Efficacy and safety of subthreshold micropulse laser in the treatment of acute central serous chorioretinopathy
Jian-Jie Guo, Xiu-Juan Li, Jing-Jing Wan
Department of Ophthalmology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province,China
Abstract● AlM: To analyze the efficacy and safety of subthreshold micropulse laser (SML) in the treatment of acute central serous chorioretinopathy (CSC).
● KEYWORDS: central serous chorioretinopathy;subthreshold micropulse laser; optical coherence tomography angiography; microperimetry
INTRODUCTION
C entral serous chorioretinopathy (CSC) is a common fundus disease characterized by serous detachment of the neural retina in the posterior pole, often accompanied with dysfunction of the choroid and retinal pigment epithelium(RPE)[1].Patients with CSC usually manifested as visual acuity decreased, metamorphopsia, micropsia and dark vision, it’s more common in young and middle-aged men[2].The disease is usually divided into acute CSC (aCSC) and chronic CSC,but the exact time scale between the acute and chronic forms has not a consensus.Many cases of aCSC are self-limiting with spontaneous resolution of subretinal fluid (SRF) within 3-4mo, but up to 30%-50% of cases will persist and recur, then it may can cause irreversible damage to visual function[3].It is worth noting that the short-term presence of SRF also can cause irreversible damage to photoreceptors[4].Furthermore,persistent SRF may cause some complications, such as RPE atrophy, choroidal neovascularizations (CNV), and polypoidal choroidal vasculopathy[5].Therefore, early and effective intervention is very necessary for aCSC.
Thus far, due to the complexity of its pathogenesis and clinical classification, there is no agreement on the treatment strategy for the disease.Traditionally, conventional laser was the only option for treating CSC.Conventional laser can close focal sites of RPE leakage, but it just can be applied to the point of angiographic leakage which is located more than 400 µm from the fovea, moreover, vision loss, visual field defect,decreased contrast sensitivity, and CNV may occur at the treatment area, affecting the patient’s visual quality[6-7].About 10 years ago, photodynamic therapy (PDT) was introduced for the treatment of CSC, and many studies have proven its effectiveness.However, PDT may cause choriocapillary closure, RPE alterations, and stimulate the upregulation of vascular endothelial growth factor (VEGF) and CNV[8].More importantly, PDT treatment is expensive and unavailable in some areas.Intravitreal injections of anti-VEGF drugs have been used in the treatment of CSC, however, its effectiveness is still controversial at home and abroad, and it is an invasive treatment, which has the risk of serious complications such as intraocular hemorrhage and infection.Therefore, anti-VEGF drugs are not suitable as the first-line treatment of aCSC[9-10].Many kinds of oral drugs are used in the aCSC, but the effect is not clear, and systemic side effects are unavoidable, further research is still required[11].Subthreshold micropulse laser (SML) is a promising treatment modality because of its low treatment cost, repeatability, and no damage to adjacent tissues[7].The purpose of this study was to assess the efficacy and safety of SML in the treatment of aCSC.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted following the principles of the Declaration of Helsinki.Informed consent was obtained from all subjects.This study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University, the approval number is 2023-KY-0265-001.
Study Design and ParticipantsThis was a retrospective case analysis study, which included patients with aCSC who visited the First Affiliated Hospital of Zhengzhou University from August 2020 to May 2022.All patients were diagnosed by fundus fuloresceien angiography (FFA), indocyanine green angiography (ICGA), and optical coherence tomography(OCT).The 58 eyes of 58 patients were included in the study,they were assigned into SML group (n=39) and observation group (n=19), SML group received SML therapy, and a month later, if the subretinal fluid was not completely absorbed,the treatment could be repeated, the observation group only reviewed regularly.If both eyes of the patient are affected,choose the left eye to be included in the study.The follow-up period was 3mo after diagnosis in our hospital.
Patients who were diagnosed as CSC by FFA, ICGA and OCT and whose course of disease was less than 3mo could be included in the study.Exclusion criteria were: 1) Patients had received PDT, conventional laser photocoagulation and intravitreal injection of anti-VEGF agents.2) Suffering from hypertension, diabetes, liver and kidney dysfunction, and other systemic diseases.3) Being treated with systemic steroids.4)History of eye trauma or eye surgery.5) Combined with high myopia or other fundus diseases, including CNV.6) Allergy history of indocyanine green or fluorescein sodium.
