Potent Anti-bacteria Activity of Tamsulosin Hydrochloride and Ningmitai Capsule in Combination by Regulating the Gene Expression Related to β-Lactamase, Hemolysis, and Virulence
CHENG Sha , SUN Bao-Fei, YU Jia , HUANG Li-Rong , LUO Heng *
(1)State Key Laboratory of Functions and Applications of Medicinal Plants, Guizhou Medical University, Guiyang 550014, China;2)Key Laboratory of Chemistry for Natural Products of Guizhou Province and Chinese Academyof Sciences, Guiyang 550014, China;3)Department of Pharmaceutical Engineering, College of Food and Pharmaceutical Engineering, Guizhou Instituteof Technology, Guiyang 550003, China;4)Department of Anatomy, School of Basic Medical Sciences,Guizhou Medical University, Guiyang 550014, China)
Abstract Tamsulosin hydrochloride (TSH) is a selective α1 adrenergic receptor antagonist used in the treatment of symptomatic benign prostatic hyperplasia (sBPH). Ningmitai capsule (NMT) is a traditional Chinese medicine preparation produced on the basis of traditional Chinese herbs formula. NMT is mainly used for treating stranguria caused by damp and hot accumulate knot, dripping wet acerbity pain and bloody urine, lower urinary tract infection and chronic prostatitis. It has been confirmed that TSH can be used in combination with many drugs to treat microbial infections and resistance to antibiotics, which displayed better therapeutic effect and application prospect. NMT also has obvious antibacterial and bactericidal effects on many pathogenic bacteria such as Escherichia coli, Proteus, Neisseria gonorrhoeae, Streptococcus faecalis, Staphylococcus aureus and so on. It is suggested that the combined application of these two drugs may have significant antibacterial activity against clinical bacteria. Therefore, anti-bacterial activities of combination of TSH and NMT were tested in vitro by turbidimetric assays. We found that combination use of TSH and NMT showed significant selectivity which displayed stronger inhibitory activities against the three strains than that of the application of single drug in vitro; The infective animal models were used to test the antibacterial activity of TSH combined with NMT in vivo. The results showed a potent effect (P < 0.01) of combination use of two drugs on the treatment of pneumonic sepsis mouse infected with K. pneumonia and a significant effect (P < 0.05) on the mouse infecting with B. subtilis, while the treatment had no obvious effects on the mouse infecting with S. aureus. And their antibacterial mechanisms were assessed by quantitation of the expression of functional genes in vitro using RT-PCR in response to infection by Klebsiella pneumonia (K. pneumonia), Staphylococcus aureus (S. aureus) and Bacillus subtilis (B. subtilis). The results suggest that the antibacterial mechanism of two drugs in combination might be attributed to the regulation of β-lactamase associated genes (including GES, VEB, PER-2 and IMP) in K. pneumonia, hemolysis associated genes (yhdP, yhdT, yqhB and yugS) in B. subtilis and key virulence genes (saeR, hla, sbi and mecA) in S. aureus. Taken together, these data suggested that combined use of TSH and NMT exhibited remarkable bactericidal effects in vitro to three strains through regulating the expression of β-lactamase, hemolysis and virulence associated genes at transcription level; The drug combination elicited better effects in the mouse model infecting with K. pneumonia and B. subtilis in vivo. Hence, the combination treatment of TSH and NMT may possess potential prophylactic or therapeutic effect against bacterial infections.
Key words Tamsulosin hydrochloride; Ningmitai; drug combination; gene expression
Microbial infections are still among the leading causes of death in the world primarily due to multidrug resistance (MDR) of pathogenic bacteria[1].On the research front, it is generally recognized that major efforts are urgently needed to discover new antimicrobial molecules[2], or even better, alternative therapeutic approaches. In order to treat severe mixed infection, expand antibacterial spectrum, and reduce adverse reactions, more and more drug combinations were applied as treatment for many diseases in clinical therapies.
