Evaluation of adolescent/youth-friendly sexual and reproductive health services: A 7-year systematic review from January 2016 to April 2022
Oladayo Damilola AKINWALE,Cecilia Bukola BELLO,Oluwaseyi Abiodun AKPOR,Mayowa Grace ELEMILE
Department of Nursing,Afe Babalola University,Ado-Ekiti,Ekiti State,Nigeria
ABSTRACT Adolescent/youth-friendly sexual and reproductive health services (SRHS) play a vital role in reducing morbidity and mortality associated with adolescent SRH.This review examined studies carried out on adolescent/youth-friendly SRHS with focus on availability,accessibility,utilization as well as perception of health care providers,and adolescents about the services.The study design was systematic review of empirical studies using a well-defined strategy.Online journal was searched comprehensively using Web of Science,Google Scholars databases,PubMed,Medline,and EMBASE.Other sources were identified through the scanning of references of selected sources.The articles selected were between 2016 and 2022 and had qualitative/quantitative and mixed methods.The articles that met the selection criteria were also screened using PRISMA-P guidelines and SPIDER framework for systematic review was further used for inclusion criteria based on the following concepts: sample,phenomenon of interest,design,evaluation and research type.A total number of 32 studies were included in the study and findings were reported based on the five emerging themes.The review showed that majority of the adolescents were not aware of adolescent/youth-friendly SRHS,some health care providers were not also in support of the services which accounted for low utilization of the services among adolescents.The review further showed poor accessibility and nonavailability of AYFSRHS as the only available SRHS were meant for married adults.Therefore,these findings serve as evidence for policy-makers at all the levels of healthcare delivery system to considered all the factors observed in this review and develop strategies that will make adolescent/youth-friendly SRHS available and accessible to adolescents.More so,other stakeholders,especially health care providers must improve their attitude toward provision of adolescent/youth-friendly SRHS.
Keywords: Accessibility,adolescent,availability,healthcare providers,sexual and reproductive health,utilization
INTRODUCTION
Health care needs of adolescents are different from adults needs,especially in the aspect of sexual and reproductive health (SRH) and right.[1]This is due to the fact that adolescents need information,counseling,and other services to respond to their challenges as they transit to adulthood.[2,3]Therefore,neglecting their specific needs can lead to negative outcomes such as drug abuse,unwanted pregnancy,unsafe abortion,dropping out of school,sexually transmitted infections (STI) including HIV,and sexual and gender-based violence.[4]However,despite the recognition of the right of the adolescents to SRH information and services,many adolescents and young people still face challenges in accessing adolescent and youth-friendly sexual and reproductive health services (SRHS) in most public health institutions.[5]According to Demographic Health Survey,one in every five adolescent girls between the ages 15-19 years have started bearing children and about 20,000 girls visit health care facility for abortion related complications each year,while unsafe abortion remains the leading cause of maternal mortality and morbidity,especially among this age group,especially girls below 20 years.[6]The National AIDS Control Council estimated that 29,000 youth aged between 15 and 24 years get infected with HIV/AIDS every year while 17% of all AIDS-related deaths occur among adolescents and youth.[7,8]These negative health outcomes among adolescents and youth can be attributed to early sexual debut;risky sexual behaviors such as unprotected sex and multiple sexual partners;sexual and gender based violence;poverty;and harmful retrogressive cultural practices.[9-11]
Moreover,despite the clear imperative to improve youth-friendly services,discomfort surrounding adolescent sexuality commonly results in barriers to essential health care like SRHS.[12-15]Many young people lack comprehensive and correct information on their sexuality largely because of the embarrassment,silence and disapproval of open discussion of sexual matters by adults,including parents and teachers.[16,17]Consequently,many are unlikely to seek SRHS and when they do,they do not get the required services either due to the judgmental nature of health care providers,concerns around privacy and confidentiality,or low capacities of the health care system.[5,15]Especially social norms may cause adolescents to fear stigma,discrimination,or lack of respect when accessing services.[18]
In addition,related obstacles faced by adolescents include poor knowledge about service availability,accessibility of the services,the cost of receiving services,and lack of confidentiality.[19,20]Even where adolescents can and do access SRHS,they are often poorly coordinated and of low quality which consequently lead health workers to impose unnecessary restrictions on adolescents;for example,refusing to offer long-acting contraceptive methods.[21,22]Investing in adolescent and youth-friendly SRHS is crucial,yet,these obstacles often dissuade adolescent and youth from accessing SRH information and services that could help them prevent unplanned pregnancy and STI including HIV.[23]Therefore,there is a particularly critical need to improve access to adolescent and youth-friendly SRHS in West Africa including Nigeria where adolescent girls have the lowest contraceptive prevalence (34%) among nonmarried sexually active adolescents and 20% among married adolescents and the highest maternal mortality rates in Africa.[24]
Furthermore,complications in pregnancy and childbirth are the leading cause of death among women aged 15-19 years,and infants born to young mothers are more susceptible to life-threatening complications.[25]Girls and young women with children are often denied opportunities to attend school and earn an income.[23,26]In turn,they,their families,and their communities are more likely to live in poverty.In order to ensure access to adolescent and youth-friendly SRHS,effective utilization of adolescent/youth-friendly SRHS and quality assurance in providing adolescent and youth-friendly services in line with the WHO recommendation that adolescent/youth-friendly SRHS must be accessible,acceptable,equitable,appropriate,and effective for adolescents and youth.[27-30]Therefore,this review aims at exploring studies carried out on adolescent/youth-friendly SRHS and to identify the gap in providing adolescent/youth-friendly SRHS across the world and particularly in Nigeria.
