粪便miRNA-92a表达与粪便隐血试验联合诊断结直肠癌的应用

[摘要]目的探讨粪便miRNA-92a表达与粪便隐血试验串联、并联对结直肠癌的诊断价值。方法选取2020年1月~2022年12月郴州市第一人民医院收治的100例结直肠癌患者为结直肠癌组和100例结直肠腺瘤患者为结直肠腺瘤组,另选取同期200例年龄、性别匹配的健康体检者为对照组。比较各组粪便miRNA-92a和粪便隐血试验结果,采用logistic回归分析结直肠癌发生的影响因素;分析miRNA-92a表达水平与结直肠癌发生的关系;比较结直肠癌组不同临床病理特点患者的粪便miRNA-92a表达差异;采用Spearman分析粪便miRNA-92a表达与结直肠癌病情的相关性;采用ROC曲线分析粪便miRNA-92a、粪便隐血试验及其串联、并联诊断对结直肠癌的诊断价值。结果各组粪便miRNA-92a表达水平、粪便隐血阳性率比较,均为结直肠癌组>结直肠腺瘤组>对照组(P<0.05);结直肠腺瘤患者粪便miRNA-92a高表达发生结直肠癌的风险是低表达患者的3.547倍;进展期腺瘤、多发息肉史、粪便miRNA-92a、粪便隐血试验阳性是结直肠癌发病的独立危险因素(P<0.05);结直肠癌组中,不同肿瘤直径、T分期、N分期、M分期、分化程度及是否有淋巴结转移的患者粪便miRNA-92a表达比较,差异均有统计学意义(P<0.05);粪便miRNA-92a表达与肿瘤直径、T分期、N分期、M分期、分化程度及淋巴结转移均呈正相关(P<0.05);粪便miRNA-92a、粪便隐血试验串联、并联试验诊断结直肠癌的曲线下面积分别为0.685、0.795;串联试验灵敏度较低,特异度较高,并联试验灵敏度较高,特异度较低。结论粪便miRNA-92a高表达可增加结直肠癌发生风险,与粪便隐血试验串联、并联试验可分别提高临床诊断的特异度、灵敏度。
[关键词]粪便;miRNA-92a;结直肠癌;粪便隐血试验
doi:10.3969/j.issn.1674-7593.2023.05.016
the Application of Fecal MiRNA-92a Expression Combined with Fecal Occult blood Testin the Diagnosis of Colorectal Cancer
Huang Haifen,He An,Xu Xiaoda,Li Ren**
The First People's Hospital of Chenzhou,Chenzhou423000
**Corresponding author:Li Ren;email:1455698997@qq.com
[Abstract]ObjectiveTo explore the diagnostic value of fecal miRNA-92a expression combined with fecal occult blood test in series or parallel for colorectal cancer.Methods100 patients with colorectal cancer(colorectal cancer group) and 100 patients with colorectal adenoma(colorectal adenoma group) who were admitted to Chenzhou NO.1 People's Hospital from January 2020 to December 2022 were selected,and another 200 healthy physical examination participants matched for age and gender during the same period were selected as the control group.The fecal miRNA-92a and fecal occult blood test results were compared among groups,logistic regression analysis was used to examine the influencing factors for colorectal cancer occurrence,the relationship between miRNA-92a expression level and colorectal cancer occurrence was analyzed,differences in fecal miRNA-92a expression among patients with different clinical and pathological features in the colorectal cancer group were compared,the correlation between fecal miRNA-92a expression and colorectal cancer severity was analyzed using Spearman correlation analysis,and the diagnostic value of fecal miRNA-92a,fecal occult blood test, and their combination for colorectal cancer diagnosis was analyzed using ROC curve analysis.ResultsThe expression levels of fecal miRNA-92a and the positive rates of fecal occult blood test were compared among groups,the results showed that the colorectal cancer group>colorectal adenoma group>control group(Plt;0.05).Patients with high expression of miRNA-92a in feces had a 3.547 times lower risk of developing colorectal cancer compared to those with low expression.Advanced adenoma,a history of multiple polyps,positive fecal miRNA-92a,and positive fecal occult blood test were independent risk factors for colorectal cancer(Plt;0.05).In the colorectal cancer group,the expression of fecal miRNA-92a was compared among patients with different tumor diameters,T-stage,N-stage,M-stage,degree of differentiation,and whether they had lymph node metastasis,and the differences were statistically significant(Plt;0.05).The expression of fecal miRNA-92a was positively correlated with tumor diameter,T-stage,N-stage,M-stage,degree of differentiation,and lymph node metastasis(Plt;0.05).The area under the curve of fecal miRNA-92a,fecal occult blood test,and their combination for diagnosing colorectal cancer were 0.685,0.795,respectively;the combination test had high sensitivity but low specificity,while the serial test had low sensitivity but high specificity.ConclusionHigh expression of miRNA-92a in feces can increase the risk of developing colorectal cancer.Fecal miRNA-92a,fecal occult blood test in series or parallel can respectively improve the specificity and sensitivity of clinical diagnosis.
