Effect of cold snare polypectomy for small colorectal polyps
Qing-Qing Meng,Min Rao,Pu-Jun Gao
Abstract
Key Words: Colorectal polyps; Cold snare polypectomy; Hot snare polypectomy; Complete polypectomy rate; Immediate bleeding; Delayed bleeding
lNTRODUCTlON
Colorectal cancer is one of the most common malignant tumors of the digestive tract, and has gained more attention in recent years due to its increasing morbidity and mortality[1,2]. Approximately 60%-80% of colorectal cancer is caused by intestinal polyps, and resection of intestinal polyps has been proved to reduce the incidence of colorectal cancer[3]. The vast majority of intestinal polyps can be found during colonoscopy and removed endoscopically. Therefore, more attention has been paid to the development of endoscopic resection of intestinal polyps. Ninety percent of polyps found during colonoscopy are < 10 mm in size[4], and the standard methods used to remove small polyps include biopsy forceps, cold snare polypectomy (CSP), and hot snare polypectomy (HSP). HSP is a popular method that has been used for many years and has a positive therapeutic effect[5]. The principle of HSP is the use a high-frequency current to generate a large amount of localized heat. The polyp is solidified and removed. In clinical practice, the range of injury caused by the current exceeds the range observed during the operation, and complications such as bleeding and perforation occur rapidly postoperatively[6]. Although CSP uses a snare to remove the polyps, without a high-frequency current, the incidence of delayed bleeding and perforation after the operation is low. Therefore, CSP is considered to be a safe operation with a high complete resection rate, and its clinical utilization rate has increased significantly. In 2017, the European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guidelines[7] recommended that colorectal polyps < 10 mm can be removed by CSP. The present study retrospectively analyzed patients with colorectal polyps 4-9 mm in size treated by endoscopy in our hospital between January to December 2020. We compared HSP and CSP, including surgical outcome and safety.
MATERlALS AND METHODS
Participants
A total of 249 patients who underwent colorectal polypectomy in the Endoscopic Center of the First Hospital of Jilin University between January and December 2020 were divided into the CSP group (n= 140) and HSP group (n= 109). Inclusion criteria were: (1) Age ≥ 18 years; and (2) Single or multiple polyps with a diameter of 4-9 mm, classified as 0-IS, 0-ISP and 0-IIA polyps using the Paris type classification. Exclusion criteria were: (1) Familial polyposis or inflammatory bowel disease; (2) Coagulation dysfunction or anticoagulant and antiplatelet drug treatment within 1 wk of the study; (3) Intestinal cleaning was insufficient; and (4) Suspected canceration. This research was approved by the Medical Ethics Committee of our institution.
Methods
Before the operation, both groups were prepared by consuming a liquid diet for 24 h followed by 2 L oral polyethylene glycol electrolyte solution, and simethicone was used to remove bubbles. Colonoscopy and treatment were performed by two experienced endoscopists with > 5 years of clinical experience. Patients were treated by standard colonoscopy or magnifying endoscopy (CF-H290I, CFHQ290I or PCF-Q290JI; Olympus, Japan), and colorectal polyps were identified by endoscopy. The location, size and shape of the polyps were recorded, and they were classified by Paris type[8]. The polyp size was estimated according to the open biopsy forceps opening or the fully open snare. In the CSP group, a unique cold snare (CAPTIVATOR II; Boston Scientific, United States) was used to capture the focus and normal tissues with a margin of 1-3 mm. When tightening the snare, it was pressed down toward the intestinal wall. The snare was then quickly tightened to mechanically remove the polyps and surrounding tissues[9,10] (Figure 1). Following an injection of saline at the base of the lesion (depending on the size of the polyp), the snare was used to trap the root of the polyp and was gradually tightened in the HSP group. The polyp was resected by electrocoagulation with a high-frequency electrotome (ERBE VIO200D), and specimens were recovered using a biopsy forceps or suction. According to the size of the wound and the presence or absence of active bleeding, titanium clips were used to clamp the wound. The location, size, quantity, operating time and complications of polypectomy were recorded in detail during the operation. The resected tissues were fixed with formaldehyde solution and then sent for pathological examination. The pathological evaluation of resected lesions was based on World Health Organization standards, and additional biopsy samples of lateral and basal margins were evaluated in detail for tumor involvement.