Tamsulosin hydrochloride (TSH) is a selective α1a adrenergic receptor antagonist used in the treatment of symptomatic benign prostatic hyperplasia (sBPH). The treatment of TSH usually led to the relaxation of smooth muscle in prostate gland and therefore reduced the resistance to urinary flow[3]. At present, it has been confirmed that TSH can be combined with many drugs to treat microbial infections and resistance to antibiotics, which displayed better therapeutic effect and application prospect[4-6]. Ningmitai capsule (NMT), produced by Guiyang XinTian Pharmaceutical Co., Ltd., China, is a formula preparation established according to the theory of traditional Chinese medicine. It consists ofRadixetcortexBerberidisSargentianae,PolygonumcapitatumBuch.-Ham.exD.Don,KadsuraPepperStem,FoliumHibisciMutabilis,RhizomaImperatae,HerbaAgrimoniaeandFructusForsythiae. Ningmitai capsule (0.38 g) contains more than 1.0 mg gallic acid, detected by HPLC in Chinese Pharmacopoeia published in 2015. Previous clinical studies showed that NMT had effects of eliminating damp-heat, removing toxin, improving micturition and dysuria[7]. NMT is mainly used for treating stranguria caused by damp and hot accumulate knot, dripping wet acerbity pain and bloody urine, lower urinary tract infection and chronic prostatitis. It also possessed obvious bacteriostatic and bactericidal effects againstEscherichiacoli,BacillusProteus,Neisseriagonorrhoeae,Streptococcusfaecalis,Staphylococcusaureusand many other pathogenic bacteria[8]. It was suggested that combination of these two drugs may have significant anti-bacterial activity for clinic bacteria.
Although TSH has been investigated for its ability to eradicate biofilms produced by medical devices infected by bacteria[9-10], its application especially in combination with other approaches, has not yet been fully investigated. In this study, an innovative treatment approach to eradicate infections caused by such antibiotic-resistant and biofilm-producing bacteria was proposed. The treatment combines TSH with NMT therapy to achieve an additive or synergistic therapeutic effect. This study focused on the anti-bacterial activity of two drugs in combination, and then discussed their molecular mechanism of action, which may provide a scientific basis for reasonable drug combination.
1 Materials and Methods
1.1 General
Varian Inova-400 spectrometer (USA) was employed to record the nuclear magnetic resonance (NMR) spectra with tetramethylsilane as an internal standard, and mass spectroscopy (MS) studies were carried out on a HP1100-MSD spectrometer (ESIMS mode) (USA). TSH was obtained from the Guizhou provincial people’s hospital. NMT were provided from Guiyang XinTian Pharmaceutical Co., Ltd., China. Chemicals used in all the experiments performed during the study were of the analytical reagent grade (AR). Organic solvents (spectroscopically pure from Sigma, USA) used in chemical synthesis included ethyl alcohol, diethyl ether and dimethylformamide (DMF). Deionization of water was done entirely in glass equipments and normally used in all preparations. Luria-Bertani (LB) broth growth media was purchased from Oxoid (Basingstoke, UK); ampicillin, streptomycin, kanamycin and Chloramphenicol were obtained from Sigma;E.coliATCC 25922,S.aureusATCC 25923,B.subtilisATCC 6051,A.baumanniiATCC BAA-1710 D,K.pneumoniaATCC BAA-1705 andP.aeruginosaATCC 39324 were obtained from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China). Other reagents were of analytical reagent quality.
1.2 Antibacterial activity assay in vitro
Anti-bacterial activities of test drugs were assessedinvitroby turbidimetric assaysinvitro[11]. Test drugs were prepared in 0.1 mol/L DMSO and diluted with LB, the final concentration of DMSO was maintained at ≤1% (V/V). The bacteria were seeded at a concentration of 1 × 105CFU/mL in 96-well microculture plates (90 μL/well) containing LB; then solutions of prepared drugs were added to each well to obtain a final concentration of 50 μg/L. Thereafter, the microplates were vigorously shaken on a vibrating platform for 20 hours at 37℃. Further, the plates were then examined in an ELISA plate reader at 450 nm for absorbance to determine the growth inhibitory activity[9]. Results were expressed as mean values of the three independent variables.
