*
1 Department of Anatomy, School of Medicine, Rafsanjan University of Medical Sciences, Rafsanjan, Kerman 37718175911, Iran;
2 Physiology-Pharmacology Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Kerman 37718175911, Iran; 3 Department of Internal Medicine, Rafsanjan University of Medical Sciences, Rafsanjan, Kerman 37718175911, Iran; 4 Department of Dermatology, Rafsanjan University of Medical Sciences, Rafsanjan, Kerman 37718175911, Iran.
Abstract
Keywords: autoimmunity, pigmentation disorders, vitiligo, 1,25-dihydroxyvitamin D3
Introduction
Vitiligo is a pigmentary disorder caused by the destruction of functional melanocytes.This disorder is distinguished by depigmented spots in the epidermis that may increase in size and change in shape over time.The depigmented spots can appear anywhere on the skin, but the most common sites are in genital and sun-exposed areas such as the hands and face.1
Vitiligo is an autoimmune disorder that affects 1% to 4% of the world population.This disorder impresses the epidermal melanocytes and neural crest-derived melanocytes and spreads to different parts of the body such as the hair follicles and eyes.2
Various mechanisms of melanocyte degeneration in vitiligo have been proposed.According to one theory, nerve endings in the skin release a toxic substance that can degenerate melanocytes.Another theory emphasizes the self-nourishment of melanocytes.A third theory states that vitiligo is an autoimmune disease in which the immune system attacks the host’s own tissues and cells.This recent theory has been discussed in studies showing close relationships between vitiligo and other autoimmune disorders.3
Some autoimmune diseases, including rheumatoid arthritis and diabetes, are related to the reduction of vitamin D.Several studies have shown that vitamin D deficiency may stimulate the development of an autoimmune disease4and have indicated that vitamin D has a role in the pathogenesis of vitiligo.5Vitamin D is a steroid hormone that has different impacts on vitamin D receptor-expressing cells such as T and B lymphocytes, macrophages,and dendritic cells.6
Although vitamin D is obtained through diet and dietary supplements, its main source is synthesis within the skin induced by ultraviolet rays.In this reaction, vitamin D precursors change into vitamin D through solar ultraviolet rays.7
1,25-Dihydroxy vitamin D (1,25[OH]2D3) is a secosteroid hormone and an active form of vitamin D that has functions such as regulation of calcium and bone metabolism, control of cell proliferation and differentiation,and immune activity.Because of its widespread functions,vitamin D is applied in the treatment of several diseases including secondary hyperparathyroidism, osteoporosis,psoriasis, and vitiligo.8
25-Hydroxy vitamin D (25[OH]D), which has a halflife around 10 to 40 days, is a stable index for evaluation of the vitamin D concentration.9
Some studies have shown that the roles of eosinophils and basophils are obvious in skin diseases, whereas these cells are not observed under physiologic conditions.Therefore, evaluating the number and function of these cells provides an opportunity for better diagnosis of skin disorders.10-11
Basophils have several roles in the pathophysiology of autoimmune diseases such as lupus and rheumatoid arthritis, and eosinophils are involved with autoimmune diseases.12Eosinophils have strong cytotoxic properties and may contribute to organ and cell destruction in autoimmune inflammation.13
In this study, we evaluated the role of vitamin D in vitiligo by measuring the serum vitamin D concentration and blood eosinophil and basophil counts in patients with vitiligo.The findings of this study may improve our knowledge of the pathophysiology of vitiligo and thus lead to improved treatment methods.
Methods and materials
Study groups
In this cross-sectional study, based on a study by Lajevardiet al.,14we evaluated 30 patients aged 20 to 40 years with vitiligo.The patients were chosen from among those who were referred to Aliebn Abitaleb Rafsanjan and Sina Zarand hospitals in 2016 and 2017.The control group comprised 30 healthy people chosen among students of the Rafsanjan University of Medical Science.14Finally,the case group comprised 14 men and 16 women and the control group comprised 10 men and 20 women.