Observation indicators included the following: general characteristics of the patients and polyps in the two groups; complete polypectomy rate and recovery rate; operating time and use of titanium clips during the operation; and operative complications (including immediate bleeding during the operation, delayed bleeding after the operation, perforation during the operation and delayed perforation). Histologically complete resection was determined by histopathological evaluation of the resected polyp specimen and the biopsy specimen at the lower side of the polyp. Incomplete resection was defined as the presence of pathological tissue in the biopsy specimen, the lower side of the polyp specimen, or at the bottom and periphery of the resection site, and complete histological resection was defined as negative results for the above parameters[11,12]. The polypectomy time referred to the time from the preparation of instruments to the completion of specimen recovery. Immediate bleeding during the operation referred to bleeding for > 30 s after the operation and was stopped by endoscopy[13]. Delayed bleeding after the operation referred to bleeding requiring endoscopic intervention within 2 wk after polypectomy.
Statistical analysis
All analyses were performed using SPSS for Windows. The measurement data were expressed as the mean ± SD, and comparisons of means between the two groups were carried out using the independentt-test. Numerical data were expressed asn(%), and theχ2test or Fisher’s exact test was adopted, and the test standard (α) was 0.05.
RESULTS
General data
We enrolled 249 patients with 301 polyps. There were no significant differences in general data such as gender and age between the two groups (Table 1). One hundred and fifty-four polyps were identified in the CSP group and 147 in the HSP group (Table 2). There were no significant differences in polyp size, polyp location, morphological classification and pathological classification between the two groups.
Outcomes in each group
The CSP and HSP groups both had a high resection rate of impaired tissue integrity, and there was no significant difference between the groups (Table 3). Among the 10 cases of incomplete resection in the CSP group, two had tiny polyps of 4-5 mm, eight had polyps of 6-9 mm, seven had morphological type IIa and three had type I. There was no significant difference in tissue recovery between the two groups. The polyps in both groups in which recovery of tissues failed were all tiny polyps of 4-5 mm, and were located in the transverse colon and left side of the colon. In terms of titanium clip utilization rate and operating time, the CSP group was superior to the HSP group. In the HSP group, titanium clips were mainly used to prevent bleeding and perforation.
Complications
The immediate bleeding rate in the CSP group was higher than that in the HSP group (P< 0.05) (Table 4). No delayed bleeding was observed in the CSP group, but there were three cases in the HSP group (P< 0.05). These three patients with delayed bleeding did not bleed after secondary endoscopic therapy and clamping the wound with a titanium clip stopped the bleeding. One case of delayed perforation occurred in the HSP group, and the patient was discharged after conservative treatment. No intraoperative perforations occurred in either group.

