改良机器人辅助腹腔镜下右肾癌根治术联合下腔静脉I级癌栓切除术一例报道
李恒平 张矛 王向荣 张向向 刘扬 李选鹏
摘 要 下腔靜脉癌栓切除术是泌尿系统最复杂和最具挑战性的手术之一。本文报道1例改良的机器人辅助腹腔镜下右肾癌根治术联合下腔静脉I级癌栓切除术。相比常规下腔静脉癌栓切除术,改良的机器人辅助腹腔镜下腔静脉癌栓切除术不需要完全分离下腔静脉,无需结扎腰静脉、肾上腺静脉,不用阻断下腔静脉、左肾静脉,也不需要切开下腔静脉和重建下腔静脉。本例手术先完全分离右肾,然后向侧面抬起右肾,使下腔静脉内的瘤栓降至肾静脉入下腔静脉处,然后用机械臂将瘤栓完全推进右肾静脉内,在不阻断下腔静脉的情况下完整切除瘤栓。此改良手术成功完成,无任何并发症,未进行输血。患者随访4年后无任何复发迹象。这表明此改良手术简单、安全、可行、值得推广,尤其适用于初学者。
关键词 机器人辅助手术;肾细胞癌;下腔静脉瘤栓;根治性肾切除
中图分类号 R737 文献标识码 A 文章编号 2096-7721(2023)03-0264-07
Modified robot-assisted laparoscopic right radical nephrectomy combined with level I inferior vena cava tumor thrombectomy: a case report
LI Hengping, ZHANG Mao, WANG Xiangrong, ZHANG Xiangxiang, LIU Yang, LI Xuanpeng
(Department of Urology, Gansu Provincial Hospital, Lanzhou 730000, China)
Abstract Inferior vena cave (IVC) tumor thrombectomy is known to be one of the most challenging and intricate surgeries in the urinary system. Herein, we performed a modified robot-assisted laparoscopic right radical nephrectomy combined with level I inferior vena cava thrombectomy in a woman with a 5cm tumor on the right kidney involving level I IVC tumor thrombus. Comparing with the routine surgery, modified robot-assisted laparoscopic right radical nephrectomy with level I IVC tumor thrombectomy only dissects the ventral and right lateral surfaces of IVC, with no need to circumferentially dissociate IVC and left renal vein, ligate the lumbar veins, clamp related vessels, cut the IVC wall, or reconstruct the IVC. This modified procedure was successfully fulfilled with a total surgical time of 3 hours and 45 minutes. There were no perioperative complications or blood transfusion. The modified procedure shows lower risk of hemorrhage and pulmonary embolism, which is safety and worthy of popularization.
Key words Robot-assisted surgery; Renal cell carcinoma; Inferior vena cava tumor thrombus; Radical nephrectomy
Renal cell carcinoma(RCC)is one of the common malignant tumors of the urinary system, affecting 2%~3% of all cancer patients. However, RCC with inferior vena cava (IVC) tumor thrombus is relatively rare, found in just 4%~10% of RCC patients, with a 5-year survival rate of about 47% after surgery[1, 2]. Traditional open surgery has a complication rate of about 38% and an intraoperative mortality rate of 4%~10%[3]. In 2003, laparoscopic radical nephrectomy combined with level I IVC thrombectomy was firstly reported by Desai M M et al. This report suggested that this procedure was safe and feasible[4]. With the development of minimally invasive techniques, laparoscopic radical nephrectomy with IVC thrombectomy has gradually matured[5]. In the past 10 years, robotic surgical system has developed rapidly. In 2011, Abaza R et al. reported the initial robot-assisted laparoscopic radical nephrectomy (RALRN) combined with IVC thrombectomy[6]. Because of its advantages of magnified surgical field, flexible freedom, and accurate suture, RALRN combined with IVC thrombectomy has been quickly applied in clinical practice and yielded good results[7-10]. Although some large medical centers have reported the successful cases of RALRN combined with IVC thrombectomy, these procedures are still very challenging even for experienced doctors[9, 11], and the reason is not only because of the complex procedure, but also for two potentially fatal events: uncontrollable hemorrhage and pulmonary embolism caused by thrombus fragmentation[12]. Herein, we report a case of female patient underwent modified RALRN for right renal carcinoma involving level I IVC thrombectomy, which is simple, safe and lower risk of hemorrhage and pulmonary embolism.