METHODOLOGY
Protocol
This is a 7-year systematic review of adolescent/youth-friendly SRHS.This systematic review was conceptualized and carried out from year 2016 to 2022 in accordance with the Preferred Reporting Items for Systemic Review and Meta-Analysis Protocol.[31]The protocol of this review was registered on PROSPERO with the registration protocol number 322965 and the methods of screening inclusion and exclusion criteria and analysis were developed following the protocol.This checklist consists of four broad outlines highlighting the background of the study (contextual literature review,research questions,or aims),methodology (quality criteria and assessment including data synthesis),results (characteristics of included studies and study flow),and discussion.[32]Data extracted from each study include authors name,publication source and year;country,participants and demographics (age and gender),objectives/aim,methodology (study design,settings,samples,and instruments),outcome,and key findings.The findings were summarized in narrative synthesis and presented in table below.
Data search
Studies were screened using predefined selection criteria;Studies using English language;Published articles in peer-review journals on awareness and utilization of adolescent SRHS by adolescents,perception and attitude of health care providers on adolescent SRHS,awareness and knowledge of health care providers on standards and guidelines for providing adolescent SRHS;availability and accessibility of adolescent SRHS in primary health centers;availability and implementation of standards and guidelines for providing adolescent SRHS in primary health care facilities as well as factors influencing the utilization of adolescent SRHS.Online journal was searched comprehensively by using Web of Science,Google Scholars databases,PubMed,Medline,and EMBASE.Other sources were identified through scanning of references of selected sources.The search terms are shown in Table 1.
Inclusion criteria
The researcher reviewed peer-review journal articles with empirical data reporting findings on awareness,knowledge and utilization of adolescent SRHS,perception and attitude of health care providers on provision of adolescent SRHS,availability,accessibility and factors influencing adolescent/youth-friendly SRHS in high-and middle/low-income countries.The articles selected were between 2016 and 2022 and had qualitative/quantitative and mixed methods.Qualitative research studies included were those that utilized focus group discussion and in-depth interview while quantitative research studies included were those that used descriptive research design among adolescent aged 12-19 years and health care providers in both urban and rural areas.This review also included only primary studies on youth friendly SRHS;availability,accessibility,and utilization that were published in the English language.Although most of the reviewed articles targeted adolescents aged 10-19 years,the researcher also included young people aged 20-24 years as well.
Exclusion criteria
The following categories of published articles were excluded from the review: systematic review or narrative review,case reporting,letter to the editor,article written in other languages than English and any article with participants predominantly >24 years or <10 years or with unclear ages.
Data screening
Title and abstract screening of all papers identified by the search strategy were carried out with reference to the published inclusion and exclusion criteria.The key findings were compiled for each study and were grouped based on common traits.
Quality assessment and appraisal of included articles
This is essential to ensure that the findings of the paper are correct and accurate.All the articles that meet the eligibility criteria were assessed for quality.The included studies were appraised critically for methodological quality and rigor using critical appraisal skill programme checklists with focus on the study design,sampling methods,data analysis,participant recruitment strategies,instrumentation,and findings [Table 2].