This study was carried out with the permission of the Ethics Council of Rafsanjan University of Medical Sciences (IR code: RUMS.REC.1396.3), and was performed in adherence to the Helsinki declaration.All patients provided written informed consent.
In both groups, people who received any medications or treatments such as topical or systemic calcium or vitamin D, systemic steroids, cholesterol-lowering medicine, weight loss medicine, thiazide diuretics, or phototherapy in the last 6 months; women who were pregnant or lactating; smokers; patients with other autoimmune diseases; and patients with kidney disease were excluded from the study.15
After obtaining informed consent, blood samples were obtained to evaluate the serum vitamin D concentration.About 5 mL of venous blood was taken from all participants in the present study.From each blood sample, 2 mL was used to determine the eosinophil and basophil counts,and about 3 mL was centrifuged and the serum isolated.The serum vitamin D concentration was measured by enzyme-linked immunosorbent assay according to the manufacturer’s instructions (Ideal Tashkhis Atieh, Iran).
All information in the present study was recorded in a checklist that included two parts.The first part contained the participants’ basic and demographic information and was completed by a doctor.The second part contained the participants’ serum vitamin D concentrations and blood eosinophil and basophil counts and was completed by a researcher.
Eosinophil and basophil counts
To obtain the eosinophil and basophil counts, one drop of blood was placed on a slide by a capillary tube and a blood smear was formed.After drying at room temperature, the slide was fixed with methanol and stained by Giemsa for 21 minutes.The numbers of cells were then determined using a cell counter device.
Statistical analysis
The collected information was analyzed using SPSS Version 20 (IBM Corp., Armonk, New York).Quantitative data are reported as mean ± standard deviation, and qualitative information are reported as a percentage (%).The homogeneity of the two groups in terms of age and sex was checked via at-test and chi square test, respectively, at the beginning of the study.The normality assumption was analyzed using the Kolmogorov-Smirnov test and the skewness and kurtosis indexes.Because this test result was not significant (P> 0.05) and both the skewness and kurtosis indexes were within the range of 1 to -1, the normality assumption was confirmed.For comparison of the average of quantitative variables between the groups, we performed an independent t-test at the end of the study.APvalue of < 0.05 was considered statistically significant in all tests.
Results
The case group comprised 30 patients with vitiligo ranging in age from 20 to 40 years who were chosen from among patients referred to Aliebn Abitaleb Rafsanjan and Sina Zarand hospitals.The control group comprised healthy people who were sex- and age-matched with patients in the case group.
The case group constituted 14 men and 16 women, and the control group constituted 10 men and 20 women.A comparison of the two groups showed that they were matched in terms of sex (P= 0.2).The mean age of all participants in this study was 31.3 ± 0.6 years (case group,31.1 ± 0.9 years; control group, 31.6 ± 0.8 years), with a range of 20 to 36 years in both groups.The mean ages were not significantly different between the case and control groups (P= 0.70).
Serum vitamin D concentration
The mean serum vitamin D concentration in the case and control groups was 25.24 ± 1.90 and 31.82 ± 1.60 ng/mL,respectively, with a statistically significant difference (P=0.01) (Fig.1A).
The serum vitamin D concentration was also compared between all participating men and women.Although the mean serum vitamin D concentration was lower in women(27.60 ± 1.60 ng/mL) than in men (29.89 ± 2.08 ng/mL), the difference was not statistically significant (P= 0.4) (Fig.1B).
Within the case group, the mean serum vitamin D concentration was significantly lower in women than in men(21.38 ± 1.90vs.29.65 ± 3.30 ng/mL, respectively;P=0.03) (Fig.1C).
The serum vitamin D concentration was also compared between women in the case and control groups and between men in the case and control groups.The results showed that the serum vitamin D concentration was significantly lower in women with than without vitiligo (P= 0.001) but was not significantly different between men with and without vitiligo (P= 0.89) (Fig.1D).
