Advances in traditional Chinese medicine as adjuvant therapy for diabetic foot
Fa-Shun Liu, Yue Li, Xian-Shan Guo, Rui-Chen Liu, Hong-Ya Zhang, Zhen Li
Fa-Shun Liu, Yue Li, Zhen Li, Department of General Surgery, Yangpu Hospital, Tongji University School of Medicine, Shanghai 200090, China
Xian-Shan Guo, Department of Endocrinology, Xinxiang Central Hospital, Xinxiang 453000, Henan Province, China
Rui-Chen Liu, Binhai College, Nankai University, Tianjin 300450, China
Hong-Ya Zhang, Central Laboratory, Yangpu District Control and Prevention Center, Shanghai 200090, China
Abstract Diabetes mellitus (DM) is a complex disease that often causes multiple systemic complications that have become a major international public health problem. Diabetic foot (DF) is one of the severe and frequent chronic complications of DM due to vascular lesions and neuropathy. DF ulcers (DFU) affect approximately 15% of people with DM and are the leading cause of death and disability. The prevalence and recurrence of DF are worrisome, and morbidity and mortality are also on the rise, which poses a substantial socioeconomic burden. Treating DF is difficult for clinicians and requires multidisciplinary cooperation, combining local and systemic therapy to reduce amputation and case-fatality rates. Traditional Chinese Medicine (TCM) has received extensive attention due to noticeable therapeutic effects and few adverse reactions. In recent years, research on DF treatment by TCM has been increasing, and further progress has been made. TCM includes oral medication, injectable preparations, and adjuvant therapy. This article reviews the relevant research on TCM-related adjuvant therapy for DF. We describe current progress in TCM in terms of external application, acupuncture, massage, acupoint injection, foot bath, fumigation, and moxibustion, as well as the mechanisms involved.
Key Words: Diabetes Mellitus; Diabetic foot; Foot ulcers; Traditional Chinese medicine; Wound healing
lNTRODUCTlON
Diabetes mellitus (DM) is a complicated metabolic disorder caused by various pathogenic factors, and the main clinical feature is abnormally elevated blood glucose[1]. The American Diabetes Association divides diabetes into types 1 diabetes, type 2 diabetes, specific types of diabetes due to other causes, and gestational DM[2]. The prevalence of DM in virtually all world regions has increased significantly in recent decades. The estimated number of people with DM worldwide was 451 million in 2017. Approximately 1 in 11 adults has DM, and 90% of them have type 2 diabetes; that number is expected to increase to 693 million by 2045[3,4]. The main goal of therapy for type 2 diabetes is to prevent or delay complications and maintain quality of life[5]. There are many complications of DM, such as cardiovascular disorders[6], end-stage renal disease[7], retinopathy[8], neuropathy[9], mental illness[10], muscle atrophy[11], adhesive capsulitis[12] and even joint stiffness following surgery[13,14]. Diabetic foot (DF) is a frequent complication of DM due to vascular and neuropathological damage and is the main reason for amputation and death[15]. About 15% of people with DM suffer from DF ulcers (DFUs), and 14%-24% of those with DFU subsequently undergo lower limb amputation, which has led to DFU being the leading cause of non-traumatic lower limb amputations[16]. The 5-year mortality after amputation is 50%-59%[17], which is higher than the 5-year pooled mortality rate for cancer, which is 31.0%[18]. The global prevalence of DFUs is 6.3%, and in North America, this figure is 13.0%[19]. Moreover, DFU has a recurrence rate of 22.1% per person per year[20]. The direct cost of DM care in the USA in 2017 was US$237 billion, of which one-third was for lower extremity complications[18]. Healthcare expenditure for DF care is even more in the UK than for breast, prostate and lung cancer combined[21]. These data prove that DF has become a serious international medical and health problem. Therefore, understanding the pathogenesis of DF and developing targeted treatment is a major concern to clinicians.