Table 1 Baseline characteristics of the patients in each group
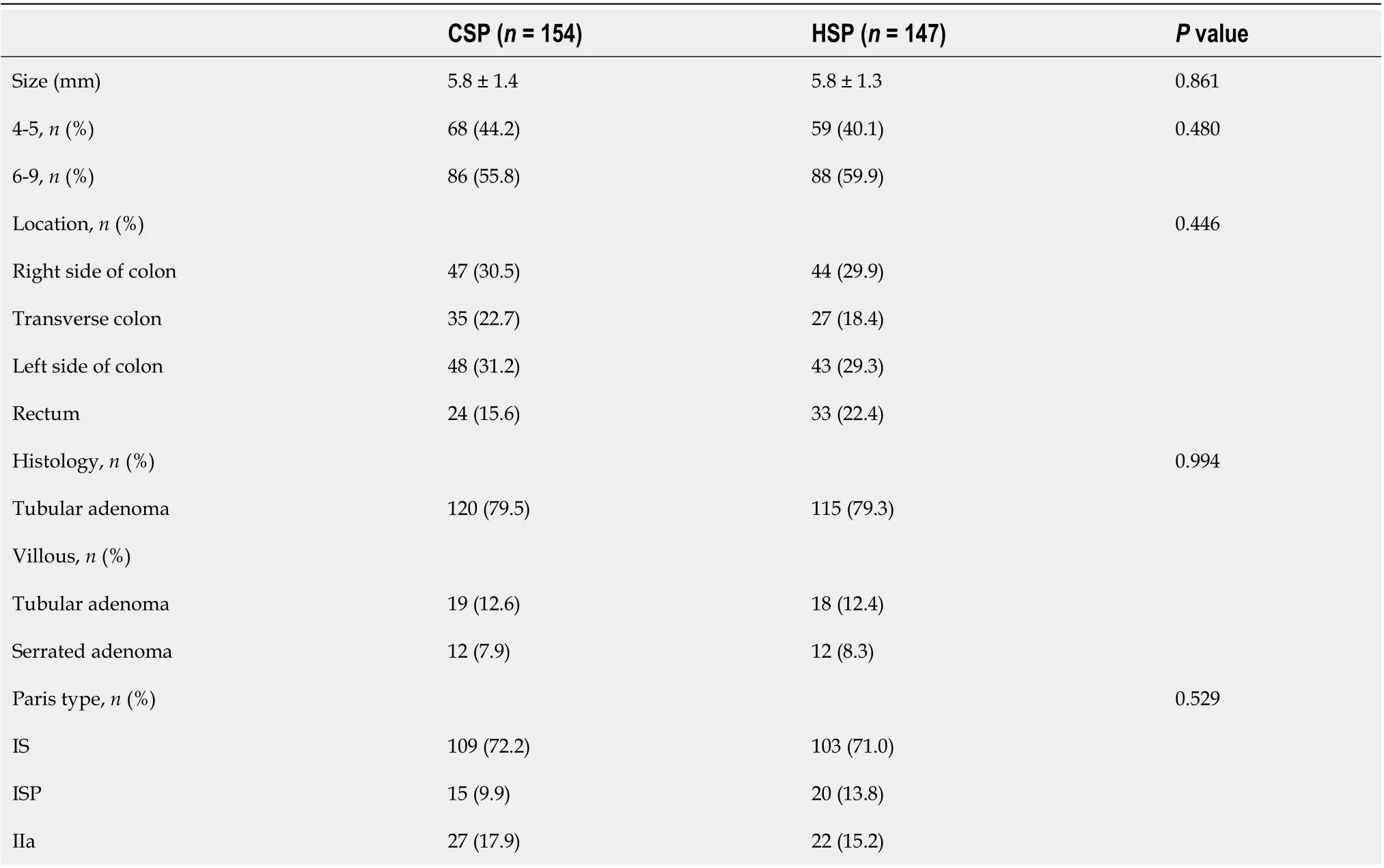
Table 2 Characteristics of the polyps
DlSCUSSlON
CSP was first proposed by Tapperoet al[14] in 1992. Due to the short operating time and fewer complications, especially the low incidence of delayed bleeding, CSP has attracted the attention of many endoscopic physicians and has been widely used. In the guidelines for colorectal polypectomy and endoscopic mucosal resection issued by the ESGE in 2017, CSP was recommended for sessile polyps < 10 mm. For colorectal polyps > 10 mm, the safety of CSP requires confirmation[15]. Recently, Murakamiet al[16] reported that the local recurrence rate after CSP for lesions < 10 mm and 10-14 mm was 1.4% and 5.4%, respectively; thus, CSP is not recommended for lesions ≥ 10 mm due to high rates of recurrence and malignancy. The ESGE guidelines were followed in our study. Colorectal polyps 4-9 mm in size detected during colonoscopy were randomly allocated to the HSP or CSP group in our study. Based on the patients’ general characteristics (age, gender, indication, preparation status, and endoscope used) and the characteristics of the polyps (location, morphology and size) being similar between the two groups, the rate of complications, complete resection and other results were compared between the CSP and HSP groups.