Eosinophil count
The eosinophil count was compared between the case and control groups.The results showed that the mean eosinophil count was lower in the case group than in the control group (181.30 ± 16.97vs.204.60 ± 23.11 cells/µL, respectively), but the difference was not statistically significant(P= 0.4) (Fig.2A).
Basophil count

Figure 1.Comparisons of serum vitamin D concentrations in various subgroups.(A) Comparison between case group (n = 30) and control group (n = 30).*P < 0.05.(B) Comparison between all participating men (n = 24) and women (n = 36).(C) Comparison between women(n = 16) and men (n = 14) in case group.*P < 0.05.(D) Comparison of women between case and control groups (n = 24) and of men between case and control groups (n = 24).*P < 0.05.
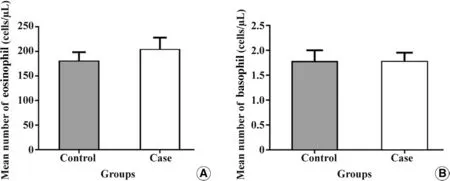
Figure 2.Comparisons of eosinophil and basophil counts in case and control groups.(A) Eosinophil count.(B) Basophil count.
The basophil count was also compared between the case and control groups.The results showed that the mean basophil count was almost identical between the case and control groups (1.70 ± 0.19vs.1.70 ± 0.18 cells/µL, respectively) with no significant difference (P=1.0) (Fig.2B).
Discussion
Vitiligo is an autoimmune disease that disrupts melanocyte function in the skin and leads to depigmentation.Vitamin D is a hormone that is made in the skin and is responsible for pigmentation.Low levels of vitamin D have been reported in some autoimmune diseases.16
In the present study, 30 people with vitiligo were matched in terms of age and sex with 30 healthy people.The results showed that the serum vitamin D concentration was significantly lower in the case group than in the control group.
Additionally, comparison of the serum vitamin D concentration between women and men with vitiligo showed that the mean serum concentration was significantly lower in women than in men.The serum concentration was also lower in women than in men in the control group, but the difference was not statistically significant.Our results are consistent with those reported by Mahmmod and Ismael.17These authors attributed the decreased serum concentration in women to the type of clothing women wear due to religion and culture in Iraq.The coverage conditions in Iran are very similar to those in Iraq.17In our study, the mean serum concentration of vitamin D was significantly lower in women than in men with vitiligo; however, although the mean serum concentration was also lower in women than in men among the whole population, the difference was not statistically significant.
Low serum vitamin D concentrations have also been reported in other autoimmune diseases such as systemic and cutaneous lupus erythematosus, psoriasis, and inflammatory bowel disease.18
In 2012, Xuet al.19analyzed the vitamin D concentrations in patients with vitiligo in China.They found that the difference in the serum vitamin D concentrations between the case and control groups was not statistically significant, demonstrating no correlation between the serum vitamin D concentration and vitiligo in China.The significant difference in the serum vitamin D concentration between the case and control groups in our study is inconsistent with the findings reported by Xuet al.19
In 2019, Alshiyabet al.20studied 100 patients with vitiligo and measured their serum vitamin D concentrations.The authors found that although the serum vitamin D concentration was lower in the case than control group,the difference was not statistically significant.20
Additionally, in 2014, Lajevardiet al.14evaluated the serum vitamin D concentrations in 30 people with vitiligo and 30 healthy people and found that the serum concentration was lower in women than in men.This reduction may have been related to how Iranian women dress, which protects their skin surface from sunlight.This result of their study is consistent with our findings.However, Lajevardiet al.14also showed that the serum vitamin D concentration was significantly lower in men with than without vitiligo but was not significantly different between women with and without vitiligo; this finding is inconsistent with our study.