The minimum bactericidal concentration (MBC) values were measured by broth microdilution method in the 96-well microculture plates[12]. The bacteria were seeded in 96-well microculture plates at the concentration of 1×105CFU/mL in LB, in a series of different concentrations of tested drugs and incubated for 20 hours at 37℃. The minimum inhibitory concentration was the lowest concentration in which absorbance by ELISA was parallel to the control in three independent experiments.
1.3 Infection of mice, survival and bacterial burden
Three test bacteria were grown to log phase in LB medium at 37℃.50 mL of bacterial solution was collected by centrifugation, washed three times with PBS and resuspended in 500 μL PBS for use. After the mice were anesthetized by ether inhalation, the suspensions of Klebsiella pneumoniae, Staphylococcus aureus, and Bacillus subtilis were injected into the nostrils of the mice, inhaled naturally, and the mice lay down until they woke up. The inoculation doses of Klebsiella pneumoniae, Staphylococcus aureus and Bacillus subtilis were all 30 μL (4×108CFU/mL). Allin-vivoexperiments were performed using 6-8 weeks old BALB/c mice on same background obtained from experimental animal research center (Shanghai, China), and bred in the animal facility of Guizhou Medical University. The infected mouse model was built as described[13-14]. All mouse in every experiment were randomly divided into four groups (every group included 10 mouse) including bacterial infected group, TSH- bacterial infected group, NMT- bacterial infected group, TSH and NMT - bacterial infected group. The dose of the drug is 3 mg/ kg body weight. Mice survival rates were computed and plotted according to the nonparametric Kaplan- Meier analysis. Animal care is in accordance with the guidelines of the Guizhou Medical University and China Council of Animal Care.
1.4 In vitro gene expression