DF is prone to ulceration and infection due to neuropathic edema and occlusive arterial disease[22]. DFU is caused by various factors, including peripheral neuropathy, foot deformity and trauma, and arterial disease[23]. In addition, DFU development was linked with a previous history of DFU and the male sex[24]. The precise mechanism of the delayed healing of DFU has not been fully elucidated. Wound healing is one of the most complex processes in the human body, mainly including four phases (hemostasis, inflammation, growth, re-epithelialization, and remodeling). Each stage has no recognizable boundaries and overlaps in time and space[25]. In DFU, however, extensive defects in the healing process result in ulcer healing delay and the occurrence of a highly pro-inflammatory chronic wound[26]. The major causes may be insufficient neovascularization, neuropathy, high probability of infection, tissue hypoxia[27], and nonphysiological inflammatory response[28]. They may also include an imbalance between metabolism and nutrient transport, abnormal cellular and gene expression, excessive formation of advanced glycation end products (AEGs)[29], and high concentrations of metalloproteases[30]. Pathologically, DFU has been found to decrease endothelial progenitor cell (EPC) recruitment due to reduced NO production[31]. Deficiency of cytokines such as vascular endothelial growth factor (VEGF), transforming growth factor (TGF)-β, keratinocyte growth factor (KGF), and platelet-derived growth factor (PDGF) are also associated with delayed DFU wound healing[29]. Furthermore, the dysfunction of the immune system in DM increases the rate of ulcer infection[32], and the frequency and severity of the infection are associated with delay and failure of the healing process[33].
Standard therapy of DFU includes decompression and ulcer protection, tissue perfusion repair, infection and metabolic control, local ulcer care, and education of patients and families[34]. TCM is the main form of ancient Asian medicine and an essential element of the Chinese health system[35], which is commonly used in clinical work in China[36]. It has accumulated a solid theoretical foundation in practice for thousands of years[37]. Chinese herbal medicine decoction is the essence of TCM, which has the characteristics of a multitarget, fewer side effects, and significant therapeutic effects[38]. With the advent of bioinformatics, the specific mechanism of TCM has been more scientifically explained[39]. Research on TCM for chronic non-communicable diseases has recently developed rapidly[40]. In particular, studies have reported that oral administration or injection of TCM herbal-based agents as an additional treatment to conventional therapies is beneficial to DFU healing[41,42]. Meanwhile, in recent years, complementary modalities have also demonstrated therapeutic potential. These methods include external application, acupuncture, massage, acupoint injection, foot bath, fumigation, and moxibustion. Therefore, a comprehensive search was conducted in the PubMed, Web of Science, and National Knowledge Infrastructure (CNKI) to investigate the value of TCM adjuvant therapy in DF. The electronic search was performed for articles published from inception to June 20, 2022. The search terms were used individually or combined: “Traditional Chinese Medicine,” “Diabetic foot,” “Diabetes Foot,” “Diabetic Patients with DF,” “Diabetes Feet,” “DF,” “External application,” ”Dressing,” “Acupuncture,” “Pharmacoacupuncture,” “Moxibustion,” “Massage,” “Acupressure,” “Knead,” “Acupoint injection,” “Acupuncture point injection,” “hydro-acupuncture,” “Foot bath,” “Lavipeditum,” “Soak,” “Medicated bath,” “Fumigation.” Reference lists of relevant articles were also hand searched. In addition, we made appropriate modifications according to actual requirements.
EXTERNAL APPLlCATON
Using plaster or compounds of TCM for external application is an efficient and straightforward treatment method. Compound Phellodendron liquid, which consists of Forsythia, Phellodendron, Honeysuckle, Dandelion, and Centipede, is one of the TCM for external application. Network pharmacology analysis shows that it contains 36 active ingredients related to DF. Functionally, the potential mechanisms of action are mainly related to inflammatory response and growth factor activity[43]. When DFU was treated with Compound Phellodendron liquid for four weeks, the ulcer area reduction, growth factor concentration, and total effective rate in the treatment group were higher than the standard nursing group[44]. Zhonget al[45] prepared a mixed ultramicro powder with Angelica, Calcined Gypsum, and Caleramide as raw materials, which promoted wound healing in DFU by accelerating wound closure and epithelialization, and inducing angiogenesis. Similarly, external application of the Chinese herbal medicine compound Tangzu Yuyang Ointment combined with standard wound treatment improved the rate of DFU healing. However, the healing time appeared to be prolonged[46].