Data CollectionAll selected patients underwent ophthalmic examination at diagnosis and 3mo after diagnosis, including best corrected visual acuity (BCVA), intraocular pressure,fundus examination after mydriasis, OCT, optical coherence tomography angiography (OCTA), microperimetry, and review as needed during follow-up.All patients in SML group underwent fundus autofluorescence (FAF) before and 3mo after treatment to observe the effects of SML on RPE.FFA and ICGA be performed before treatment and then repeated as required.Check the BCVA with the international standard visual acuity chart, and convert it to a logarithm of the minimum angle of resolution (logMAR) scale for analysis.Central retinal thickness (CRT) and subfoveal choroidal thickness (SFCT) are automatically measured by OCT (SVision VG200) built-in software.CRT is defined as the height from the internal limiting membrane to Bruce’s membrane (Figure 1).
TreatmentsSML treatments are carried out by the same experienced ophthalmologist.All patients were fully dilated with tropicamide phenylephrine eye drops, then the topical anesthesia was performed with obucaine eye drops.The IQ 577 laser therapeutic instrument of Iridex Company in the United States is used and set to the micropulse mode, the laser parameter was set to 5% duty cycle, the spot diameter was 200 μm, the exposure time was 200ms, the treatment energy is 400 mW, and the 7×7 matrix mode without spacing between two spots is adopted, the photocoagulation range covers the entire edema area.After SML therapy, pranoprofen eye drops were given for analgesia and anti-inflammatory.Recheck one month after treatment, if there is still SRF, the treatment can be repeated.
Statistical AnalysisStatistical analysis was performed using SPSS 26.0.All quantitative data were tested for normality using Shapiro-Wilk test.The variables in accordance with the normal distribution were expressed as mean±standard deviation(SD), and the differences between groups were analyzed byt-test.Variables that did not meet the normal distribution were expressed as median [interquartile range (IQR)], and the Rank-Sum test was used to analyze the difference between groups.The intra group differences were analyzed by pairedt-test or paired Rank-sum test.For categorical variables, the data difference between the two groups was analyzed by the Chi-square test.Pvalues less than 0.05 were considered statistically significant.
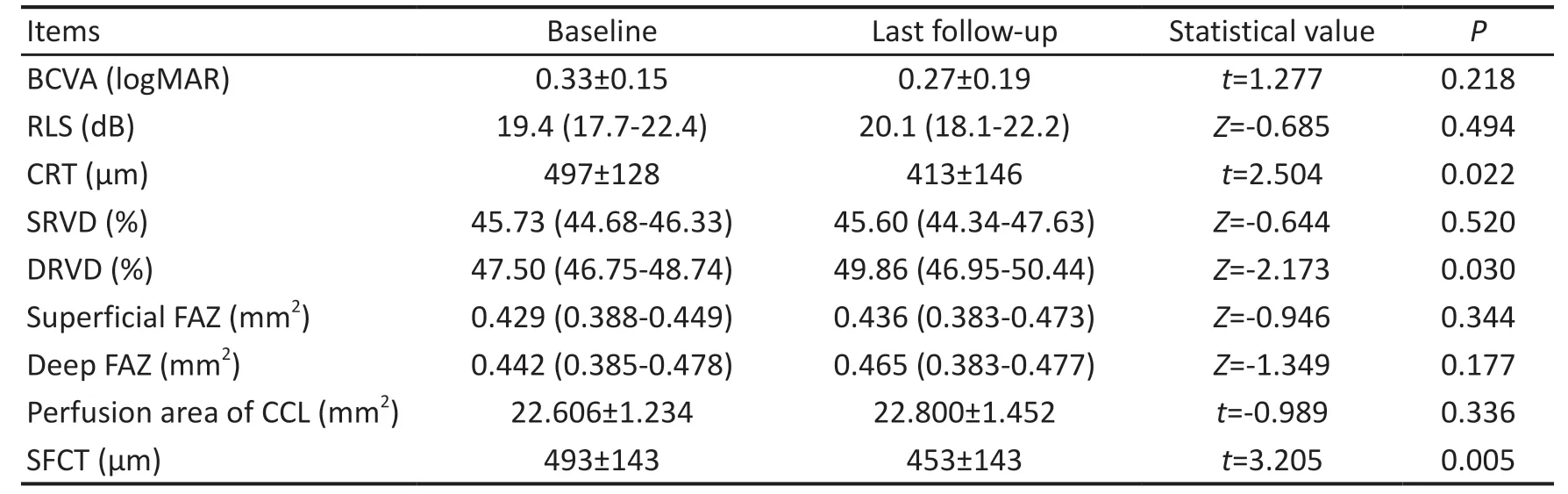
Table 2 Changes of research items in the observation group during follow-up mean±SD/IQR
RESULTS
Patient Demographics and Baseline CharacteristicsFifty-eight patients were included in this study, the mean age of the patients was 46±8 (range: 32-64)y, the average course of disease was 42±16 (range: 16-78)d, and there were 45 males and 13 females.They were divided into SML group(n=39) and observation group (n=19), there was no significant difference in age, gender, course of disease and baseline characteristics of the research items between the two groups (allP>0.05; Table 1).