Bacteria (2×107) were resuspended in LB containing 50 μg/L of drugs (TSH 50 μg/L, NMT50 μg/L, TSH 50 μg/L+NMT50 μg/L) or in LB alone. Samples were incubated at 37℃ for 20 hours, and RNA was harvested and subjected to TaqMan real-time reverse transcriptase polymerase chain reaction (RT-PCR), as described previously[11-12]. The relative quantification of genes was determined by changes in expression of transcription relative to the expression in untreated bacteria. Samples were normalized to the housekeeping gyrase subunit B (gyrB, a ubiquitous gene encoding the B subunit protein of DNA gyrase in bacteria) gene ofS.aureusand 16 S ribosomal RNA (16 s RNA, a component of the small subunit of a prokaryotic ribosome) ofK.pneumoniaorB.subtilis[12]. Data were expressed as change at transcription level after treatment with the screened drugs. The sequences of the primers used for analysis are listed in Table 1.
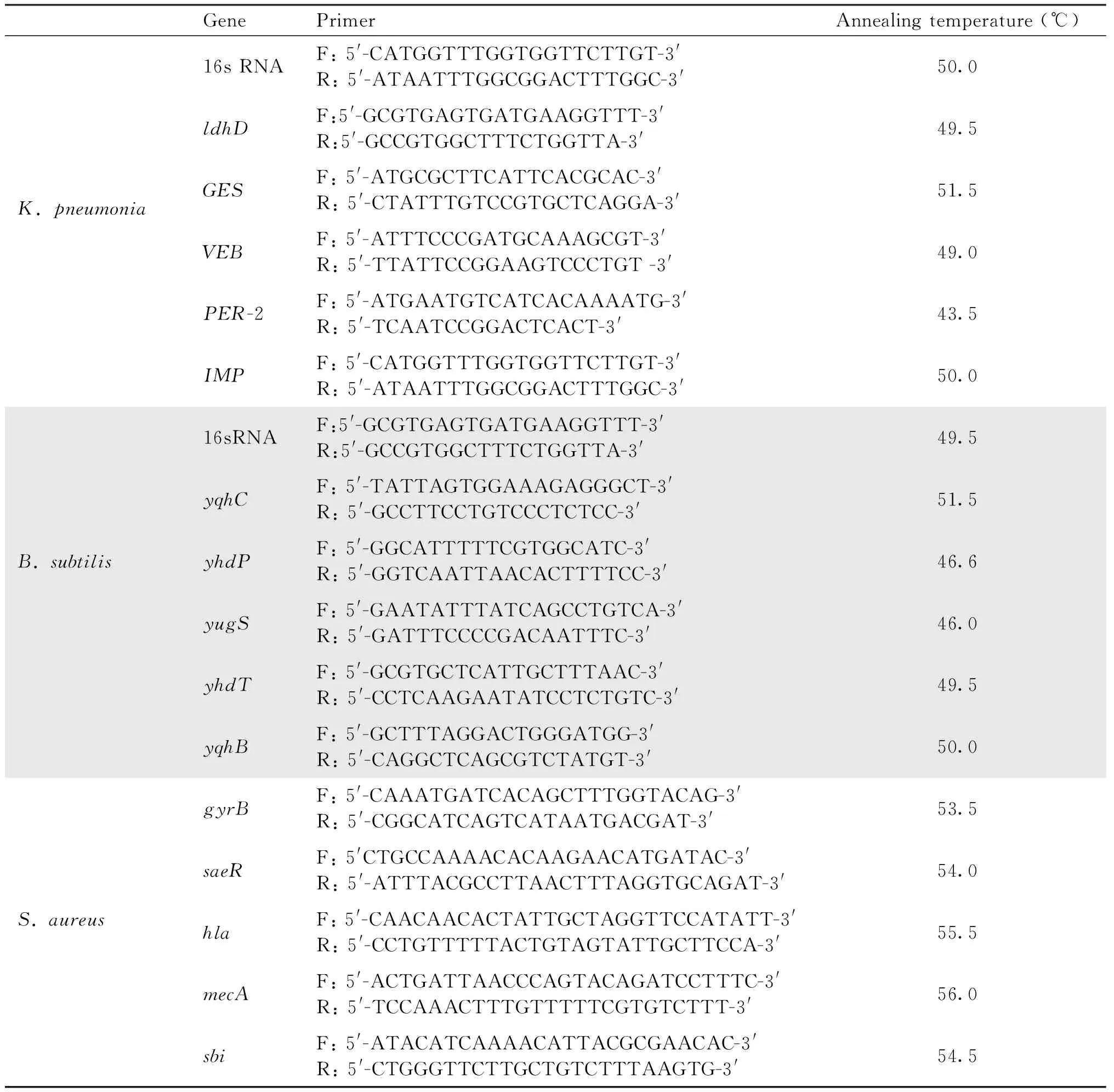
Table 1 List of the primers used in this study
1.5 Statistical analysis
TheIC50value was calculated from the semi-logarithmic dose-response curves. The data were analyzed using SPSS 18.0 and reported as mean ±SDof the number of experiments indicated. For all the measurements, one-way ANOVA followed by a Student’st-test was used to assess the statistical significance of difference between each group. LSD method is used to assess the statistical significance of difference between every two group. A statistically significant difference was considered at the level ofP< 0.05. Dates were presented as the mean ±SEMof three independent assays.
2 Results
2.1 Antibacterial activity of TSH and NMT in combined application
The anti-growth activities of 50 μg/L TSH, 50 μg/L NMT and their balanced mix were assayed for preliminarily evaluating the antibacterial activities. The results were summarized in Fig. 1 and Table 2. Results showed that TSH and NMT given individually exhibited slight antibacterial activity againstK.pneumonia,S.aureusandB.subtilis. However, the two drugs in combination displayed stronger inhibitory activities against the three strains. Especially forK.pneumonia, drug combination possessed similar antibacterial effect to that of control, and stronger than that of independent treatment of each drug (P< 0.01). Furthermore, MBC values need to be evaluated for both drugs and their combination according to their inhibitory concentration curves.