Table 1: List of search terms
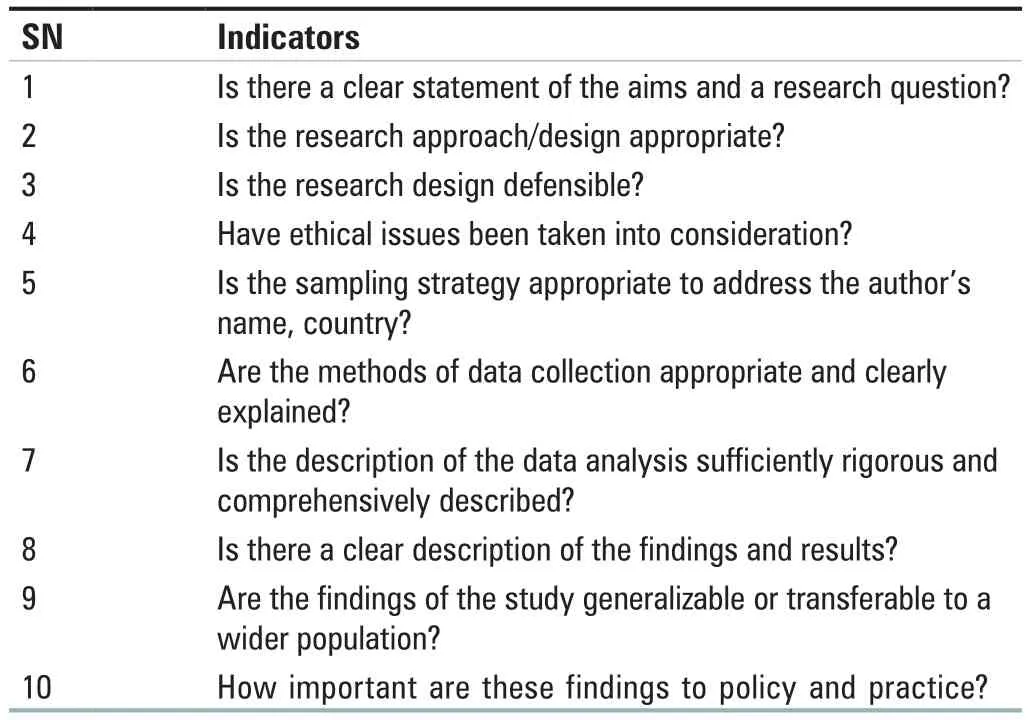
Table 2: Quality appraisal indicator
Data extraction
The data extraction spreadsheet was created using Microsoft Excel to record systematically all relevant studies identified.The common extraction tool was used for all studies with variation depending on the research design.The data extraction headings included were author name,publication source,year of publication,study setting,study location/country,aim and objectives of the study,participants and demographic,study design,sample,instrumentation and outcomes,analysis used,and key findings.The lead reviewer screened each title,extracted data and assessed the quality of all included studies.The extracted sheet was finally cross-checked by the second reviewer and inconsistencies were resolved by consultation with the third author.As part of extraction process,each qualitative and quantitative study was assessed for methodological rigor.Thus,the retrieve data were analyzed to answer the main research and specific objective.
Data synthesis
The findings from included studies were summarized in a narrative statement and presented in the result table and discussion of findings.
Framework used for this review
Following the selection of eligible studies,the articles that met the selection criteria were also screened using PRISMA-P guidelines and SPIDER framework for systematic review was further used for inclusion criteria based on the following concepts: sample,phenomenon of interest,design,evaluation and research type.This provides final inclusion criteria for the review,as shown in Figure 1.
RESULTS
A total number of 30,500 studies were identified on adolescent SRHS through the database search.A total number of 32 studies were finally included in the review [Figure 2].Twenty-six were conducted in Africa out of which eight were from Nigeria,five in Asia,and one from Europe.Table 3 summarizes the studies included in the review with the author’s name,year,country,title,objectives,research design,sample,instrument,and findings.The findings and emerging themes were included in the study.