In rats with DFU, Chinese medicine ulcer oi (Cortex Phellodendri and Angelica japonica as the main ingredients) upregulated the expression of VEGF and PDGF and downregulated protein tyrosine phosphatase 1B and AGEs in the wound tissue[47]. This indicated that Chinese medicine ulcer oil reduced local wound inflammation, promoted angiogenesis, and facilitated ulcer healing. Shixiang ointment promoted angiogenesis and accelerated ulcer healing by reducing AGEs and their receptors, activating nuclear factor kB p65, and upregulating VEGF, CD34, and endothelial NO synthase in the granulation tissue of DFU rats[48]. Wanet al[49] proved that San-huang-sheng-fu oil reduced cyclooxygenase-2 and upregulated VEGF and improved the decrease in plantar temperature and pain sensation in rats caused by the diabetic peripheral circulatory disorder. Similarly, another agent, Jing Wan Hong Ointment, elevated PDGF expression in a DFU murine model, enabling almost complete ulcer healingviaretarding inflammation and promoting cell proliferation and angiogenesis[50].
The common factors involved in the beneficial effects of external application of TCM in DF treatment rely on VEGF and PDGF to promote angiogenesis, cell proliferation, and inhibition of local inflammatory response.
ACUPUNCTURE
Acupuncture is essential to TCM and has been used for thousands of years against many disorders, including vascular diseases. There are many modalities of acupuncture, such as encircling needling, Bangci (focal center-side needling), auricular acupuncture, pestle needling therapy, and traditional acupuncture[51]. After auricular acupuncture treatment in type 2 DM patients, the blood flow of the lower extremities is improved, and the temperature of the soles of the feet increases, showing a preventive effect against DF[52]. Pestle needling therapy can decrease the foot vibration perception threshold and improve the sensory nerve function of the foot and the quality of life in high-risk DF[53].
Weiet al[54] compared the efficacy of encircling needling and Bangci (focal center-side needling) in wound healing of mice with DM. Both promoted skin wound healing by increasing local blood perfusion, and the therapeutic effect of encircling needling was better than Bangci. Mechanistically, acupuncture may reduce the protein levels of proinflammatory cytokines tumor necrosis factor (TNF)-α and interleukin (IL)-1β and increase neovascularization and fibroblasts in the wound[55]. These outcomes indicate that acupuncture can promote wound healing by reducing inflammation, promoting cell proliferation and angiogenesis, and inducing extracellular matrix remodeling.
Acupuncture benefits DF not only for its therapeutic effects but also demonstrates some preventive effects. It is important because reducing the incidence will significantly reduce the cost of DF treatment.
MOXlBUSTlON
The mechanism of moxibustion-based therapy is similar to that of acupuncture, and it has complementary therapeutic effects to acupuncture. It has been verified that the smoke and heat of moxibustion have a role in promoting wound healingviainhibiting the inflammatory response and promoting the formation of collagen fibers, granulation tissues, and capillaries[56]. The expression of TGF-β in wound tissue is significantly increased after moxibustion intervention, indicating the promotion of fibroblast proliferation and rapid formation of granulation in the early stage[57]. After six moxibustion interventions in a rat model, Kanet al[58] found that fibroblasts and collagen fibers in the wound tissue were more closely arranged, and neovascularization was richer. They demonstrated that moxibustion ended the inflammatory stage by regulating proinflammatory cytokines and initiated the repair stage in advance. Moreover, the content of VEGF and VEGF in the serum of rats after the intervention was significantly increased[59]. However, some studies have raised doubts. Alonsoet al[60] observed that acupuncture and moxibustion downregulated TGF-β1 and VEGF in adult female Wistar rats, but they still believed that moxibustion and acupuncture could stimulate fibroblast proliferation and neovascularization. Although many scholars have reported that moxibustion can promote wound healing, there is still no unified statement on its specific mechanism. Some scholars have even come to the opposite conclusion. Therefore, more basic and clinical research is needed to unveil the specific mechanism and justify the efficacy of moxibustion.