1 Materials and methods
1.1 Case presentation
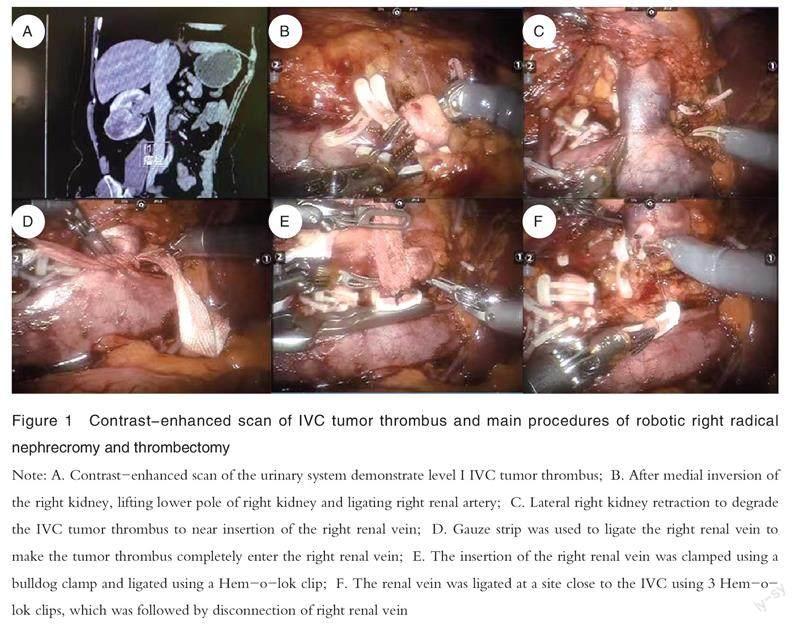
A 46-year-old female patient visited the urology department of Gansu Provincial Hospital in June 2018 due to space-occupying lesions in the right kidney found by ultrasonography in another hospital 1 day before. At our hospital, ultrasonography examination indicated a hypoechoic lesion in the lower right kidney measuring about 50mm×46mm, which was mostly considered to be a renal cancer, and a tumor thrombus in the right renal vein extending to about 1cm above the entry of IVC was also observed. Plain CT scan + contrast-enhanced scan of the urinary system showed lightly low-density mass with an unclear boundary in the lower pole of the right kidney, which was considered to be renal clear cell carcinoma and appeared to be growing outwards, together with filling defects in the right renal vein and part of the IVC (Figure 1A), which was considered to be indicative of the tumor thrombus. The left kidney showed no significant abnormality, and no significant abnormalities of both lungs were revealed by CT imaging. The patients tumor thrombus was classified as level I according to the Mayo classification of tumor thrombus[3]. The outcomes of test for preoperative routine laboratory examining were unremarkable, and further imaging examinations showed no metastases.
1.2 Surgical techniques
Modified RALRN for right renal cancer with level I IVC thrombectomy was performed under general anesthesia. The surgical steps were as follows.
1.2.1 Body position
Following successful general anesthesia, the patient was placed in the left lateral decubitus position at approximately 70 degrees with a high lumbar pad.
1.2.2 Trocar position
A 12mm port was placed about 2cm to the upper right umbilicus as the camera port, while three 8mm robotic ports for first, second, and third robot arm were placed at about 2cm medial to the right midclavicular line and costal margin, at about 8cm to the camera port near the anterior axillary line and McBurneys point, and about 8cm to the caudal cannula beside the rectus abdominis, respectively. In addition, another 12mm port was placed 2cm below the midline of the umbilicus to serve as an assistant port, and a 5mm port was placed near the xiphoid below the costal margin to make another assistant port for intraoperative retraction of the liver.