The most common complication of HSP and CSP is bleeding, which can be divided into immediate and delayed bleeding. Immediate bleeding is a common adverse event after CSP. A large prospective nonrandomized controlled trial by Repiciet al[17] reported that the immediate bleeding rate of CSP was 1.8%. Jegadeesanet al[18] reported that the immediate bleeding rate of CSP was higher than that of HSP (6.6%vs3.3%). In the present study, the immediate bleeding rate of CSP was 11.7%, which was higher than that in the HSP group (1.4%), but was similar to that in several previous studies[17,18]. It is suggested that this adverse event is not important clinically. As most sessile polyps are < 10 mm, there are few major vessels in the roots, bleeding usually occurs in venules or blood capillaries, and there is only minimal bleeding with spontaneous hemostasis a few seconds after mechanical cutting during CSP. Even in rare cases in which bleeding persists, endoscopic clipping is an effective management option. Delayed bleeding is often considered a common adverse event of HSP. Three postprocedural bleeding events occurred in patients who underwent HSP, and bleeding stopped in all patients after the second endoscopic intervention. A prospective study by Suzukiet al[19] observed the wounds after CSP and HSP. Although the size of the wound in the CSP group was larger than that in the HSP immediately after resection, 1 d later, the size of the wound in the CSP group was significantly smaller than that immediately after CSP. The sustained effect of HSP after electrocoagulation increased, suggesting that the wounds in the CSP group healed faster and were more conducive to reduced delayed bleeding compared with those in the HSP group. Surgical intervention or death rarely occurs due to delayed postpolypectomy bleeding[20], but delayed bleeding is thought to increase the risk and difficulty in emergency colonoscopy due to the presence of blood, and poor vision in the colon can lead to hospitalization, blood transfusion and repeated endoscopic hemostasis. The advantage of CSP is that immediate bleeding is easily identified and timely treated, avoiding secondary endoscopic intervention or surgical hemostasis, and obviating additional cost to patients. We found that clips had no advantage in preventing delayed bleeding after CSP, and the utilization rate of clips in the CSP group was only 15.6%. Except for immediate bleeding, clips were not used to prevent delayed bleeding, and no cases of delayed bleeding occurred in the CSP group. These results are similar to those reported by Kawamuraet al[21]. Therefore, for sessile polyps < 10 mm, we do not recommend the preventive application of clips during CSP.

Table 3 Outcomes in each group
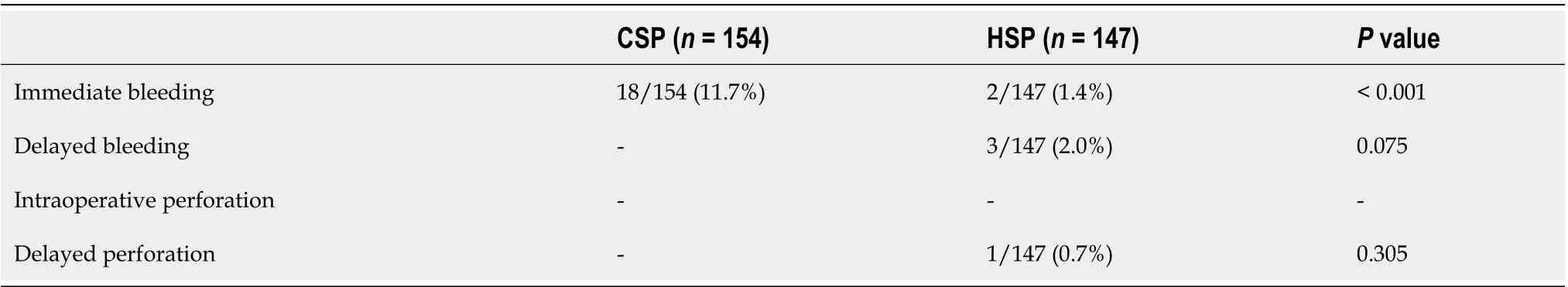
Table 4 Complications in each group

Figure 1 The process of cold snare polypectomy. A: Polyp approximately 0.7 cm in diameter identified under the white light of colonoscopy; B: Polyp observed under narrow band imaging; C: Tightening of the snare during cold snare polypectomy (CSP); D: Wound after CSP; E: Postoperative pathological tissue specimen.