With respect to epidemiological evidence of vitamin D deficiency in adults with vitiligo, Zhanget al.21evaluated the vitamin D concentration in children with vitiligo.They studied 114 patients and 100 healthy people and reported that the serum vitamin D concentration was lower in the case group than in the control group.They demonstrated that age was an independent factor that can impact the serum vitamin D concentration,which was significantly different in patients and healthy people of different ages.They also found no correlation between the serum vitamin D concentration and sex, duration of disease, type of vitiligo, location of skin lesion, disease stage, or family history.Their finding in terms of the significant reduction in the serum vitamin D concentration is consistent with our study.However,we found that sex was an effective factor and that the serum vitamin D concentration was lower in women than in men.This finding is inconsistent with the study by Zhanget al.,21although they studied children and not adults.
In 2015, Takciet al.22evaluated vitamin D metabolism in patients with vitiligo.They compared 44 patients with a mean age of 34 years and 43 control subjects with a mean age of 33 years.They reported that the serum 25(OH)D concentration was significantly lower in the patient group than in the control group,22whereas in 2019, Sanieeet al.23showed no significant difference in the vitamin D concentration between 98 patients with vitiligo (mean age of 30 years) and 98 control participants.
In 2016, Upala and Sanguankeo24performed a review of 383 articles involving 1,200 patients with vitiligo.Their meta-analysis showed a significant relationship between vitamin D insufficiency and vitiligo.They reported that further studies are needed to determine whether taking vitamin D supplements improves vitiligo in these patients.24Their results were consistent with the findings in our study.
In 2010, Silverberget al.25focused on the serum vitamin D concentration in autoimmune disease by evaluating 45 patients with vitiligo vulgaris.The patients were divided into three groups according to their serum vitamin D concentration.Serum vitamin D was found to be sufficient(>30 ng/mL) in 31.1% of patients, insufficient (<30 ng/mL) in 55.6% of patients, and deficient (<15 ng/mL) in 13.3% of patients.The authors showed that vitamin D deficiency was associated with an increased incidence of Fitzpatrick phenotype and with autoimmune disease, but not with age, sex, race, ethnicity, or family history of vitiligo.They concluded that a low vitamin D concentration is helpful in the assessment of autoimmune disease.25
In the present study, the eosinophil and basophil counts were calculated in the case and control groups.Although the eosinophil count was higher in the case than control group, the difference was not statistically significant.The limitation of the study was the few participants, which caused that basophil count was not significantly different between the case and control groups.
In 2020, Kolkhir et al.evaluated 1,613 patients with Chronic spontaneous urticaria and found eosinopenia and basopenia could associated with high disease activity and type II autoimmunity.26The findings in this case study were not consistent with our study results.
In 2016, Lang and Kaya27described a 60-year-old woman with diffuse erythematous papules surrounded by a white halo and a 10-year history of vitiligo lesions on the hands,arms, and legs.Laboratory tests, blood cell counts, and biochemical factors including thyroid function were normal.Histological evaluation of an erythematous papule showed dermatitis, including perivascular and interstitial infiltration of lymphocytes and eosinophils.The lesions completely disappeared after 2 weeks of antihistamine therapy.27The major limitation of the current study is the small sample size of this study, and results need to be verified by a large sample study.
In conclusion, our study findings suggest that the serum vitamin D concentration decreases in patients with autoimmune disease.This decrease in vitamin D might be a factor in the development of vitiligo or it may occur after vitiligo has become established.However, the eosinophil and basophil counts are not effective markers for vitiligo.Further studies of the serum vitamin D concentration are essential.
Acknowledgments
The authors thank Rafsanjan University of Medical Sciences for supporting this study.
- 国际皮肤性病学杂志的其它文章
- Transcription and Secretion of lnterleukin-1β and HMGB1 in Keratinocytes Exposed to Stimulations Mimicking Common lnflammatory Damages
- Dermoscopic Assessment of Pityriasis Versicolor: A Cross-Sectional Observational Study
- Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care?
- Basal Cell Carcinoma Excision Guided by Dermoscopy: A Retrospective Study in Macau
- The Role of Endoplasmic Reticulum Stress in Melanoma
- The Relationship Between Ultraviolet B and DNA Methylation in Skin Cancers