[Key words]Feces;MiRNA-92a;Colorectal cancer;Fecal occult blood test
目前对于结直肠癌的临床筛查仍有不足之处,粪便隐血试验对于结直肠腺瘤等癌前病变的灵敏度较低,肠镜存在高花费、高侵入性的问题,且顺应性较低,不适用于大样本量筛查[1-2]。不同于蛋白和mRNA,miRNA-92a作为miRNAs具有稳定性高、降解速度慢等特点,作用于细胞信号与细胞周期调控中,临床应用中miRNA-92a可于血清、组织、机体排泄物中检出[3-7]。本研究分析miRNA-92a与粪便隐血试验联合诊断在结直肠癌早期筛查中的应用价值。
1对象与方法
1.1研究对象
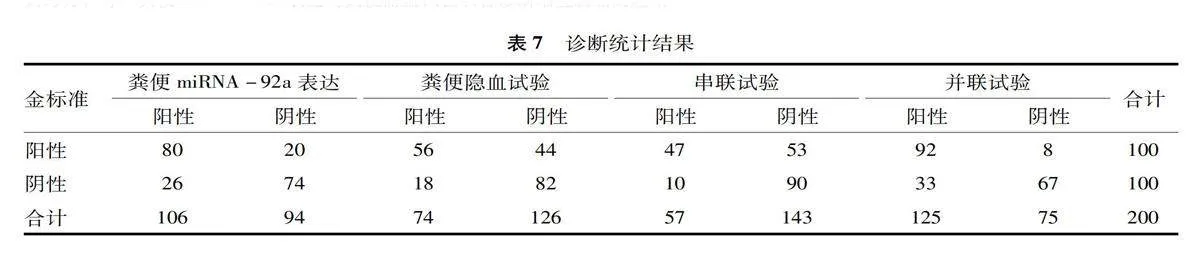
选取2020年1月~2022年12月本院收治的100例结直肠癌患者(结直肠癌组)和100例结直肠腺瘤患者(结直肠腺瘤组),另选取同期200例年龄、性别匹配的健康体检者为对照组。纳入标准:①结直肠癌和结直肠腺瘤均经结肠镜及病理检查结果证实;②未接受相关放化疗或靶向治疗;③无肠易激综合征、炎症性肠病等肠道慢性病史;④无自身免疫性疾病;⑤自愿签署知情同意书者。排除标准:①存在其他部位肿瘤;②免疫抑制剂、非甾体抗炎药长期用药史;③合并肛裂、月经、痔等影响检查结果的疾病;④存在重要脏器病变;⑤蒙特利尔认知评估异常。本研究经医院伦理委员会批准。结直肠癌组进展期腺瘤、多发息肉占比大于结直肠腺瘤组、对照组(P<0.05),其他指标三组比较,差异均无统计学意义(P>0.05),见表1。
1.2方法
1.2.1全身基础检查以病历收集、调查问卷、跟踪检查等方式进行资料收集,包括性别、年龄、体质量指数、血压、糖化血红蛋白、血糖、血脂(甘油三酯、总胆固醇、低密度脂蛋白胆固醇、高密度脂蛋白胆固醇)、饮食习惯(吸烟史、饮酒史、红肉摄入过量、新鲜叶菜摄入不足、烧烤腌制食物摄入过量、油脂摄入过量)、结直肠息肉史类型(进展期腺瘤、低危息肉)、息肉数量(单发、多发)。