1.2.3 Surgical steps
1.2.3.1 Routine surgical procedure
After docking, a 30-degree down lens was used for visualization. The hepatocolic ligament were incised, the liver was lifted by clamping the lateral peritoneum with a locked needle holder to fully expose the upper pole of the right kidney. The ascending colon and the transverse colon were reflected medially by incision the peritoneum along the white line of Toldt, and the duodenum and IVC was exposed. The renal artery was clipped with Hem-o-Lok clips in the interaortocaval space. Then the ventral surfaces of the right and left renal veins were isolated. The IVC was dissected above and below the insertion of the renal vein to the extent dictated by the length of the tumor thrombus. The venous collaterals of IVC were ligated and divided for circumferential dissection of IVC. The left renal vein was dissected circumferentially in the interaortocaval space. The IVC above the upper limit of the tumor thrombus was adequately mobilized and the vessel loops were wrapped twice around the IVC above and below the tumor thrombus and the left renal vein. The caudal IVC, left renal vein, and cephalic IVC were sequentially clamped. After clamping the aforementioned vessels, the IVC wall was cut, the thrombus was removed, and the IVC was sutured or reconstructed. After suturing, cephalic IVC, left renal vein, and caudal IVC were released in order[6, 13].Then the radical nephrectomy was performed.
1.2.3.2 Steps of modified surgery
The initial surgical steps remained the same as those in the routine surgery, but it was difficult to find the right renal artery because there were abundant and thick collateral veins around the right renal vein. In view of high risk of hemorrhage, the strategy was changed to radical nephrectomy first with full mobilization of the right kidney and then the IVC thrombus was removed. In order to ligate the right renal artery as early as possible, the lower pole, lateral side, upper pole, and posterior side of the right kidney were adequately separated. After medial inversion of the right kidney, the lower pole of the kidney was lifted to expose the right renal artery, then it was ligated and cut (Figure 1B), and the original position of the right kidney was then restored. The robot arm 3 was used for lateral right kidney retraction to degrade the IVC tumor thrombus to near insertion of the right renal vein (Figure 1C). Subsequently, robot arms 1 and 2 alternately pushed the IVC thrombus into the right renal vein, and gauze strip was used to ligate the right renal vein (to prevent sharp ligation and fragmentation of the tip of the tumor thrombus, otherwise, it would become detached) to make the tumor thrombus completely enter the right renal vein (Figure 1D). Meanwhile, the inserting of the right renal vein was lamped using a bulldog clamp (Figure 1E), and the renal vein was ligated with 3 Hom-o-lok clips at a site close to the IVC, which was followed by disconnection of right renal vein (Figure 1F). Finally, the specimen was placed into an endobag, and devices were withdrawn. The incision was then sutured, which marked the completion of the operation.
2 Results
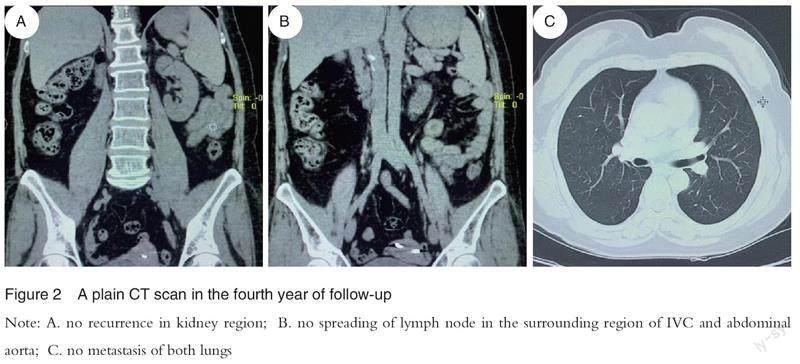
The operation lasted about 3h and 45 min, the volume of blood loss was about 80ml, and no blood transfusion occurred. The patient began to ambulate on the second day after surgery and started liquid diet on the third day. The postoperative pathological outcomes confirmed clear cell renal cell carcinoma with World Health Organization/International Society of Urological Pathology classification of grade 2. No neoplastic necrosis was observed, the renal capsule and perirenal adipose tissues were not involved in the cancer tissue, the renal pelvis and ureter margin of surgery showed no cancer tissue involvement, the perirenal lymph nodes did not metastasize, and an intravascular tumor thrombus was observed in the vena cava. The hospital stay was 6 days, and the patient was regularly followed up for 4 years without any signs of recurrence or metastasis (Figure 2).