Ten studies used mixed method approaches with cross-sectional design which was considered appropriate for the studies included,although four studies did not clearly state the specific design used for the study and one study used case study approach which is considered inappropriate for mixed method approach.All the included studies indicated the sample size but participant recruitment strategies and sampling techniques were not properly stated.The instruments used for the studies were considered accurate and appropriate;six studies used adapted questionnaire and checklist for their studies.As regards study participants,seven studies used three set of participants: adolescents,health care providers and health care facilities;four used adolescents and health care providers;however,18 used adolescents only while 3 used only health care providers.Out of the reviewed articles,five studies were carried out on awareness and knowledge of adolescent on adolescent/youth-friendly SRHS,eight discussed utilization of adolescent/youth-friendly SRHS,five explain perception and attitude of healthcare providers,availability,and accessibility of adolescent/youth-friendly SRHS was also discussed by five studies included in the review.However,few of the study combined more than two concepts to explore adolescent/youth SRHS.
DISCUSSION
Five themes emerged from the analysis and synthesis of the data as documented on adolescent SRHS.These themes include (1) awareness and knowledge of adolescents on SRH and services;(2) perception and attitude of health care providers toward utilization of adolescent SRHS;(3) utilization of adolescent/youth-friendly SRHS;(4) availability,accessibility,and quality of adolescent/youth-friendly SRHS,and (5)factors as barriers and challenges influencing utilization of adolescent/youth friendly SRHS among adolescents.

Figure 1: Systematic review framework

Figure 2: PRISMA flow diagram showing study selection process
Awareness and knowledge of adolescents on sexual and reproductive health and services
Studies on level of awareness and knowledge of adolescents on adolescent SRHS indicated low level of awareness of SRHS among adolescents which was attributed to lack of information on where to access the services and whom the services are meant for,poor and moderate knowledge was also reported by the studies included in this review.[33]This suggests that adolescents have low level of awareness and knowledge about adolescent SRHS.A study identified knowledge gap on myth and poor knowledge about HIV transmission,contraceptive methods and other SRH issues affecting adolescents.[34]On a general note,all the studies included in this review reported low level of awareness and knowledge of adolescents on SRH and services.[35-37]However,there was lower SRH knowledge among rural adolescents compare to urban district.Among sexually active adolescents,35.2% used contraception.
Perception and attitude of health care providers toward adolescents’ utilization of adolescent SRHS
Out of several studies conducted on perception and attitude of health care providers on utilization of adolescent/youth-friendly SRHS by the adolescents,five met criteria for inclusion and were analyzed.The findings from these studies showed that majority of health care providers were generally supportive of adolescents who asked for and used contraceptives.[38]However,noncompliance to family planning regimens and repeated requests for termination of pregnancies were perceived by nurses as irresponsible behaviours which were particularly frustrating to them and not in concordance with their personal values.[38]In addition,a study on health care professionals’ attitudes toward youth-friendly SRHS conducted in Jordan revealed that providers’ attitudes toward youth-friendly SRHS highlighted content-specific and cultural concern about SRHS provided to adolescents.[39]
This review thus explains the role cultural concern plays in influencing providers’ attitudes towards the provision of adolescent SRHS.Health care providers appear to have the least favorable attitude toward issues specifically related to youth sexuality,especially among unmarried youth.For instance,religion principles prohibit sexual relationship outside marriage and the discussion of sexuality is generally considered a taboo according to traditional norms of stigmatizing youth sexuality despite the providers’ responsibility to provide care.[39,40]However,physicians exhibited significantly more youth-friendly attitude than nurses and providers who have been previously trained in SRH issues.There was no difference between providers’ characteristics.[39]Furthermore,sexual reproductive health nurses indicated that they are experiencing challenges with the concept and practice of termination of pregnancy for unmarried adolescents which denotes that the practice contradicts their opposing beliefs and values.Other challenges influencing the attitude of health care providers include lack of time to provide necessary care to the adolescents,limited access to where adolescents can be reached and lack of periodic training on adolescent SRH.[41]

Table 3: Adolescent/youth-friendly sexual and reproductive health services
Contd...