To determine if the two drugs and their combination demonstrated antibacterial activities at different

Fig.1 Inhibitory effects of NMT, TSH and their combination on the growth of three bacteria in vitro Drugs were added into 96-well microculture plates containing the bacteria at concentration of 105 CFU/mL in Luria Broth. The plates were measured in an ELISA plate reader at 450 nm after cultures shaken on a vibrating platform at 37℃ for 8 hours. The concentration of drugs was 50 μg/L. Data were obtained from three independent experiments, same as the below results

Table 2 Antibacterial activities of TSH, NMT and their combination against three strains
concentrations, the bacteria were incubated in LB containing varied concentrations of drugs for 8 h at 37℃ with shaking. The optical density at 450 nm was measured after 8 h to evaluate inhibitory activities and to determine MBC values of two drugs and their combination. MBC values of each treatment for each bacterium were defined as the lowest concentration of drugs that reduced growth by causing 1% reduction of the inoculum control as normal strains[8-11]. The inhibitory concentration curves (Fig. 2) and MBC values (Table 3) clearly showed that two drugs and their combination inhibited the growth of three bacteria as a concentration- dependent manner. Expectedly, inhibitory activities of the two drugs in combination againstK.pneumonia(Fig. 2A),S.aureus(Fig. 2B) andB.subtilis(Fig. 2C) showed stronger activity than that of single use of each drug at different concentrations, which demonstrated that the two drugs in combination can enhance antibacterial activity forK.pneumonia,S.aureusandB.subtilis. In addition, no significant difference in MBC values forK.pneumonia(P< 0.01) was observed between drug combination and the control, which indicated that the two drugs in combination exhibited as powerful ability against the growth ofK.pneumoniaas that of empirical clinical medication ampicillin. Likewise, drug combination showed close inhibitory activity forB.subtilis(P< 0.05) comparing with streptomycin.

Fig.2 The inhibitory concentration curves of the screened drugs against three strains in vitro Different concentration of tested drugs was added to 96-well microculture plates containing the (A) K. pneumonia ATCC BAA-1705, (B) B. subtilis strain ATCC 6051 and (C) S. aureus strain ATCC 25923 at concentration of 105 CFU/mL in Luria Broth, respectively. The plates were measured in an ELISA plate reader at 450 nm after cultures shaken on a vibrating platform at 37℃ for 8 hours. The inhibition ratio (%) was calculated by the equation of the turbidimetry test in methods