MASSAGE
Before the appearance of TCM decoction, ancient Chinese people started to use massage for disease prevention and treatment. Since massage needs to be administered at specific locations, when there are ulcers, massage will increase the pain and the risk of infection, so massage is mainly used for adjuvant treatment of diabetic peripheral neuropathy (DPN) and early DF. DPN is a significant risk factor for DF[61]. Nerve conduction studies are considered the gold standard in clinical research for DPN. Nerve conduction velocity (NCV) detects peripheral nerve conduction dysfunction caused by segmental demyelination and axonal damage and is usually slowed in DPN[62]. A recent meta-analysis of 3284 patients showed that TCM bath combined with acupoint massage improved the sensory and motor NCV and decreased neurological syndrome score in DPN[63].
Massage even improved the general condition of DM patients. Zarvasiet al[64] found that blood glucose significantly decreased and insulin levels increased after the self-acupressure intervention. After three years of acupressure treatment, the levels of total cholesterol, triglyceride, and low-density lipoprotein-cholesterol significantly decreased, and the level of high-density lipoprotein-cholesterol increased[65]. Massage appears to be beneficial not only for DF but also for the control of hyperlipidemia. It should be noted that since it is challenging to perform massage in animals, the specific mechanisms are hard to reveal.
ACUPOlNT lNJECTlON
Acupoint injection is a common treatment method in TCM. Either injection of Chinese herbal extracts (e.g., Danshen injection and Fufang Danggui injection) or conventional medicines (e.g., mecobalamin, vitamin B1, and anisodamine) at specific acupoints are available[66]. Applying electroacupuncture after methylcobalamin injection at Sanyinjiao (SP6) can restore ulnar and tibial nerve motor NCV and sensory NCV in patients with DPN[67]. A systematic review of 1071 Chinese DPN patients showed that acupoint injection of Chinese herbal extracts at Zusanli (ST36) was safe and may reduce pain and improve nerve afferent velocity compared with intramuscular injection of the same drug[66]. However, the trials included in this review were of low quality. Therefore, higher quality clinical trials are necessary to delineate the safety and efficacy of acupoint injection as adjuvant therapy for DF.
FOOT BATH
TCM foot bath using decoctions increases blood circulation for Grade 0 DF[68]. Additionally, herbal foot baths can improve local microcirculation and regulate skin permeability to increase drug absorption, thus effectively increasing drug concentration[69,70]. Recently, clinical trials have been designed to examine the efficacy and safety of TCM foot baths[68,71]. Nevertheless, foot baths can spread infection at the ulcer site in patients with chronic limb ulcers and increase the rate of toe loss (53%) and major amputation (30%)[72]. Consequently, the choice of foot bath treatment for DF needs to be carefully considered by clinicians due to its double-sided effect.
FUMlGATlON
Chinese herbal fumigation is a kind of external treatment of TCM, which can relax muscles and tendons and remove obstructions from meridians, activating blood to eliminate stagnation[73]. Cuyuxunxi prescription is a Chinese herbal fumigant widely applied to wash surgical wounds after anal fistulotomy, potentially promoting wound healing and antagonizing infection[74]. Zhuyuan decoction fumigation is an effective treatment to relieve the symptoms of patients with chronic sinusitis[75]. In addition, fumigation reduces knee osteoarthritis swelling and pain by inhibiting the expression of proinflammatory factors, promoting blood reflux, and reducing skin sensory nerve excitability[76]. Meanwhile, fumigation smoke and heat can promote wound healing in rats by inhibiting inflammatory responses and ameliorating the formation of collagen fibers, granulation tissue, and capillary status[56]. An ongoing systematic review will evaluate the effectiveness and safety of TCM fumigation in DPN[77]. Fumigation may be an effective therapeutic measure for DFU due to its anti-infective, inflammation-inhibiting, and wound-healing effects.