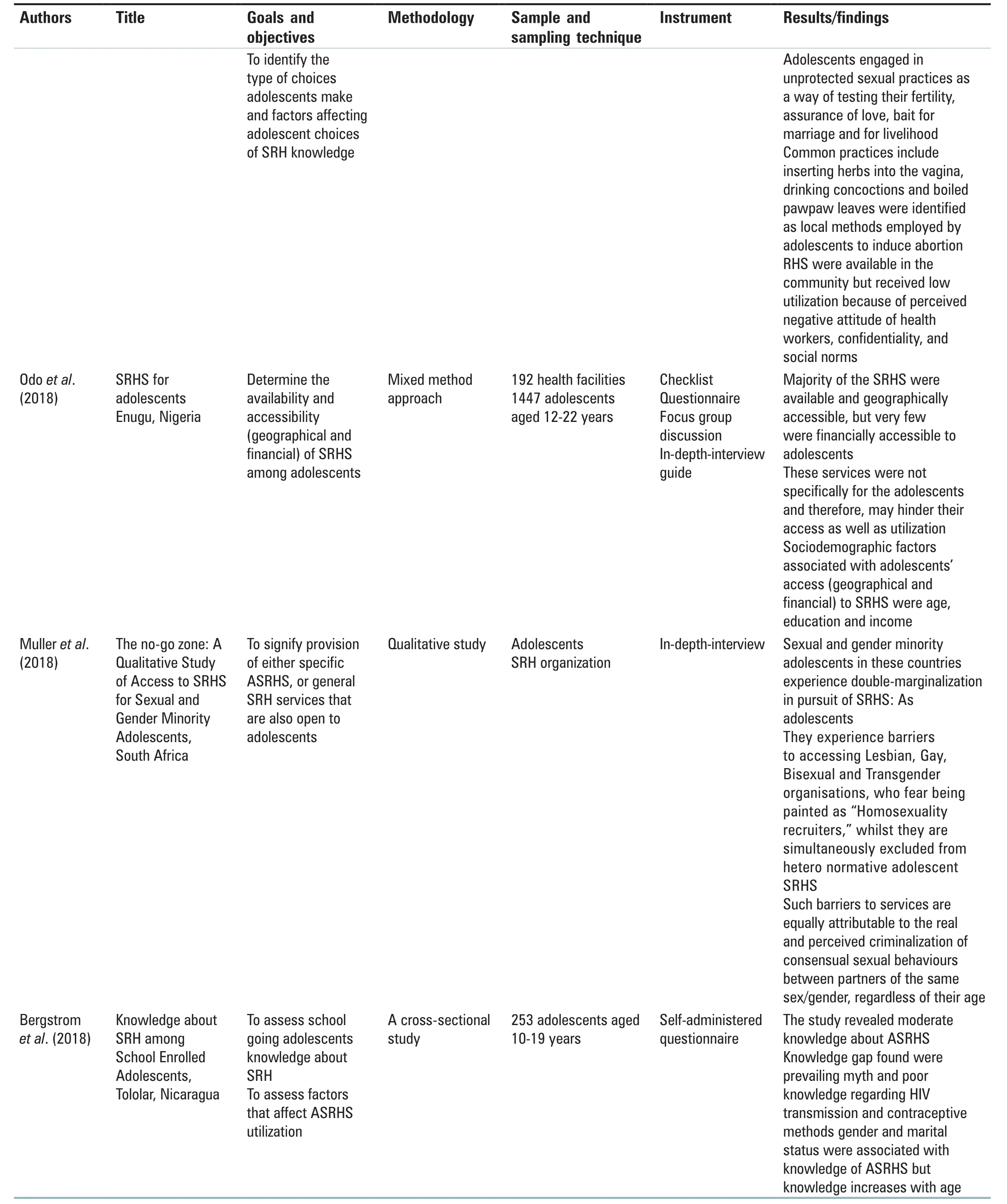
Table 3: Contd...
Contd...

Table 3: Contd...
Contd...