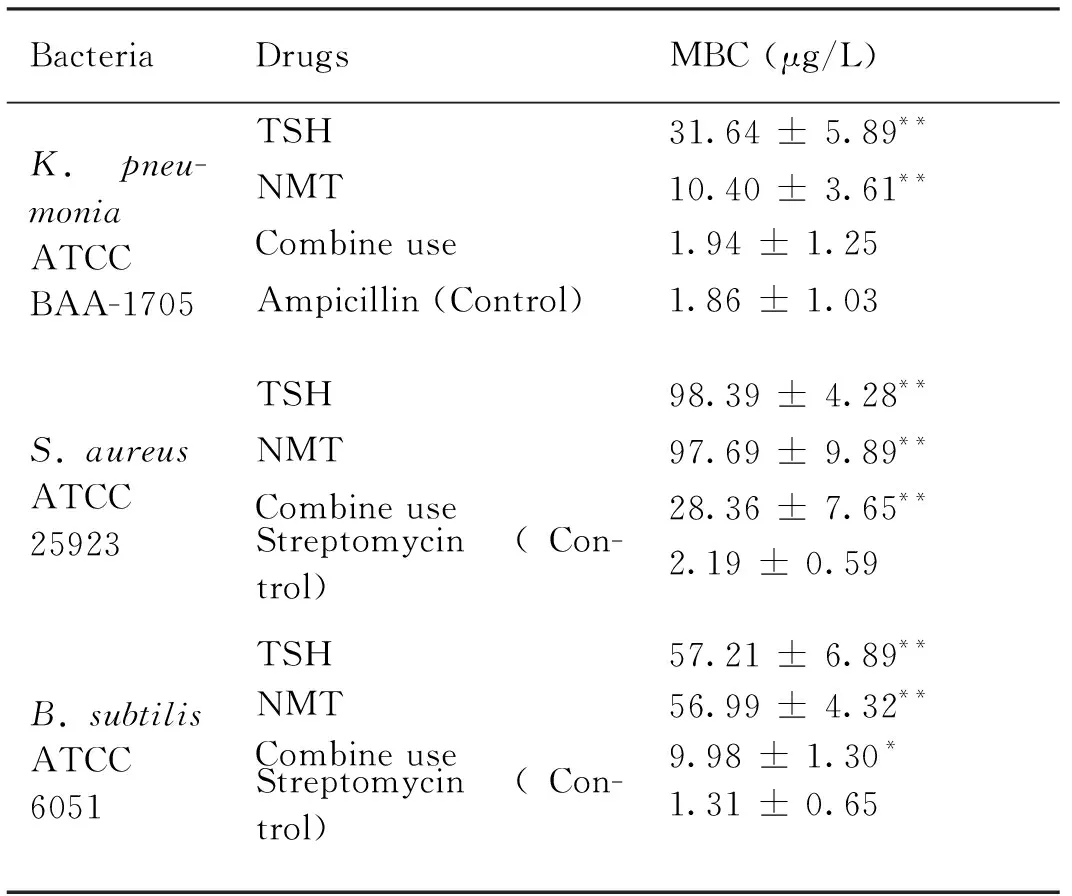
Table 3 MBC values of the drugs against three strains in vitro
2.2 Antibacterial activity of TSH and NMT combined application in vivo
The anti-growth activities of 3 mg/kg TSH, 3 mg/kg NMT and their balanced mix were assayed for preliminarily evaluating the treatment effects using the bacterial infected miceinvivo. The results were summarized in Fig. 3. Results showed that both of TSH and NMT exhibited slight therapeutic effect respectively for the mice infected withK.pneumonia,S.aureusandB.subtilis. However, the two drugs in combination displayed stronger therapeutic effect for the mice that infected with theK.pneumoniaandB.subtilis. Especially forK.pneumonia, drug combination possessed similar antibacterial effect to that of control, and stronger than that of independent treatment of each drug (P< 0.01). However, there was no obvious effect for the mice infected withS.aureus. Those results indicated that TSH and NMT in combination had a better therapeutic effect to the infected mice withK.pneumoniaandS.aureus, which suggested that two drug combination is a novel therapeutic method for some infected diseases.
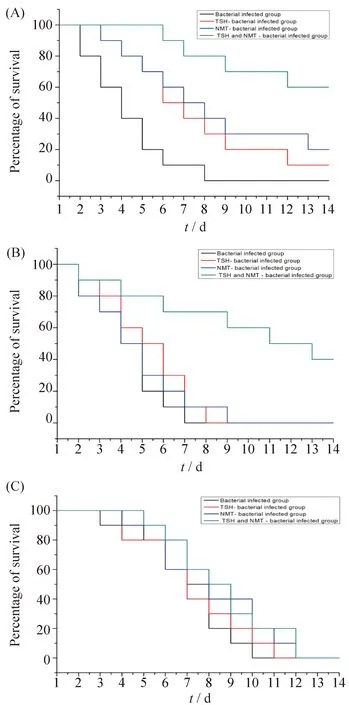
Fig.3 The therapeutic effect of the screened drugs to the mice infected with three strains in vivo Three test bacteria (A) K. pneumonia ATCC BAA-1705, (B) B. subtilis strain ATCC 6051 and (C) S. aureus strain ATCC 25923 were grown to log phase in LB medium at 37℃. All in-vivo experiments were performed using 6-8 weeks old BALB/c mice on the same background. All mouse in every experiment were randomly divided into four groups (every group included 10 mouse) including bacterial infected group, TSH-bacterial infected group, NMT-bacterial infected group, TSH and NMT-bacterial infected group. The dose of the drug was 3 mg/ kg body weight. Mice survival rates were computed and plotted according to the nonparametric Kaplan-Meier analysis
2.3 Effect of the drugs on the expression of metabolism related genes in K. pneumonia
The mechanism by which these drugs synergistically inhibited the growth ofK.pneumoniawas determined by measuring the expression of metabolism associated genesGES,VEB,PER-2,IMPandldhD, using the housekeeping gene 16sRNAas control[15](Fig.4). Two experiments of RT-PCR (Fig. 4A) and semi-quantitative RT-PCR (using the agarose gel, Fig. 4B) were applied for determining the expression level of above genes.