PROSPECTlVE
DF can be divided into neurologic, ischemic, or neuroischemic according to the International Working Group on the Diabetic Foot (IWGDF)[78] while The Society for Vascular Surgery Lower Extremity Threatened Limb (SVS WIfI) classification system classifies DF into four grades: Grade 0, 1, 2, and 3 (Table 1)[79]. For grade 2 or 3 DF, amputation and hemodynamic reconstruction are often required. Therefore, TCM adjuvant therapy is mainly used for grades 0 and 1 DF. As shown in Figure 1, for grade 0 or 1 DF caused by neuropathy (usually DPN), foot bath, acupoint injection, and massage are optional treatment modalities because they can accelerate the sensory and motor NCV in the lower limbs. External application, moxibustion, fumigation, acupuncture, massage, and foot bath can increase blood flow in the lower extremities and promote neovascularization in the local wound for ischemic grade 0-1 DF. For neuroischemic grade 0 or 1 DF, massage, footbath, or a combination of other adjunctive therapies, can be chosen. For all DF (including grades 2 and 3), massage is an optional adjunctive therapy that regulates local and systemic metabolism (including blood glucose and lipids). In addition, topical application, moxibustion, and acupuncture can promote wound healing in grade 1 DF, and fumigation may be an effective anti-infection modality when local infection occurs. In conclusion, selecting appropriate TCM adjunctive therapy for early DF(grades 0 and 1) will positively affect patients, but it should be noted that foot baths may lead to skin maceration and increase the rate of amputation.
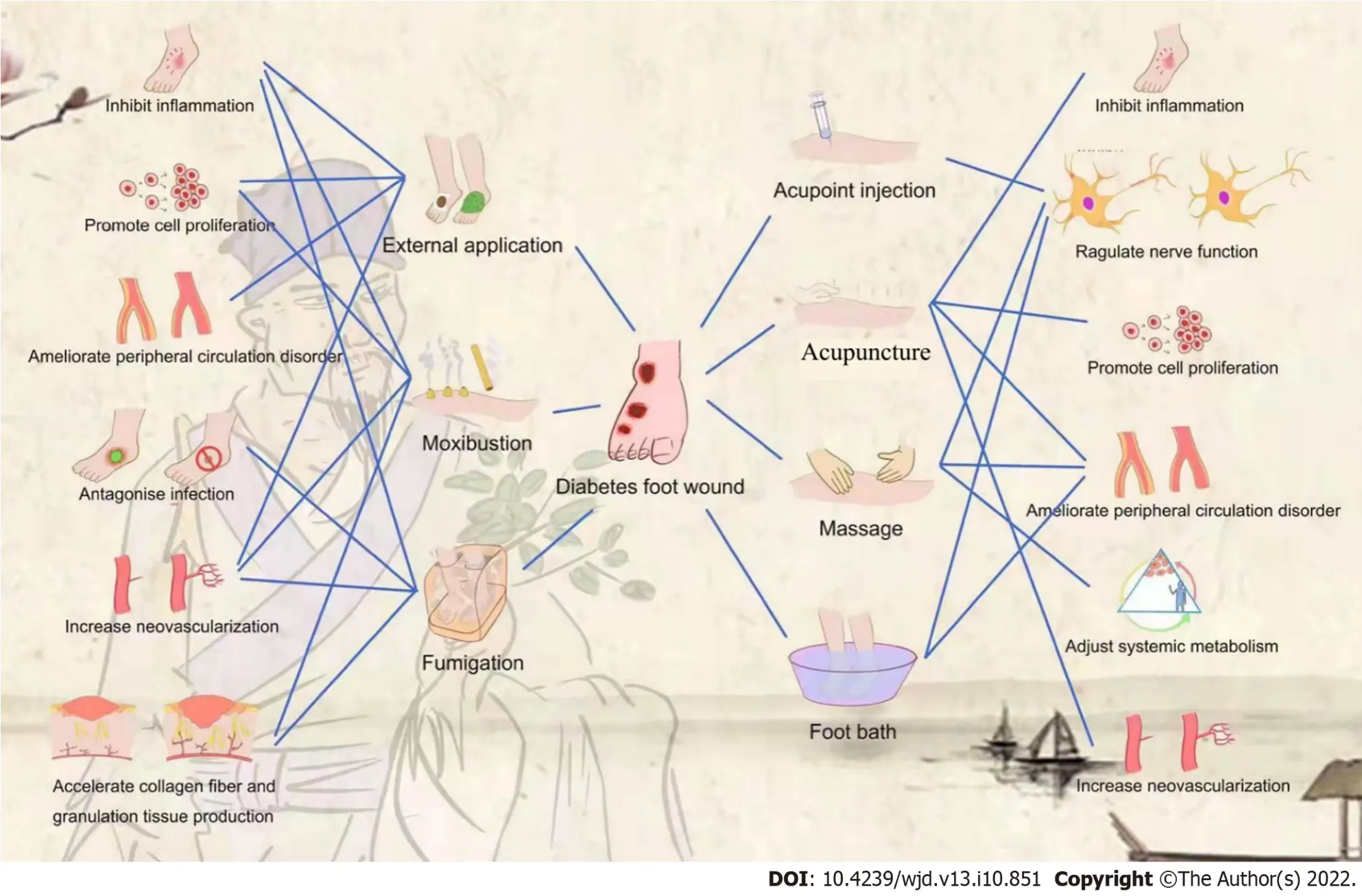
Figure 1 Categories of traditional Chinese medicine as adjuvant therapy for diabetic foot wound and related mechanisms.

Table 1 Society for Vascular Surgery Lower Extremity Threatened Limb (SVS Wlfl) classification system
Chinese herbal medicine treatment is distinguished by its multi-target and multi-level nature. With the application of network pharmacology to the study of TCM herbal formulations in recent years, the active constituents of herbal medications and their unique targets of action have been discovered, providing a theoretical foundation for their clinical use[80]. Future studies may focus on new wound dressings utilizing medicinal plant extracts or their purified active components[81]. Nonetheless, we must not overlook the fact that the precise mechanism of action of TCM requires additional investigation. In addition, there is no research on the effectiveness of TCM in preventing DF. “Treating the untreated” has been a critical area of concern for TCM, and scientific randomized controlled trials (RCTs) can be used to confirm its risk-benefit ratio in the prevention of DF is also necessary.