3 Discussion
Even in the era of open surgery, radical nephrectomy combined with IVC thrombectomy is known to be one of the most challenging surgeries in the urinary system due to its higher mortality rate and more complications[3]. With the continuous development of minimally invasive techniques, especially the advent of robotic surgical systems, RALRN combined with IVC thrombectomy has now been reported by several institutions and demonstrated to be safe and reliable[6-9]. However, even for experienced surgeons, the surgical risk remains very high, with bleeding attracting the greatest risk during the procedure[10-11]. Surgeons also need to be familiar with anatomy, careful separation, gentle motion, proper prevention and management of avulsion, and superb suture skills[8]. Although studies have suggested strategies to reduce uncontrollable bleeding, this procedure is still very challenging[13]. Compared to the routine surgery[6-9, 11, 13], the modified procedure only dissociates the ventral and right surfaces of IVC with no need to dissociate circumferentially the IVC, which leads no ligation of the lumbar veins and adrenal vein, incision of the IVC, or IVC suturing and reconstruction, it could save operative time and reduce the risks of bleeding or embolization. Studies have reported that operative time, blood transfusion, and grade of tumor thrombus are risk factors for early postoperative complications in patients with tumor thrombus[14-16]. The modified surgical procedure in this study is characterized with a short operative time, low tumor thrombus grade, no need for blood transfusion, and no postoperative complications. Malignant tumor recurrence or metastasis often causes patient death. Even if radical nephrectomy combined with IVC thrombectomy performed in patients with renal cancer involving tumor thrombus, the long-term recurrence rate is as high as 38.6%~74.0% and the 5-year survival rate is 40%~60%[2, 17-19]. This modified surgery does not involve an incision of the IVC, so the tumor thrombus remains completely closed in the blood vessels, which could reduce the chance of tumor cell implantation and lower the risk of recurrence. The patient had no signs of recurrence or metastasis during 4 years of follow-up, which may be related to the adoption of the modified surgical steps. The routine surgery requires occlusion of the left renal vein, caudal IVC, and cephalic IVC above the end of the tumor thrombus before making an incision of the IVC[6-9, 11, 13], which may lead to left renal dysfunction, hemodynamic effects, and lower-extremity venous sequelae[7-8, 20]. Meanwhile, the modified procedure does not require clamping of the IVC and affects on left renal function, systemic blood flow, or lower-extremity veins. Treating renal cancer involving IVC thrombus with robotic surgery has a long learning curve for its complex procedures, high risk, and rare to see[1, 9, 11]. Studies have demonstrated that success in treating renal cancer with level I-IV IVC thrombus surgically required the completion of an initial 40 cases and then 80 more such procedures before the desired clinical outcome could be achieved[21]. It is generally difficult for medical centers to achieve the expected number of surgeries in a short period of time, and this modified surgery has obvious advantages in shortening the learning curve. However, the modified procedure is limited in its own way: in patients with infiltration of the IVC wall or an immobile tumor thrombus or bland thrombus in the lower end of the IVC, routine surgery or circumferential IVC resection is required[7]. In addition, contact with the tumor thrombus should be minimized when removing the kidney so as to lower the risk of tumor thrombus detachment or embolism. In conclusion, the modified robot-assisted laparoscopic right radical nephrectomy combined with level I IVC thrombectomy has obvious advantages, especially for beginners.
4 Conclusions
To our knowledge, we firstly describe the modified robot-assisted laparoscopic right radical nephrectomy with level I IVC thrombectomy. The modified procedure shows lower risk of hemorrhage and pulmonary embolism, which is safety and worthy of clinical popularization.
References
[1] Marshall F F, Dietrick D D, Baumgartner W A, et al. Surgical management of renal cell carcinoma with intracaval neoplastic extension above the hepatic veins[J]. J Urol, 1988, 139(6): 1166-1172.
[2] Parra J, Drouin S J, Hupertan V, et al. Oncological outcomes in patients undergoing radical nephrectomy and vena cava thrombectomy for renal cell carcinoma with venous extension: a single-centre experience[J]. Eur J Surg Oncol, 2011, 37(5): 422-428.
[3] Blute M L, Leibovich B C, Lohse C M, et al. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus[J]. BJU Int, 2004, 94(1): 33-41.
[4] Desai M M, Gill I S, Ramani A P, et al. Laparoscopic radical nephrectomy for cancer with level I renal vein involvement[J]. J Urol, 2003, 169(2): 487-491.