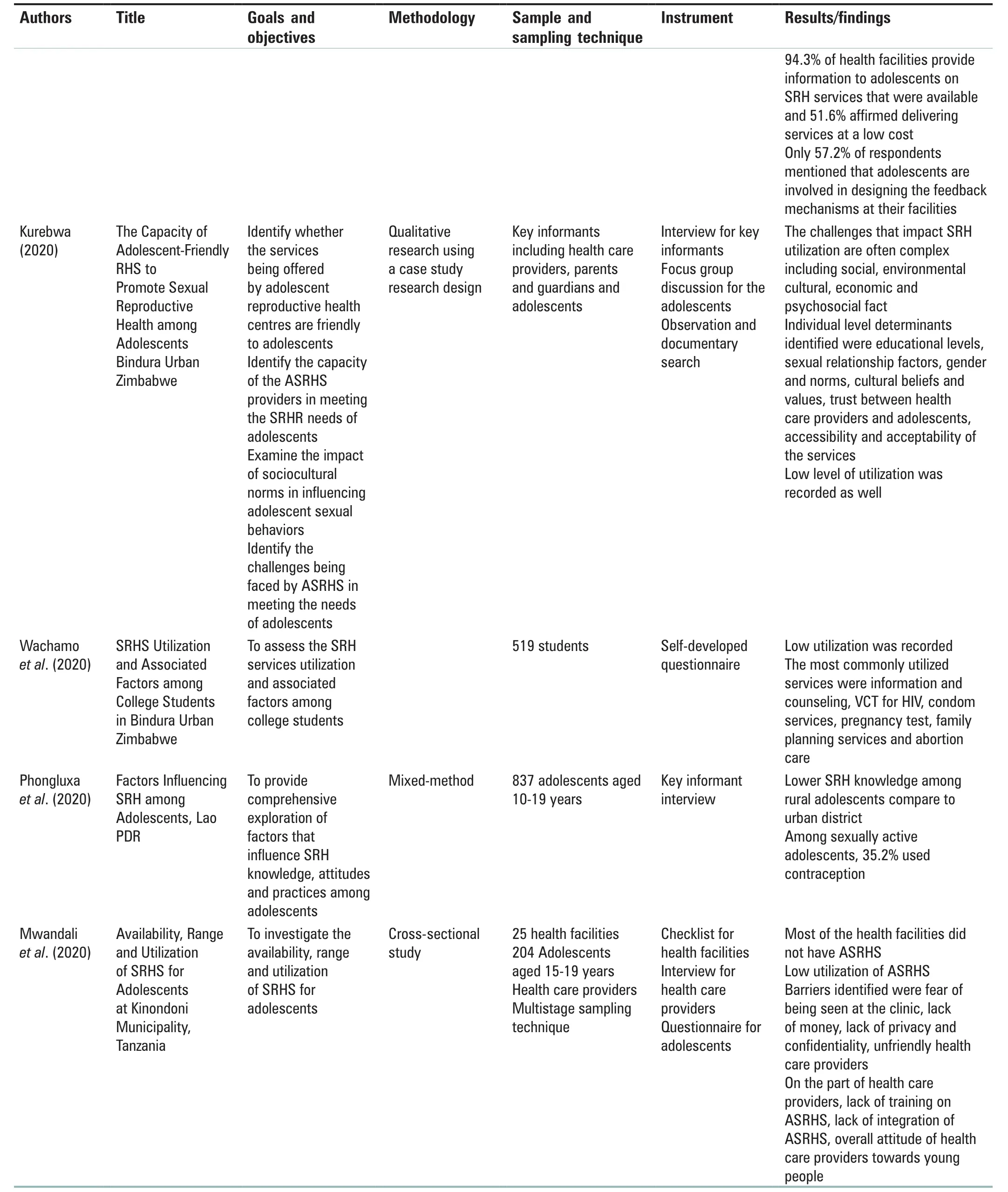
Table 3: Contd...
Contd...

Table 3: Contd...
Contd...

Table 3: Contd...
Contd...

Table 3: Contd...
Utilization of adolescent/youth-friendly sexual and reproductive health services
Studies on utilization of adolescent SRHS revealed low level of utilization by the adolescent/youth.[23,24,42-50]However,the studies conducted by Owoeye and Nwaogwugwu[42]and Abdurahmanet al.[43]were conducted among secondary school adolescents excluding out-of-school adolescents which therefore,may not be generalized to all adolescents.In the other studies,Mbachuet al.[46]and Tilahunet al.[24]reported that low utilization of adolescent/youth-friendly SRHS by the adolescents was associated with the fact that patent medicine vendors were the most visited type of facility for SRHS information and other services.Contrary to those studies,Ssebadduka and Nanyingi[51]reported high utilization of adolescent/youth-friendly SRHS among youths who have ever had adolescent/youth-friendly SRHS problems.However,some reasons for their failure to utilize the available adolescent and young SRHS were as follows:long distance to service centers;unfriendly and judgmental healthcare providers;drug stock-outs at health units;negative attitude by youth towards the use of adolescent and young SRHS;fear to be stigmatized or discriminated against and traditional beliefs.The factors found to be significantly associated with adolescent and young SRHS utilization include: being a teenager,being out-of-school,agreeing that religion approves youth to seek adolescent and young SRHS;and disagreeing that contraception use encourages promiscuity.