Fig.4 The screened drugs altered the expression of K. pneumonia related gene in vitro (A) Fold change of four metabolism genes was analyzed by real-time PCR. (B) The expression of four genes was assayed by semi-quantitative RT-PCR. The 2×107K. pneumonia was incubated with the 25 μg/L drugs for 8 hours. Data are normalized to the transcript abundance of 16s 004RNA gene, and fold change was relative to K. pneumonia incubated in medium alone (time matched).*P < 0.05 and ** P < 0.01 compared with the control, respectively. Data were obtained from three independent experiments, same as the below results
Our results showed that TSH significantly (P< 0.01) promoted the expression of three ESBL-related genes, while NMT exhibited a significant (P< 0.01) promotion for the expression ofPER-2 but no obvious effect on the expression ofGESorVEB. However, TSH combined with NMT displayed significant (P< 0.01) inhibitory effects against the expression ofGES, and significant (P< 0.01) promotive effects for the expression ofPER-2. In addition, TSH combined with NMT significantly (P< 0.01) inhibited the expression ofIMP. However, the results showed that the two drugs and their combination displayed no obvious inhibition or promotion for the expression ofldhD.
2.4 Effect of drugs on the expression of hemolysis-associated genes in B. Subtilis
Expression levels ofyhdT,yqhB,yugS,yhdPandyqhCgenes in test strains treated with TSH, NMT and their combination were determined using housekeeping gene 16 s RNA as control (Fig. 5) by RT-PCR (Fig. 5A) and semi-quantitative RT-PCR methods (Fig. 5B). Results showed that the expression ofyqhBwas significantly (P< 0.01) up-regulated under the treatment of TSH, NMT and their combination; expression levels ofyhdT,yugSandyhdPwere significantly (P< 0.01) down-regulated under the treatment of combination of NMT and TSH; single treatment of NMT significantly inhibited the expression ofyhdT(P< 0.01) andyugS(P< 0.05). However, significant expression ofyqhCwas not observed for both drugs and their combination.
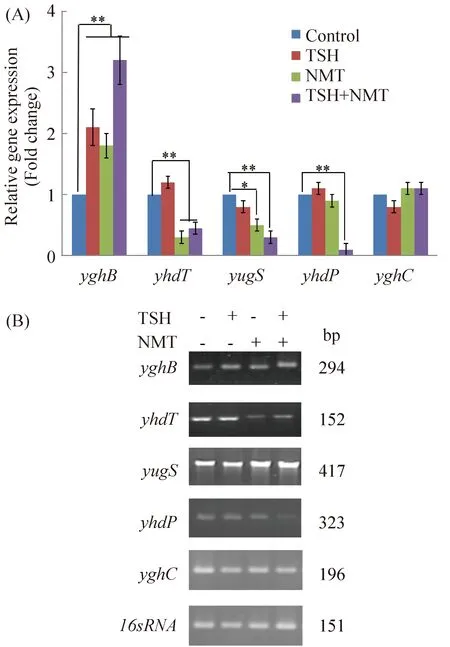
Fig.5 The screened drugs altered the expression of B. subtilis hemolysis- associated gene in vitro (A) Fold change of five hemolysis genes was analyzed by real-time RT-PCR. (B)The expression at transcription level of five genes was assayed using semi-quantitative RT-PCR. The 2×107 B. subtilis was incubated with 25 μg/L drugs for 8 hours. Data are normalized to the transcript abundance of 16sRNA gene, and fold change was relative to B. subtilis incubated in medium alone (time matched). *P < 0.05 and ** P < 0.01 compared with the control, respectively. Data were obtained from three independent experiments, same as the below results
2.5 Effect of the drugs on the expression of virulence genes in S. Aureus
To determine if the two drugs and their combination exhibited any influence on the expression of virulence factor, we incubatedS.aureusATCC 25923 with a sublethal dose of the drugs (25 μg/L) and measured transcript abundance of keyS.aureusvirulence factorssaeR,hla,sbiandmecAat 8 h post exposure, using RT-PCR (Fig. 6A) and semi-quantitative RT-PCR methods (Fig. 6B) withgyrBhousekeeping gene as control. The results showed that there was a significant enhancement (P< 0.01) in the inhibitory effect against the expression ofsaeRunder the treatment with TSH combined with NMT.