Complete resection is now considered a powerful indicator of the quality of colonoscopy. Kawamuraet al[21] conducted a prospective, multicenter, randomized controlled, parallel, noninferiority trial in Japan to investigate the success rate of CSP for complete resection of 4-9 mm colorectal adenomatous polyps and compared the success rate with that of HSP. The complete resection rates with CSP and HSP were 98.2% and 97.4%, respectively, with no significant difference between the two groups. They then concluded that HSP and CSP resulted in the same complete resection rate for polyps < 10 mm by consulting the randomized controlled trials in PubMed and the Cochrane library[22]. However, some studies have shown that the complete resection rate was significantly lower with CSP than with HSP[23,24]. This may be explained as follows. First, electrocoagulation was not used with CSP; the resection area may have been inadequate; and residual lesions may have been present. Second, due to the lack of thermocoagulation marks after CSP, the lateral margins of the lesions were unclear, which affected histological evaluation of the specimens. In this study, the complete resection rate was 93.4% in the CSP group and 94.5% in the HSP group. The complete resection rate was high in both groups, and the difference was not significant. In the CSP group, the polyps were removed with the snare extended to normal tissues 1-3 mm away from the edge of the lesion, to ensure adequate margins, and to ensure no problems with histological evaluation of specimens (Figure 2). Some studies reported that the rate of incomplete resection was influenced by polyp size[22], and in this study the result was similar. However, morphological classification was seldom mentioned in previous studies. In this study, there were seven cases of incomplete resection with type IIa morphological classification in the CSP group, and the rate of incomplete resection was significantly higher than that of type IS and ISP. The residual tissue following CSP was in the lateral margins of the defect and not in the bottom margin, which was considered to be related to the morphological classification. The margin was that of a flat type IIa lesion, whose mucosa was similar to the peripheral boundary and was sometimes unclear. Suzukiet al[25] removed 145 lesions with CSP using linked color imaging (LCI), and the residual rate of tumor was 0.7%. They suggested that LCI easily identifies flat colorectal polyps. However, this remains to be confirmed. In recent years, with the development of CSP, some scholars think that CSP is inferior in obtaining submucosal tissue compared with HSP. Itoet al[26] reported that resection depth from muscularis mucosae in CSP versus hot-snare endoscopic mucosal resection was 76 μm versus 338 μm, and that resection of submucosa was achieved in 9% versus 92%, respectively. Shichijoet al[27] prospectively enrolled patients undergoing polypectomy for nonpedunculated polyps of 4-9 mm, and the overall incidence of incomplete mucosal layer resection was 63%. Thus, they concluded that CSP should be used for intraepithelial lesions only, and careful pretreatment evaluation is recommended. To improve the complete resection rate of CSP and improve the submucosal resection rate, some researchers have used submucosal injection before CSP (CSP-SI). Recently, some research on this has been carried out, but the conclusions showed clear differences. Some studies have shown that, compared with conventional CSP, CSP-SI has a significantly higher submucosal resection rate. However, a single-center prospective study by Shimodateet al[28] found that CSP-SI did not improve the resection depth of CSP for colorectal polyps < 10 mm, and the method resulted in lower rates of negative lateral and vertical margins of the resected lesions. Our research was limited to a comparison between conventional CSP and HSP (injection of saline according to the size of the lesion in the HSP group); thus, it was difficult to evaluate the effectiveness and safety of CSP-SI in our study. It has recently been reported that underwater CSP can obtain a higher complete resection rate and a sufficient deep resection compared with conventional CSP[29]. However, further data are required to confirm this. It has also been reported that improvement of the CSP snare may also be necessary to facilitate easy grasp of the lesions together with the submucosal layer[30].