1.2.2粪便标本采集研究对象自行采样,采样前由研究人员进行粪便标本采样方法的培训,并于卫生间放置宣传册指导,以减少人为因素对检测结果的影响。取不少于1 g(蚕豆大小)新鲜粪便,注意勿采样血便、水便、黏液便。
1.2.3粪便miRNA-92a检测新鲜粪便标本采集30 min内送检,采用粪便RNA提取试剂盒(北京百奥莱博科技有限公司,货号BTN101109),取≥1 g粪便标本,根据试剂盒说明书步骤操作,从样品中提取、纯化RNA,置于-80 ℃冻存待检;按照miRNA cDNA Synthesis试剂盒(上海泽叶生物科技有限公司,货号CW2141S)操作指南进行逆转录,反应条件为37 ℃ 30 min,85 ℃ 5 s,4 ℃暂存;获取逆转录产物,按照SYBR Premix EX TaqTMⅡ试剂盒(北京博奥派克生物科技有限公司,货号TakaRa_DRR820A)操作指南,采用实时荧光定量PCR仪(美国ABI公司,型号7300型)测定miRNA-92a表达水平。
1.2.4粪便隐血试验采用粪便隐血胶体金检测试纸法于样本采集4 h内检测。将粪便标本涂于载玻片,滴加3%过氧化氢溶液(2~3滴)、邻-甲苯胺冰乙酸溶液(10 g/L),2 min内观察试纸十字区内显色情况,显示蓝绿色为阳性,无颜色为阴性。
1.2.5结肠镜检查、病理检查结肠镜检查由消化内科医生完成,结肠镜检查前所有研究对象均须仔细阅读并签署结肠镜检查知情同意书,肠道清洁采用复方聚乙二醇电解质散6袋溶于4 000 mL温开水中于2 h 内喝完,直至便液为无色清亮。病理诊断由病理科2名经验丰富的医师完成,得出统一结论。
1.2.6联合诊断的方法粪便miRNA-92a、粪便隐血试验串联试验阳性判定标准为两种试验均阳性判定为阳性,并联试验阳性判定标准为两种试验中任一阳性即为阳性。
1.3统计学方法