Changes in Research Items of the Observation GroupCompared with the baseline data, the last follow-up of patients in the observation group showed that CRT decreased,deep retinal vascular density (DRVD) increased, and SFCT decreased, the differences were statistically significant (allP<0.05; Table 2).But, there was no significant difference in BCVA, retinal light sensitivity (RLS), superficial retinal vascular density (SRVD), superficial and deep foveal avascular zone (FAZ) area, and perfusion area of choroidal capillary layer(CCL) (allP>0.05; Table 2).
Changes in Research Items of the Subthreshold Micropulse Laser GroupIn the SML group, compared with before treatment, BCVA, RLS, SRVD, DRVD and perfusion area of CCL were increased, CRT and SFCT were significantly reduced, the area of superficial and deep FAZ were reduced 3mo after treatment, the differences were statistically significant (allP<0.05; Table 3, Figure 2).
Comparison of Research Items Between Two Groups at the Last Follow-upAt 3mo, BCVA and RLS in SML group were better than those in the observation group, and CRT was lower, SRVD, DRVD and perfusion area of CCL were larger,differences were statistically significant (allP<0.05; Table 4).However, there was no significant difference in the superficial and deep FAZ area and SFCT compared with the observation group (allP>0.05; Table 4).
SafetyOn FAF, all SML-treated patients showed different degrees and types of fluorescence reduction or enhancement before treatment, and no change of treatment spots was found after treatment (Figure 3).No structural laser damage was observed on OCT and OCTA, and no CNV was found.
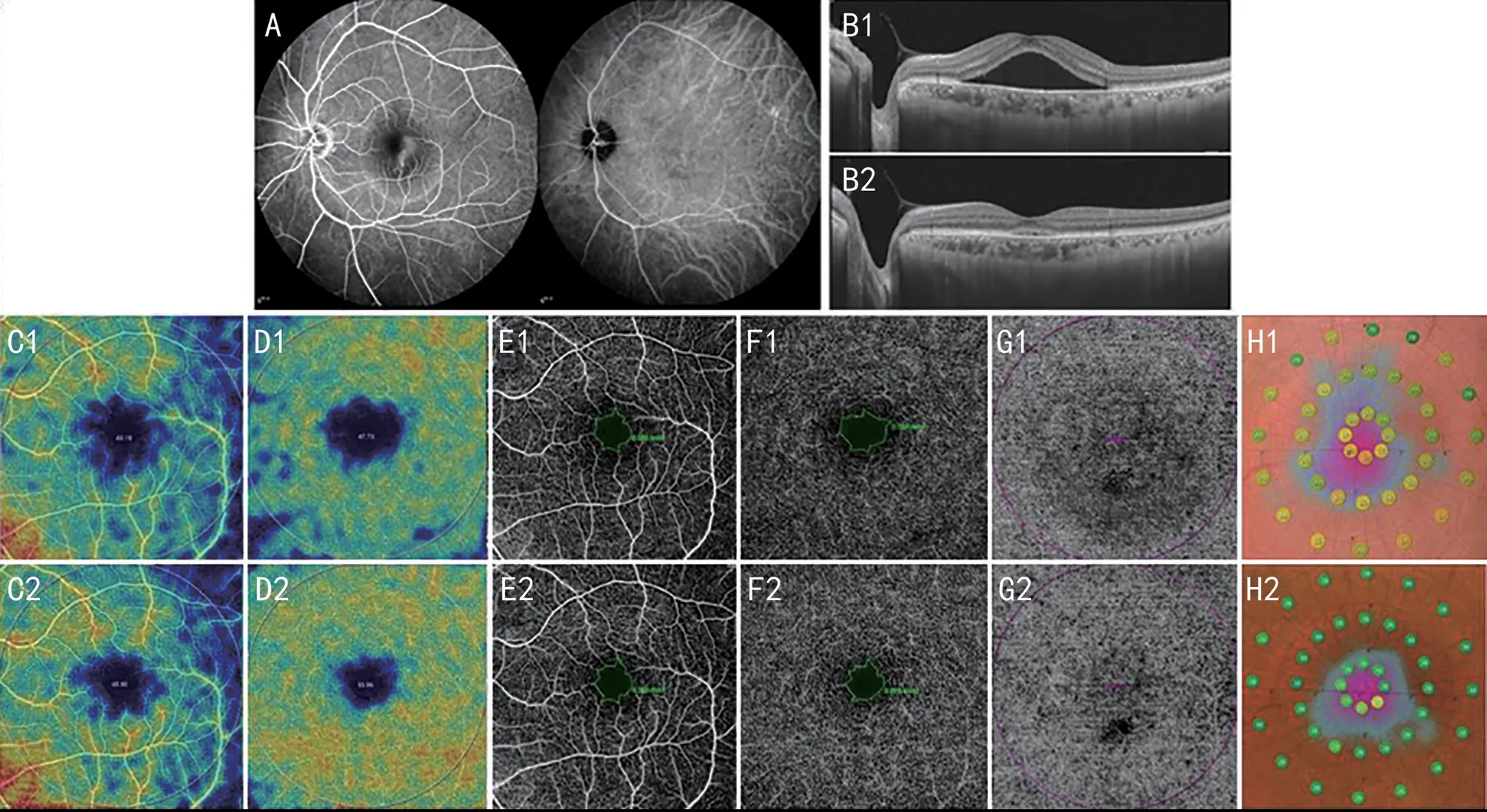
Figure 2 A 46 years old male patient’s fundus examination before and after SML treatment A: FFA and ICGA at the time of diagnosis; B: OCT before treatment (B1) and 3mo after treatment (B2); C: SRVD before treatment (C1) and 3mo after treatment (C2); D: DRVD before treatment(D1) and 3mo after treatment (D2); E: Superficial FAZ area before