[5] TIAN X J, HONG P, LIU Z, et al. En bloc retroperitoneal laparoscopic radical nephrectomy with inferior vena cava thrombectomy for renal cell carcinoma with level 0 to II venous tumor thrombus: a single-center experience[J]. Cancer, 2020. DOI: 10.1002/cncr.32747.
[6] Abaza R. Initial series of robotic radical nephrectomy with vena caval tumor thrombectomy[J]. Eur Urol, 2011, 59(4): 652-656.
[7] SHI T P, HUANG Q B, LIU K, et al. Robot-assisted cavectomy versus thrombectomy for level II inferior vena cava thrombus: decision-making scheme and multi-institutional analysis[J]. Eur Urol, 2020, 78(4): 592-602.
[8] WANG B J, LI H Z, HUANG Q B, et al. Robot-assisted retrohepatic inferior vena cava thrombectomy: first or second porta hepatis as an important boundary landmark[J]. Eur Urol, 2018, 74(4): 512-520.
[9] Chopra S, Simone G, Metcalfe C, et al. Robot-assisted level II-III inferior vena cava tumor thrombectomy: step-by-step technique and 1-year outcomes[J]. Eur Urol, 2017, 72(2): 267-274.
[10] Aghazadeh M A, Goh A C. Robotic left-sided level II caval thrombectomy and nephrectomy using a novel supine, single-dock approach: primary description[J]. Urology, 2018. DOI: 10.1016/j.urology.2017.10.018.
[11] Gill I S, Metcalfe C, Abreu A, et al. Robotic level III inferior vena cava tumor thrombectomy: initial series[J]. J Urol, 2015, 194(4): 929-938.
[12] GU L Y, MA X, GAO Y, et al. Robotic versus open level I-II inferior vena cava thrombectomy: a matched group comparative analysis[J]. J Urol, 2017, 198(6): 1241-1246.
[13] WANG B J, LI H Z, MA X, et al. Robot-assisted laparoscopic inferior vena cava thrombectomy: different sides require different techniques[J]. Eur Urol, 2016, 69(6): 1112-1119.
[14] Ebbing J, Wiebach T, Kempkensteffen C, et al. Evaluation of perioperative complications in open and laparoscopic surgery for renal cell cancer with tumor thrombus involvement using the Clavien-Dindo classification[J]. Eur J Surg Oncol, 2015, 41(7): 941-952.
[15] Abel E J, Thompson R H, Margulis V, et al. Perioperative outcomes following surgical resection of renal cell carcinoma with inferior vena cava thrombus extending above the hepatic veins: a contemporary multicenter experience[J]. Eur Urol, 2014, 66(3): 584-592.
[16] Haddad A Q, Leibovich B C, Abel E J, et al. Preoperative multivariable prognostic models for prediction of survival and major complications following surgical resection of renal cell carcinoma with suprahepatic caval tumor thrombus[J]. Urol Oncol, 2015, 33(9): 388 e381-389.
[17] Berczi A, Flasko T, Szerafin T, et al. Surgical management and outcome of renal cell carcinoma with inferior vena cava tumor thrombus[J]. Urol Int, 2017, 99(3): 267-271.
[18] TANG Q, SONG Y, LI X S, et al. Prognostic outcomes and risk factors for patients with renal cell carcinoma and venous tumor thrombus after radical nephrectomy and thrombectomy: the prognostic significance of venous tumor thrombus level[J]. Biomed Res Int, 2015. DOI: 10.1155/2015/163423.
[19] Ali A S, Vasdev N, Shanmuganathan S, et al. The surgical management and prognosis of renal cell cancer with IVC tumor thrombus: 15-years of experience using a multi-specialty approach at a single UK referral center[J]. Urol Oncol, 2013, 31(7): 1298-1304.
[20] Donaldson M C, Wirthlin L S, Donaldson G A. Thirty-year experience with surgical interruption of the inferior vena cava for prevention of pulmonary embolism[J]. Ann Surg, 1980, 191(3): 367-372.
[21] SHEN D L, WANG H F, WANG C F, et al. Cumulative sum analysis of the operator learning curve for robot-assisted mayo clinic level I-IV inferior vena cava thrombectomy associated with renal carcinoma: a study of 120 cases at a single center[J]. Med Sci Monit, 2020. DOI: 10.12659/MSM.922987.