采用SPSS23.0统计学软件进行数据分析。计量资料以±s表示,采用t检验、单因素方差分析(两两比较采用LSD-t检验);计数资料采用χ2检验;多因素logistic回归分析结直肠癌发生的影响因素;Spearman相关系数分析各变量的相关性;ROC曲线分析粪便miRNA-92a、粪便隐血试验串联、并联对结直肠癌患者的诊断价值;P<0.05为差异有统计学意义。
2结果
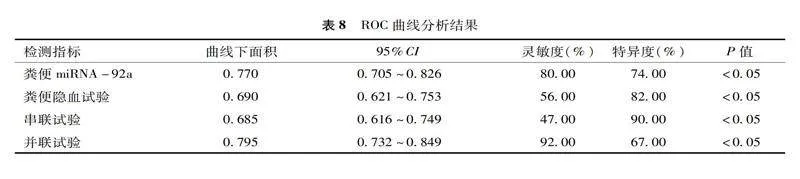
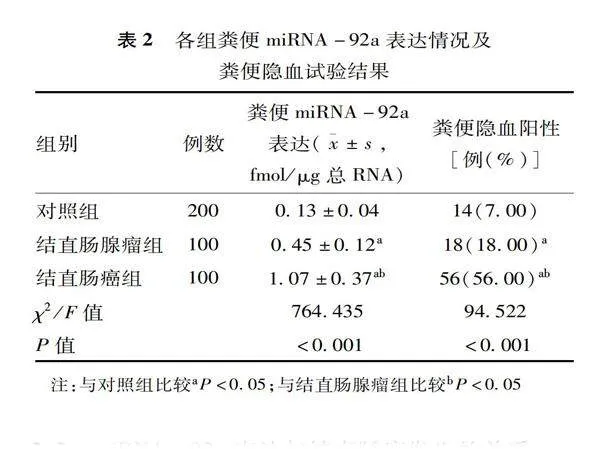
2.1各组粪便miRNA-92a表达情况及粪便隐血试验结果
各组粪便miRNA-92a表达水平及粪便隐血阳性率比较,结直肠癌组>结直肠腺瘤组>对照组,差异均有统计学意义(P<0.05),见表2。
2.2miRNA-92a表达与结直肠癌发生的关系
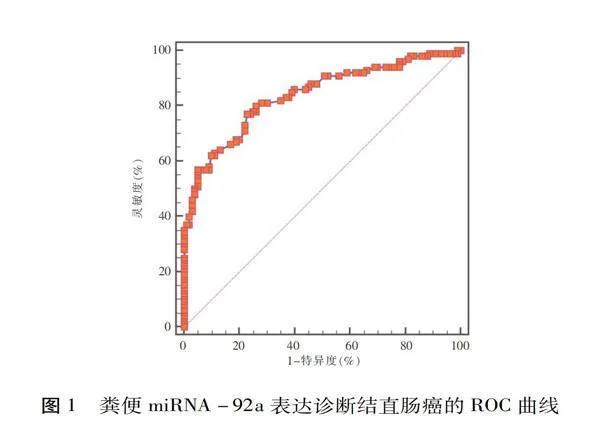
以300例作为样本,绘制ROC曲线分析粪便miRNA-92a表达对结直肠癌的诊断价值,获取截断值为0.78 fmol/μg总RNA,见图1,以该截断值为界,进行危险度分析,结直肠腺瘤患者粪便miRNA-92a高表达发生结直肠癌的风险是低表达患者的3.547倍(P<0.05),见表3。
2.3结直肠癌发病的影响因素分析
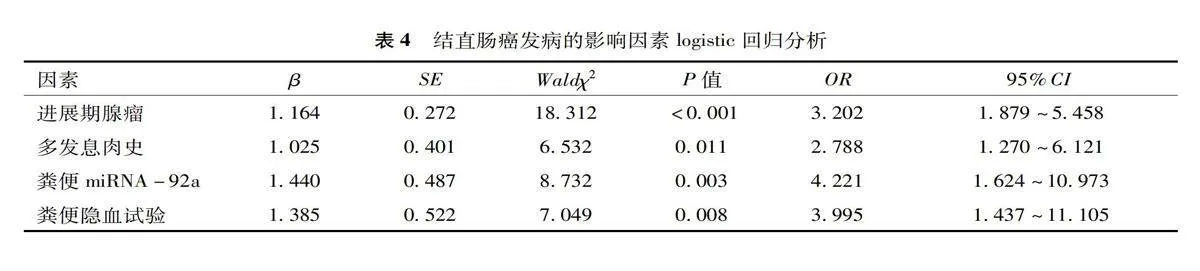
以结直肠息肉史类型(低危息肉=1,进展期腺瘤=2)、息肉史数量(单发息肉史=1,多发息肉史=2)、粪便miRNA-92a表达(≤0.78 fmol/μg总RNA=1,>0.78 fmol/μg总RNA=2)、粪便隐血试验(阴性=1,阳性=2)为自变量,以是否发生结直肠癌为因变量(否=0,是=1)进行多因素logistic回归分析,结果显示:进展期腺瘤、多发息肉史、粪便miRNA-92a>0.78 fmol/μg总RNA、粪便隐血试验阳性是结直肠癌发病的独立危因素(P<0.05),见表4。