treatment (E1) and 3mo after treatment (E2); F: Deep FAZ area before treatment (F1) and 3mo after treatment (F2); G: Perfusion area of CCL before treatment (G1) and 3mo after treatment (G2); H: RLS before treatment (H1) and 3mo after treatment (H2).SML: Subthreshold micropulse laser; FFA: Fluoresceien angiography; ICGA: Indocyanine green angiography; OCT: Optical coherence tomography; SRVD: Superficial retinal vascular density; DRVD: Deep retinal vascular density; FAZ: Foveal avascular zone; CCL: Choroidal capillary layer; SFCT: Subfoveal choroidal thickness; RLS: Retinal light sensitivity.
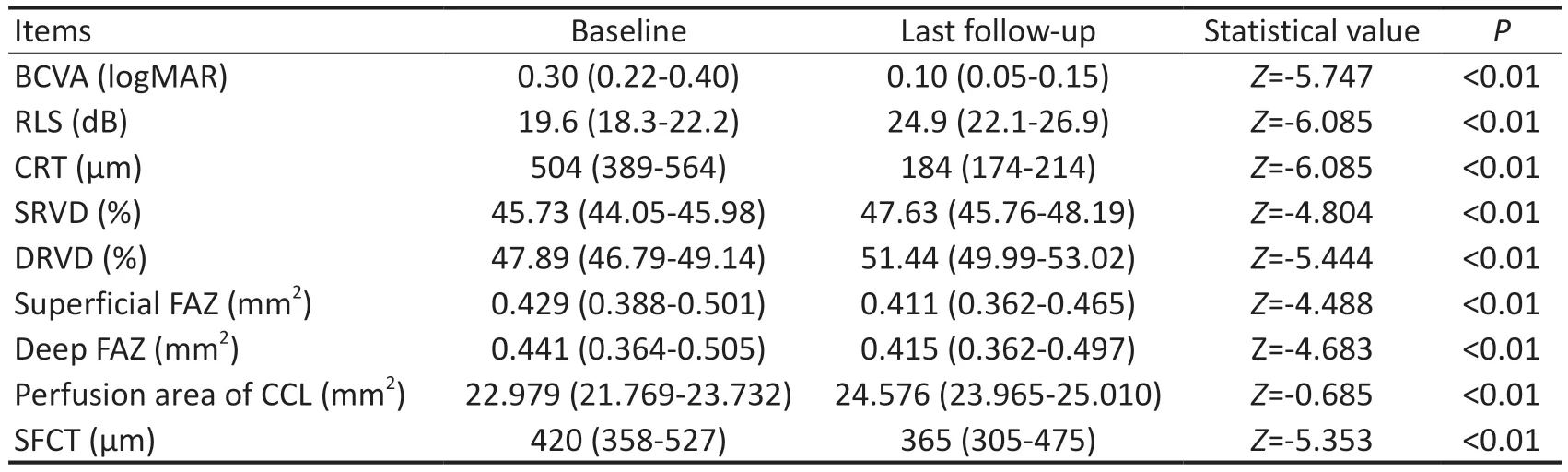
Table 3 Changes of research items in the SML group during follow-up IQR
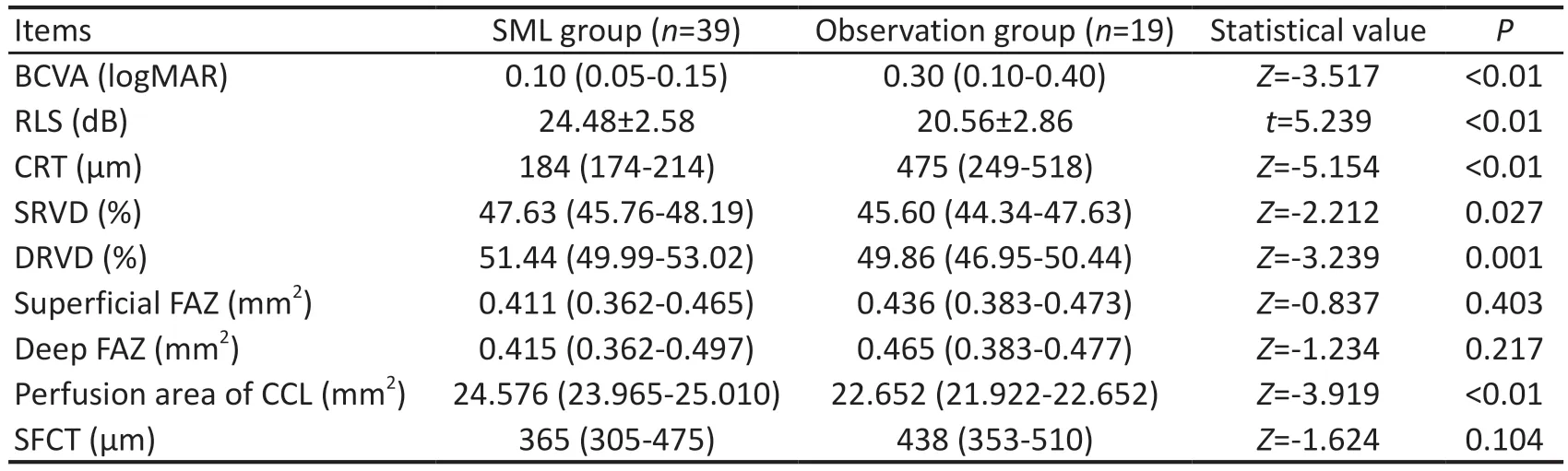
Table 4 Comparison of research items between two groups of patients at 3mo after diagnosis mean±SD/IQR
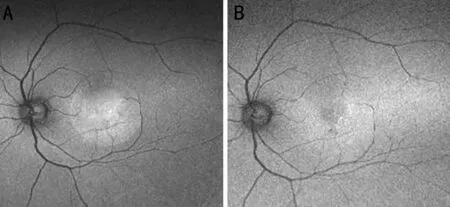
Figure 3 A 46 years old male patient’s FAF A: FAF before treatment; B:FAF 3mo after treatment.FAF: Fundus autofluorescence.