Accessibility,availability,and quality of adolescent/youth-friendly sexual and reproductive health services
Low accessibility to adolescent/youth-friendly SRHS was reported low by several included studies in this review.This is reflected in the level of utilization of the services which was associated with three main level of factors: individual level factors such as inadequate knowledge about types of SRHS,poor attitude towards RHS and certain risky behavior of adolescents;social level factors include parental influence,community and religion norms,financial constraint and stigma attached to adolescent utilization of SRHS;health system factors include poor health workers attitude and inconvenient opening hours.[49]
The study conducted by Mwandaliet al.[45]reported that most of the health care facilities did not have adolescent SRHS and SRHS available were meant for adults,especially married women of reproductive age.Envuladuet al.[52]reported that majority of the facilities in the state lacked dedicated space,basic equipment,and essential SRH care services for adolescents.
Factors influencing utilization of adolescent/youth-friendly sexual and reproductive health services among adolescents
Low utilization of SRHS among adolescents was attributed to unavailability of services within 30 min of walking distance,[53]Other factors identified from included studies were fear of family and society as well as socio-cultural norms and stigma.One study highlights the barriers associated with low utilization of adolescent/youth-friendly SRHS which included individuals factors,social factors and health system factors,as previously stated.In addition to this,Iloriet al.[48]identified that lack of information on where to access the services was a significant factors influencing the utilization of adolescent SRHS.
In addition,interpersonal determinants identified were schooling status,parents being alive;institutional determinants were timing of opening of the facilities.[44]Other determinants were lack of privacy and confidentiality,unfriendly attitude of health care providers.[44]The factors that promote utilization of adolescent SRHS include knowledge and awareness of SRHS,peer influence and attitude of health care providers.[50]Mwandaliet al.[45]identified barriers to low utilization of adolescent SRHS as fear of being seen at the clinic,lack of money,lack of privacy and confidentiality,and unfriendly health care providers among adolescents while lack of training on adolescent SRHS,lack of integration of adolescent SRHS,overall attitude of health care providers toward young people were reported among health care providers.
This review also identify poor knowledge,attitude and practice of SRH and services among adolescents with a significant relationship between gender,religion,education,and knowledge of SRHS;significant association between age,occupation of household head,and attitude toward SRHS as well as practice of adolescent SRH being associated with categories of adolescents’ schools.[24,36]Furthermore,knowledge gap was identified as the barriers to utilization of adolescent/youth-friendly SRHS as the knowledge of reproductive health choices was low among respondents.Majority of adolescents relied on their peers for information on SRH,had sexual partner(s) and engaged in premarital sex,which was common and viewed as normal.[24]Adolescents were also found to engage in unprotected sexual practices as a way of testing their fertility,assurance of love,bait for marriage and for livelihood.Common practices including inserting herbs into the vagina,drinking concoctions and boiled pawpaw leaves were identified as local methods employed by adolescents to induce abortion.Reproductive health services were available in the community but received low utilization because of perceived negative attitude of health workers,confidentiality,and social norms.[33]
The significant predictors identified from these review include sociodemographic characteristics of age,level of education,income and living status,psychocultural and health system factors,which are predictors of young people’s utilization of SRHS.[54]In general,factors influencing utilization of adolescent/youth-friendly SRHS are grouped into three: socio-demographic factors of the adolescents,and health care providers;socio-cultural factors embedded in beliefs,values and norms;and health system-related factors.This is supported by the studies conducted by Odoet al.[54]that identified structural,individuals,socio-economic and socio-cultural factors as the major factors influencing utilization of adolescent/youth-friendly SRHS.However,individual factors are associated with incorrect knowledge of SRHS,including myth and misconceptions around contraception,limited self-efficacy,and individual agency,constraints ability to navigate internalized social and gender norms,and lack of access to information about what SRHS are available and where to seek services.Structural barriers are associated with laws and policies requiring parental or partner consents,distance from facilities,cost of services,inconvenient hours,cost of services and transportation,long waiting hours for the services,lack of necessary commodities at health facilities,and lack of privacy and confidentiality.Cultural factors are restrictive norms and stigma associated with adolescents and youth sexuality,inequitable or harmful gender norms,discrimination and judgment by the communities,families,partners and providers while socio-economic factors were embedded in pressure that prevent low class individuals from moving over the course of receiving better SRH like high class individuals.[55]
CONCLUSION
This review has shown that most adolescents were not aware of SRHS for the adolescents neither were they knowledgeable about forms of SRHS meant for them and where to visit when in dare need of the services.This was associated with myth and misconceptions regarding sexuality education for the adolescents and youth,fear to be stigmatized or discriminated against and traditional beliefs,adolescent being out of school,peer influence,fear of being seen at the clinic.This accounts for low utilization of SRHS among adolescents.According to this review,nearly all the included studies reported low utilization of adolescent SRHS.This suggests that there is low utilization of adolescent/youth-friendly SRHS among adolescents despite the need for the services.