2.4结直肠癌组临床病理特点与粪便miRNA-92a表达
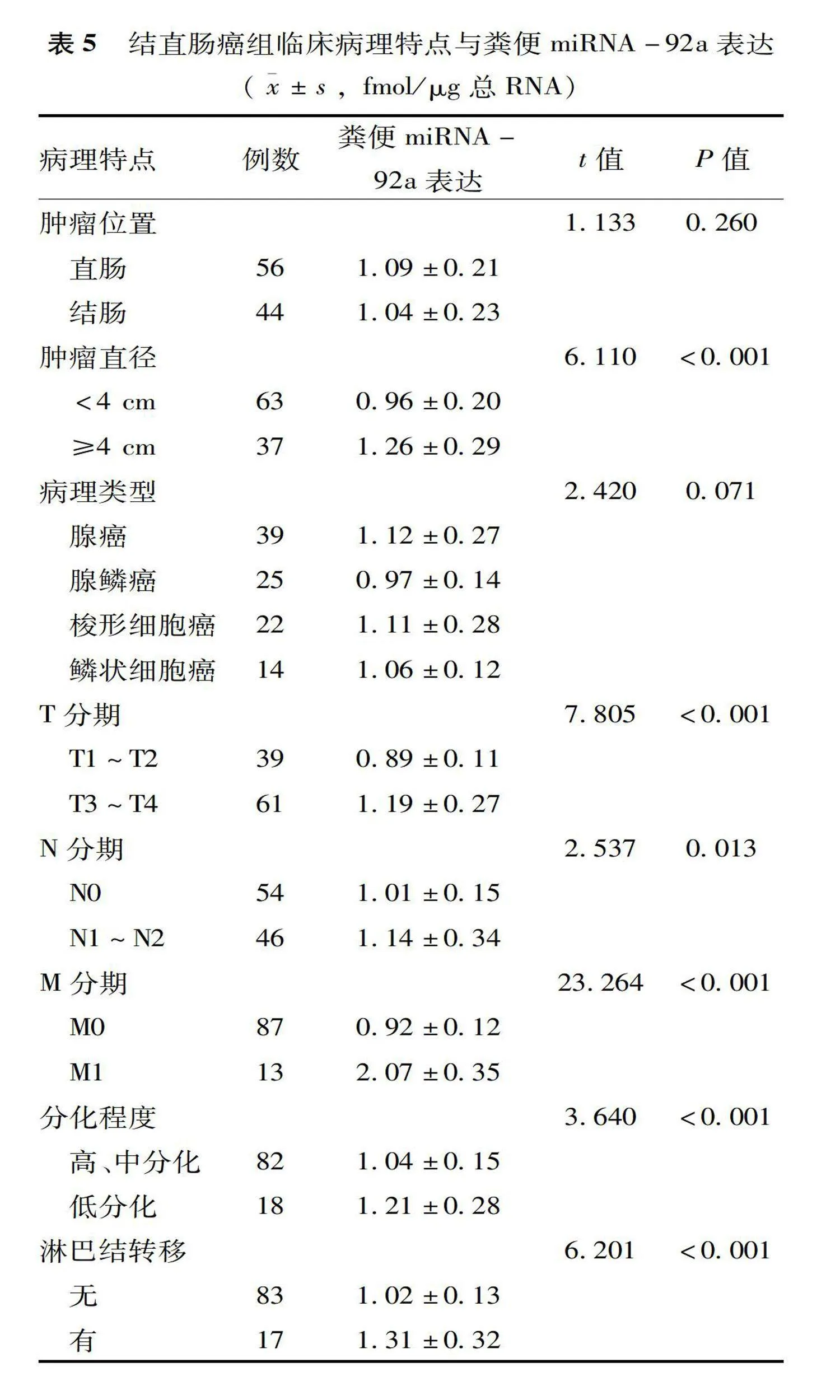
结直肠癌组不同肿瘤直径、T分期、N分期、M分期、分化程度及有无淋巴结转移患者的粪便miRNA-92a表达比较,差异有统计学意义(P<0.05),见表5。
2.5粪便miRNA-92a表达与结直肠癌病理特点的相关性
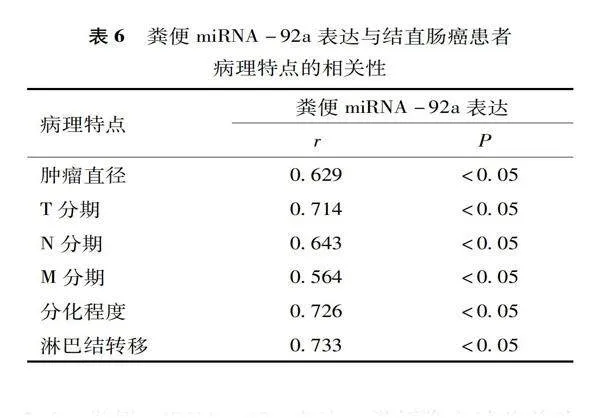
赋值方式:肿瘤直径<4 cm=1,≥4 cm=2;T分期T1~T2=1,T3~T4=2;N分期N0=1,N1~N2=2;M分期M0=1,M1=2;分化程度高、中分化=1,低分化=2;无淋巴结转移=1,有=2。粪便miRNA-92a表达与结直肠癌肿瘤直径、T分期、N分期、M分期、分化程度及淋巴结转移均呈正相关(P<0.05),见表6。
2.6粪便miRNA-92a表达、粪便隐血试验单独诊断结直肠癌及串联、并联联合诊断的结果
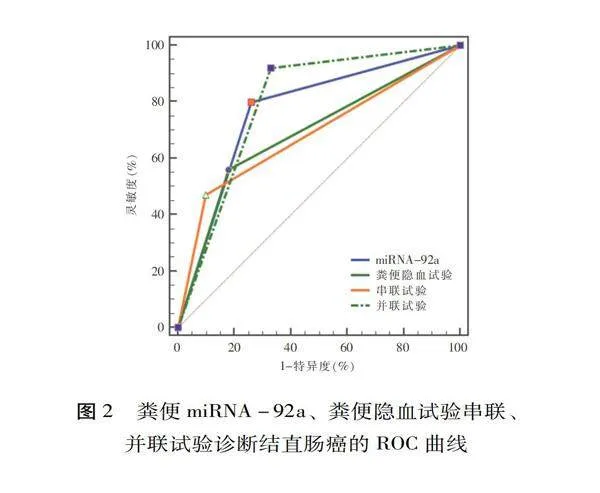
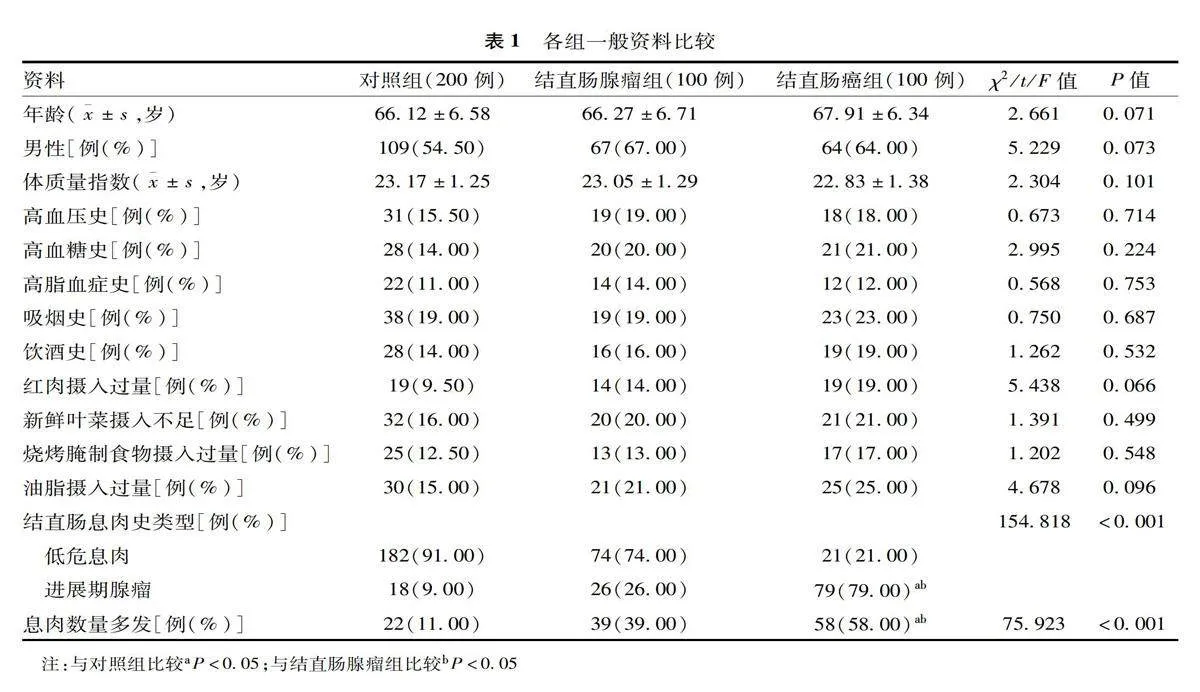
以直肠癌患者和结直肠腺瘤患者作为样本进行分析,串联、并联试验诊断结直肠癌的AUC值及灵敏度最高,粪便miRNA-92a、粪便隐血试验串联试验的灵敏度较低,见表7~8、图2。
3讨论
本研究显示,结直肠癌组粪便miRNA-92a表达水平最高,结直肠腺瘤组次之。miRNA-92a不仅表达于结直肠病变组织细胞,结直肠黏膜细胞生理性脱落至肠腔,亦少量表达于正常黏膜表面细胞,故对照组粪便中也有少量miRNA-92a表达[8-9]。结直肠癌的发生演变过程较为复杂,主要为正常肠上皮发生病变,然后由非进展期腺瘤持续演变为进展期腺瘤、腺癌、癌转移等一系列病理改变,伴随结直肠癌缺失基因、DNA异常甲基化等大量癌基因、抑癌基因突变;相对于结直肠正常黏膜脱落的上皮细胞,肿瘤细胞更具生存活性[10-12]。