DISCUSSION
CSC is an idiopathic chorioretinopathy with predominantly macular involvement, characterized by localized serous detachment of the neuroepithelial layer and RPE layer[7].The exact pathophysiological mechanism of CSC remains unknown.The most widely accepted explanation currently includes two factors: high permeability of choroidal vessels and RPE dysfunction[3].The hypothesis of choroidal dysfunction holds that the hyperpermeability of choroidal vessels and the focal hypoperfusion of choroidal capillaries lead to ischemia and hypoxia of adjacent retinal tissues, thereby impairing the structure and function of RPE layer, and exudates enter the subretinal neuroepithelial layer[12-13].However, the theory of RPE dysfunction believes that VEGF secreted by RPE can maintain the normal structure and homeostasis of choroidal capillaries, long-term diseases and chronic RPE atrophy lead to the increase of choroidal capillary hydrostatic pressure and the decrease of RPE barrier function, resulting in the accumulation of SRF[14].For many years, aCSC has been considered a selflimiting disease, most of which can recover without any damage within 3-4mo after onset[1], so many scholars advocate observing the changes of the disease.However, research by Gawęckiet al[15]shows that the presence of SRF in the course of CSC, even in its acute and fast-resolving form, can lead to functional and morphological alterations of the retina.Uzluet al[16]found the longer the course of the disease, the more severe the damage to the retinal structure and function,when the symptoms persist for more than 4mo, even if the anatomical structure is restored, the patient’s visual function will be irreversibly damaged.Therefore, early, effective and safe treatment of aCSC is very necessary.
SML is a kind of short and high-frequency repetitive pulse laser with the characteristics of short exposure time, low energy and high density[17].Ⅰt is different from the traditional continuous laser and can minimize the related thermal damage.The key part of SML treatment is RPE, it activates the function of RPE, heats the RPE complex through a dense spot of light, induces HSP70 expression, inhibits apoptosis and down-regulates inflammatory factors.At the same time, light stimulates sublethal RPE cells to produce pigment epitheliaderived factors and VEGF inhibitors, restores pump function and outer barrier, and finally reduces choroidal permeability to achieve therapeutic effect[18-19].SML can use either the 577 nm or the 810 nm wavelength, the 577 nm micropulse laser can minimize the absorption of yellow light by lutein in the inner and outer plexiform layer of the macula, so it is relatively safe for the treatment of macular fovea and its vicinity[20].Gawęckiet al[21]confirmed that SML can effectively promote the absorption of SRF without changing the structural morphology of retina.In this study, no change of treatment spots was found after SML treatment, and no laser scar or structural damage was found on OCT and OCTA.This indicates that SML therapy for aCSC is safe in the short term and can be applied to the macular region and its adjacent tissues, which has more advantages than traditional laser and PDT, this is consistent with the previous safety research results of micropulse laser[18,22].
OCTA is a new ocular examination technology developed in recent years, and it has attracted the attention of ophthalmologists as soon as it was born because of its advantages in the examination of fundus blood vessels.With the clinical application of OCTA, its application in retinal and choroidal vascular diseases is more and more widespread.It can clearly display the characteristics of retinal and choroidal vascular morphology, so it has strong application value in the research of retinal and choroidal vascular diseases[23].In a study comparing the density of superficial retinal microvessels in patients with aCSC and controls, Yuet al[24]found that the density was reduced in patients with aCSC.Podkowinskiet al[25]showed that deep retinal capillary density and vascular perfusion in the SRF region were decreased in aCSC, and these changes may lead to chronic changes in the microvascular system and potential morphological changes.Previous studies have shown that changes in vascular density and FAZ are related to the course and prognosis of some retinal diseases[26].Reichet al[27]showed that patients with aCSC had reduced blood flow in the CCL.Therefore, this study observed SRVD,DRVD, superficial and deep FAZ area, the perfusion area of CCL before and after SML treatment to evaluate its therapeutic effect.After SML treatment, we can find that SRVD, DRVD and the perfusion area of CCL of patients has increased, and the area of superficial and deep FAZ has decreased, while in the observation group, only DRVD has increased.At 3mo,we found in the comparison of two groups, the changes of SRVD, DRVD and perfusion area of CCL of SML group were better than those of the observation group.Under physiological conditions, the choroidal capillaries provide oxygen and metabolic exchange to the outer retina, including the RPE and photoreceptors.The retinal circulation provides about 15% of the metabolic activity of the inner segment of the photoreceptors[28].Therefore, both retinal and choroidal circulation provide nutrients for photoreceptors to maintain their normal metabolism.Our study demonstrated that SML could effectively improve retinal and choroidal blood circulation.This suggests that SML is effective in treating aCSC.The change in DRVD in the observation group shows that aCSC can heal itself to a certain extent.At the same time, we can see that the SFCT in the observation group also decreased compared to baseline at the last follow-up, and there is no significant difference between the observation group and the SML group.RPE has significant paracrine influence on the retina, and likely choroid, while there is little to none in the choroid itself, repair of RPE and improvement of the choroid may have occurred in both the SML group and the observation group.At the same time, we cannot ignore that choroidal thickness is affected by many factors, such as age, axial length,intraocular pressure, and may fluctuate at different time points within a day.The area of superficial and deep FAZ decreased after SML treatment, but the difference was not statistically significant compared with the observation group.This may be because SRF mainly exists in the fovea of the macula, and the absorption of SRF here is the slowest, which has the greatest impact on the structure and function of the fovea.In addition,the capillary damage or morphological changes of FAZ caused by ischemia and hypoxia in the macular area require a longer time to repair, however, the observation time of this study is shorter, the recovery of the superficial and deep FAZ may take longer.