Furthermore,regarding the perception and attitude of health care providers,this review revealed that some health care providers were in support of adolescent/youth-friendly SRHS for adolescents who seek for the services to avoid noncompliance with family planning regimen of adolescents and repeated request for termination of pregnancy.However,on a general note,according to this review,perception and attitude of health care providers were considered cultural concern about SRHS provided to adolescents as sexual behavior among unmarried adolescents is against the cultural norms and belief.This serves as a challenge in providing adolescent SRHS.Furthermore,poor accessibility and availability of adolescent/youth-friendly SRHS was reported from this review,most of the studies conducted on availability and accessibility of adolescent/youth-friendly SRHS reported nonavailability of SRHS for the adolescents and the little available SRHS in health care facilities were meant for the adult,especially married women not for the adolescents,most of the health facilities also lacked dedicated space,basic equipment and essential SRHS for adolescents.
Factors associated with poor utilization of adolescent/youth-friendly SRHS based on this review are grouped into three: adolescent factors which include socio-demographic factors such as age,level of education;socio-economic factors,lack of awareness and knowledge about SRHS,lack of knowledge about where to seek SRHS;health care providers factors such as personal principles,norms and belief as well as religious inclination of health care providers,providers characteristics like poor perception,unfriendly attitudes,judgmental attitude,lack of time,privacy and confidentiality required to provide services to the adolescents,limited access to where adolescents can be reached as well as lack of periodic training on SRHS.Health care facilities factors include accessibility like long distance to service centers,inconvenient opening hours;availability such as lack of equipment,drug stock-outs at health units;negative attitude by youth towards the use of SRHS,lack of integration of adolescent SRHS.Finally,policy factors is also associated with utilization of adolescent SRHS,like laws and policies requiring parental or partner consents,lack of training on adolescent SRHS,lack of integration of adolescent SRHS into national health policy.Therefore,there is a need for collaboration between the stakeholders including the three levels of health care facilities to ensure that adolescent SRH is given priority in health care system to avoid consequences attached to failure to provide these services to the adolescents.
Based on this review,it is therefore recommended that there should be provision of more adolescent-specific IEC materials that use fewer technical terms and more language that adolescents could understand;provide the materials in the local language and include images of happy,healthy adolescents;and make them available throughout the health facilities.Use media,such as television,to provide information to adolescents.Moreover,there should be provision of in-services training for health care providers on adolescent/youth-friendly SRHS.Although health care providers are conversant with SRHS,however,there is a need for effective training on adolescent/youth-friendly SRHS to ensure effective utilization of the services.There is also need for health care facilities to be equipped with adequate staff including clinical personnel,counselors,and peer educators to ensure effective use of adolescent/youth-friendly SRHS,and there should be provision of standard and guidelines for providing adolescent SRHS that will spell out the right of the adolescents and role of health care providers in providing SRHS for the adolescents.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 Journal of Integrative Nursing2022年4期
Journal of Integrative Nursing2022年4期
- Journal of Integrative Nursing的其它文章
- Symptom experience in patients with cancer-related fatigue: A systematic review and meta-synthesis
- Drivers of early marriage and teenage pregnancy in Kenya and Uganda during COVlD-19 lockdown period:A systematic review
- Dredging hand Yang meridians with deep tissue massage combined with neck movement in stiff-neck syndrome:A randomized controlled trial
- Quality of life and psychological impact among chronic disease patients during the COVlD-19 pandemic
- Job satisfaction and organizational commitment among nurses working on temporary versus permanent jobs at a tertiary care teaching hospital,Uttarakhand,lndia
- Nursing students’ experiences of horizontal violence and occupational belonging during clinical placements