经logistic回归分析发现,粪便miRNA-92a与结直肠癌发生有关。miRNA异位表达或突变已在多种肿瘤疾病中证实,miRNA-92a属miRNA-17-92基因簇,定位于人体第13号及X染色体,在生物体发育过程中发挥重要调控作用,是结直肠癌病情进展的核心,发挥癌基因或腺瘤抑制基因功能[13-15]。冷晓旭等研究表明,粪便标志物miRNA检测对于癌前病变的检出率较高,操作简便、检查费用较低,但诊断靶向性存在不足[16]。以往有研究结直肠病变患者血清、癌组织中miRNA-92a表达情况。Zaki等研究表明,结直肠腺瘤患者血清miRNA-92a表达水平高于健康者[17]。张志勇等研究表明,中晚期结直肠癌组织中miRNA-92a表达明显升高,并且与微血管密度形成、肿瘤恶化有关[18]。本研究粪便miRNA-92a表达与高龄结直肠癌肿瘤直径、T分期、N分期、M分期、分化程度及淋巴结转移均存在正相关性,进一步明确粪便miRNA-92a表达对结直肠癌诊断有明确意义。
研究表明miRNA参与结直肠癌干细胞相关信号通路,并能通过直肠癌肿瘤上皮间质转化途径调控结直肠癌肿瘤干细胞的作用机制[19-20]。通常在早期癌、癌前病变诊断中,癌组织细胞进入机体血液循环较少,基于血液的检测可能不易查出,而对于结直肠病变,黏膜表面细胞持续性脱落,粪便中富集肠道脱落上皮细胞,有利于病变检出;且基于粪便的检测可重复性较强,因此在早期筛查中十分重要[21-22]。粪便隐血试验是常用结直肠癌筛查方法,但其检测的应用价值有限,灵敏度较低,约50%,通常需间隔1周后再次检测[23]。本研究中ROC曲线分析粪便miRNA-92a、粪便隐血试验串联诊断结直肠癌的AUC值为0.685,特异度增高,更适用于较低风险群体的大范围筛查,如既往有结直肠息肉史的健康体检者,简便试验后若提示有患病可能,再进一步检测筛查。