In recent years, microperimetry has been widely used in fundus diseases.It combines fundus morphology examination with retinal function examination to detect visual field changes caused by macular disease and evaluate visual function[29].CSC is a fundus disease mainly affecting the macular area.In the past, central vision was used to evaluate the function of the macular area, but the central vision only reflected the function of the fovea, and there was a lack of corresponding detection methods for the parafovea and perifovea.MP-3 microperimetry can measure RLS in a larger range, and is not affected by eye movement and fixation stability.Ⅰn this study,compared with before treatment, BCVA, CRT and RLS in SML group were significantly improved 3mo after treatment,and were significantly higher than those in the observation group, however, in the observation group, only CRT was reduced, BCVA and RLS at the last follow-up were not significantly different from baseline.This shows that SML can effectively protect and even improve the visual function of the lesion area while promoting the absorption of SRF in patients with aCSC.The improvement in visual function may be due to the absorption of SRF, which improves the physiological environment of retinal cells, restores the physiological function of retinal cells and intercellular synaptic connections, and improves the function of visual signal transduction pathways.Ⅰşık[22]observed the efficacy of SML in the treatment of chronic CSC and found that SML promoted the absorption of SRF and provided significant anatomical and functional improvements,which is consistent with the results of this study.However,in our study, we used microperimetry to evaluate the therapeutic effect of SML more objectively, and used OCTA to quantitatively analyze the blood flow changes of the retina and choroid and the changes of FAZ area.This made the changes of retina and choroid before and after SML treatment more intuitive to show in front of us, and provided us with a deeper understanding of the pathophysiological mechanism of CSC.
In this study, SML showed good efficacy and safety in the treatment of aCSC.In fact, at present, SML has been used in a variety of fundus diseases, including diabetic macular edema and retinal vein occlusion secondary macular edema[30-31].In recent years, some scholars have proposed to use SML for panretinal photocoagulation to treat diabetic retinopathy,and SML has also been reported to be used in the treatment of retinitis pigmentosa and secondary macular edema after cataract surgery[32-33].In the research of these diseases, SML also shows great potential, but more clinical studies are still needed to confirm.This study still has some limitations.First,the follow-up time is short, and the long-term effect of SML treatment cannot be observed.Second, the sample size is small and there may be bias.In addition, we manually measured the FAZ area of the superficial and deep retina, which may affect the accuracy of the measurement.
In summary, we believe that 577 nm SML treatment can make the SRF rapidly absorbed, ameliorate visual function, improve retinal and choroid blood flow.Moreover, it will not produce laser spot on the retina, is safe and effective.SML is beneficial to shorten the course of disease and improve the prognosis,and has unique advantages in clinic due to its low price, few complications and repeatable treatment characteristics.It is believed that SML will be used in the treatment of many eye diseases in the future.It will have a broader application prospect.
ACKNOWLEDGEMENTS
Conflicts of Interest:Guo JJ, None; Li XJ, None; Wan JJ,None.
 International Journal of Ophthalmology2023年6期
International Journal of Ophthalmology2023年6期
- International Journal of Ophthalmology的其它文章
- Role of 7-methylxanthine in myopia prevention and control: a mini-review
- How internal limiting membrane peeling revolutionized macular surgery in the last three decades
- Photoreceptor changes in Leber hereditary optic neuropathy with m.G11778A mutation
- Efficacy of ripasudil in reducing intraocular pressure and medication score for ocular hypertension with inflammation and corticosteroid
- Different serum levels of lgG and complements and recurrence rates in IgG4-positive and negative lacrimal gland benign lymphoepithelial lesion
- Subconjunctival conbercept for the treatment of corneal neovascularization