CONCLUSlON
DF is a common complication of diabetes. There are many adjunctive therapies in TCM that can be applied to DF. Some have been proven effective, while others require more research. Animal experiments have confirmed that TCM adjuvant therapy can promote DFU wounding healing by inhibiting nonphysiological inflammationviadown-regulating AGEs, RAGE, TNF-α, and IL-1β, promoting neovascularizationviaup-regulating VEGF and PDGF, inducing extracellular matrix remodeling, improving local blood circulation, and accelerating the production of collagen fibers and granulation tissue. In the future, more high-quality research is needed to demonstrate and popularize the application of TCM adjuvant therapy in DF.
ACKNOWLEDGEMENTS
We thank the Fudan University Committee of the Communist Youth League for the guidance of diagram.
FOOTNOTES
Author contributions:Liu FS wrote the paper; Li Y, Guo XS, and Liu RC performed the collected the data; Li Z reviewed the article; all authors have read and approved the final version.
Conflict-of-interest statement:Authors declare no conflict of interests for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Fa-Shun Liu 0000-0002-6825-9559; Yue Li 0000-0002-7447-3957; Xian-Shan Guo 0000-0003-1288-4061; Rui-Chen Liu 0000-0003-1046-4098; Hong-Ya Zhang 0000-0002-8046-0829; Zhen Li 0000-0002-6147-7545.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YX
 World Journal of Diabetes2022年10期
World Journal of Diabetes2022年10期
- World Journal of Diabetes的其它文章
- Growing importance of urogenital candidiasis in individuals with diabetes: A narrative review
- Considerations for management of patients with diabetes mellitus and acute COVlD-19
- Everything real about unreal artificial intelligence in diabetic retinopathy and in ocular pathologies
- New therapeutic approaches for type 1 diabetes: Disease-modifying therapies
- Correlation between gut microbiota and glucagon-like peptide-1 in patients with gestational diabetes mellitus
- Effectiveness and safety of human umbilical cord-mesenchymal stem cells for treating type 2 diabetes mellitus