粪便miRNA-92a、粪便隐血试验并联用于结直肠癌诊断的AUC值为0.795,灵敏度增高,但特异度降低,当需要对结直肠癌高风险者作出迅速诊断时,并联试验可有效提高诊断灵敏度,减少漏诊,避免延误病情。
综上所述,粪便miRNA-92a表达与结直肠癌患者病理特点有关,其高水平表达可增加结直肠癌发生风险,与粪便隐血试验串联、并联试验可分别提高临床诊断的特异度、灵敏度,对临床针对性诊断具有指导意义。
参考文献
[1]He X,Hang D,Wu K,et al.Long-term Risk of Colorectal Cancer After Removal of Conventional Adenomas and Serrated Polyps[J].Gastroenterology,2020,158(4):852-861.e4.
[2]Wielandt AM,Hurtado C,Moreno M,et al.Fecal occult blood test for colorectal cancer screening[J].Rev Med Chil,2021,149(4):580-590.
[3]Shi Y,Liu Z.Serum miR-92a-1 is a novel diagnostic biomarker for colorectal cancer[J].J Cell Mol Med,2020,24(15):8363-8367.
[4]Mao QQ,Chen JJ,Xu WJ,et al.miR-92a-3p promotes the proliferation and invasion of gastric cancer cells by targeting KLF2[J].J Biol Regul Homeost Agents,2020,34(4):1333-1341.