In this study, CSP had an obvious advantage in terms of operating time compared with HSP. The specimen collection rates in the two groups were 98.1% and 98.6%, respectively. We suggest that the specimen collection rate had little to do with the resection method, and was mainly due to the size of the polyps and intestinal cleanliness.

Figure 2 Tissue specimen of cold snare polypectomy. A: Gross specimen of cold snare polypectomy (CSP); B: Cutting edge of CSP under high magnification.
There were some limitations to this study. First, it was a retrospective, single center study. Second, the follow-up data were insufficient. We attempted to obtain follow-up data from the enrolled population within 1 year after operation, but the sample size was too small to analyze. Third, the morphological classification included IS, ISP and IIa lesions, but none of the included patients had type IP polyps. At present, type IP polyps are mainly removed by HSP in our department. We look forward to applying CSP in these patients in future work, in order to better evaluate its safety and effectiveness.
CONCLUSlON
In conclusion, this study revealed that the rate of complete resection with CSP was similar to that with HSP, and CSP resulted in fewer adverse events compared with HSP. Thus, CSP is safe and effective for 4-9 mm colorectal polyps. CSP is worthy of further examination to determine whether it can improve the complete resection rate and resection depth in combination with other endoscopic techniques.
ARTlCLE HlGHLlGHTS


Research conclusions
In the treatment of sessile colorectal polyps < 10 mm, CSP has the same resection rate of impaired tissue integrity as HSP, but the delayed bleeding and perforation rate are lower in CSP group. CSP is a safe and effective method for polypectomy.
Research perspectives
This study retrospectively analyzed patients with colorectal polyps 4-9 mm in size treated by endoscopy in our hospital from January 2020 to December 2020. A comparison of HSP and CSP was carried including surgical outcome and safety.
FOOTNOTES
Author contributions:Meng QQ, Rao M and Gao PJ have all participated in the design of this study; Meng QQ and Gao PJ were responsible for analyzing and processing the data; Rao M collected the data in this study; Meng QQ wrote the manuscript, and Gao PJ made the final revision to the manuscript; all the authors have read and approved the final manuscript.
人与人之间呼吸道传播是结核病传染的主要方式。传染源是接触排菌的肺结核患者。随着环境污染和艾滋病的传播,结核病发病率越发强烈。除少数发病急促外,临床上多呈慢性过程。常有低热、乏力等全身症状和咳嗽、咯血等呼吸系统表现。
lnstitutional review board statement:The study was reviewed and approved by the Institutional Review Board of the First Hospital of Jilin University.
lnformed consent statement:All study participants, or their legal guardian, had provided verbal consent prior to study enrollment.
Conflict-of-interest statement:Meng QQ, Rao M, Gao PJ are employees of the First Hospital of Jilin University.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Qing-Qing Meng 0000-0002-1181-9666; Min Rao 0000-0001-8330-260X; Pu-Jun Gao 0000-0002-8306-7694.
S-Editor:Yan JP
L-Editor:A
P-Editor:Yan JP
 World Journal of Clinical Cases2022年19期
World Journal of Clinical Cases2022年19期
- World Journal of Clinical Cases的其它文章
- Current guidelines for Helicobacter pylori treatment in East Asia 2022: Differences among China, Japan, and South Korea
- Review of epidermal growth factor receptor-tyrosine kinase inhibitors administration to non-small-cell lung cancer patients undergoing hemodialysis
- Arteriovenous thrombotic events in a patient with advanced lung cancer following bevacizumab plus chemotherapy: A case report
- Endoscopic ultrasound radiofrequency ablation of pancreatic insulinoma in elderly patients: Three case reports
- Acute choroidal involvement in lupus nephritis: A case report and review of literature
- Choroidal thickening with serous retinal detachment in BRAF/MEK inhibitor-induced uveitis: A case report