[5]魏前灯,郑文波,孙凯.MiR-92a表达上调与结直肠癌临床病理及预后的相关性分析[J].转化医学杂志,2020,9(1):8-11.
[6]Chen F,Dai X,Zhou CC,et al.Integrated analysis of the faecal metagenome and serum metabolome reveals the role of gut microbiome-associated metabolites in the detection of colorectal cancer and adenoma[J].Gut,2022,71(7):1315-1325.
[7]Cai GX,Cai MY,Feng ZQ,et al.A multilocus blood-based assay targeting circulating tumor dna methylation enables early detection and early relapse prediction of colorectal cancer[J].Gastroenterology,2021,161(6):2053-2056.e2.
[8]熊英,唐晓磊,朱芮.手足口病毒诱导肠上皮细胞差异表达miRNA的筛选及其在患儿粪便标本中的诊断效能分析[J].山东医药,2020,60(35):1-5.
[9]de Miguel Pérez D,Rodriguez Martínez A,Ortigosa Palomo A,et al.Extracellular vesicle-miRNAs as liquid biopsy biomarkers for disease identification and prognosis in metastatic colorectal cancer patients[J].Sci Rep,2020,10(1):3974.
[10]李程,闫柯,霍斌亮,等.结直肠癌不同病理特征患者化疗前后循环肿瘤DNA水平变化及预后预测的列线图模型构建[J].疑难病杂志,2022,21(6):566-570,581.
[11]Luo H,Zhao Q,Wei W,et al.Circulating tumor DNA methylation profiles enable early diagnosis,prognosis prediction,and screening for colorectal cancer[J].Sci Transl Med,2020,12(524):eaax7533.
[12]Wieszczy P,Kaminski MF,Franczyk R,et al.Colorectal cancer incidence and mortality after removal of adenomas during screening colonoscopies[J].Gastroenterology,2020,158(4):875-883.e5.
[13]Yu L,Sui B,Fan W,et al.Exosomes derived from osteogenic tumor activate osteoclast differentiation and concurrently inhibit osteogenesis by transferring COL1A1-targeting miRNA-92a-1-5p[J].J Extracell Vesicles,2021,10(3):e12056.
[14]胡学丽,范先成.乳腺癌组织miR-92a、KLF4 mRNA的表达及与临床病理参数、预后的关系[J].中国现代医学杂志,2022,32(6):74-79.
[15]Liu PJ,Ye YX,Wang YX,et al.MiRNA-92a promotes cell proliferation and invasion through binding to KLF4 in glioma[J].Eur Rev Med Pharmacol Sci,2019,23(15):6612-6620.
[16]冷晓旭,房静远.粪便标志物DNA和RNA筛查结直肠癌特性分析[J].中华医学杂志,2020,100(42):3373-3376.
[17]Zaki A,Fawzy A,Akel SY,et al.Evaluation of microRNA 92a expression and its target protein bim in colorectal cancer[J].Asian Pac J Cancer Prev,2022,23(2):723-730.
[18]张志勇,丁惠娟,王伟民.miR-92a表达与结直肠癌病理学特征及MVD形成的关系[J].实用癌症杂志,2020,35(3):399-402.
[19]陈悦华.MiRNA在结直肠癌干细胞信号通路中的作用[J].临床与病理杂志,2021,41(6):1388-1394.
[20]袁涛,文坤明.microRNAs在调控结直肠癌肿瘤干细胞相关信号通路中的作用机制[J].天津医药,2020,48(11):1115-1119.
[21]Kim M,Vogtmann E,Ahlquist DA,et al.Fecalmetabolomic signatures in colorectal adenoma patients are associated with gut microbiota and early events of colorectal cancer pathogenesis[J].mBio,2020,11(1):e03186-19.
[22]Lee MW,Pourmorady JS,Laine L.Use of fecal occult blood testing as a diagnostic tool for clinical indications:a systematic review and meta-analysis[J].Am J Gastroenterol,2020,115(5):662-670.
[23]Randel KR,Schult AL,Botteri E,et al.Colorectal cancer screening with repeated fecal immunochemical test versus sigmoidoscopy:baseline results from a randomized trial[J].Gastroenterology,2021,160(4):1085-1096.e5.
(2023-02-28收稿)