Fig.6 The screened drugs altered the expression of S. aureus virulence genes in vitro (A) Fold change of four virulence genes was analyzed by real-time RT-PCR. (B) The expression at transcription level of four genes was assayed using semi-quantitative RT-PCR. The 2×107S. aureus was incubated with 25 μg/L drugs for 8 hours. Data were normalized to the transcript abundance of gyrB gene, and fold change was relative to S. aureus incubated in medium alone (time matched). *P < 0.05 and ** P < 0.01 compared with the control, respectively. Data were obtained from three independent experiments, same as the below results
3 Discussion
Antibacterial activity assay showed that TSH and NMT exhibited slight antibacterial activities againstK.pneumonia,S.aureusandB.subtilis. However, the two drugs in combination displayed stronger inhibitory activities against the three strains in a concentration-dependent manner, especially forK.pneumonia. TSH is a selective α1 receptor antagonist, and NMT is a Chinese medicine formula with relative antibacterial effect for lower urinary tract infection. The main pathogens of urinary tract infection are Klebsiella spp and some Enterococcus and Staphylococcus spp. The literature shows that α1 receptor blockers can significantly increase the drug concentration, prolong the half-life and the concentration time, and reduce the clearance rate of antibacterial drugs, and synergistically produce a strong antibacterial effect[4-6]. Therefore, it is speculated that TSH cooperates with NMT to have stronger antibacterial effect on Klebsiella pneumoniae, followed by antibacterial effect onStaphylococcusaureusandBacillussubtilis.
Extended-spectrumβ-lactamase (ESBL), producingE.coliandK.pneumonia, described in the early 1980 s have now rapidly spread through worldwide and posed serious threat for health care-associated (HA) infection[15-16]. Most of these ESBLs are derivatives of restricted-spectrum TEM- and SHV-typeβ-lactamases, with one or more amino acid substitutions surrounding their active sites, thus explaining the extension of their hydrolysis profile[15]. Plasmid-located ESBL genes are mostly found inK.pneumoniaeand also in other Enterobacteriaceae species and have been recently described inPseudomonasaeruginosa[15, 17]. Our results clearly demonstrated that combination of these two drugs inhibited the growth of bacteria through up- or down-regulation of ESBL-related genesGESorPER-2 and interfering with genes involved inβ-lactamases biological regulation pathway. Indeed, the profile of antimicrobial resistance conferred byGEScorresponded to those observed with structurally unrelated ESBLs, rather as a ceftazidime-hydrolyzing enzyme as opposed to the recently describedVEB[15, 18]. The carbapenem-resistant geneIMP, belongs to Ambler class B metallo-β-lactamases (MBLs), has a broad substrate profile and often confers high-level resistance to allβ-lactams except aztreonam. In modern time, the clinical utility of these antimicrobials is under threat with the emergence of acquired genes for carbapenemases, particularly those coding for MBLs, now have been reported in Asia[19], Europe[20, 21], North America[22], and South America[23]. Unlike class A β-lactamases, MBLs are not inhibited by clavulanic acid, tazobactam, or sulbactam. However, they are susceptible to ion chelator EDTA because of their zinc dependence. Acquired MBLs have now been detected in a range of organisms, includingPseudomonasaeruginosa[20],Acinetobacterspecies[24]andK.pneumonia[25], but rarely has hospital infection outbreak been described in which multiple gram-negative genera are involved[26]. Our results of the expression detection ofIMPindicated that the drug combination inhibited the growth of bacteria probably through up- or down-regulation of MBLs-related genesIMPand further confirmed by interfering with the genes involved in theβ-lactamases biological regulation pathway. D-lactic acid dehydrogenase (ldhD), is a key enzyme for the synthesis of D-lactic acid. The ldhD enzyme transforms pyruvic acid to produce lactic acid by biochemical reactions with NADH as coenzyme; oppositely, the enzyme can catalyze adverse reaction under the presence of coenzyme NAD+. However, the results showed that the two drugs and their combination displayed no obvious inhibitory or promotive action for the expression ofldhDgene.
The pathogenicity of bacteria was closely related with hemolysis vitality as haemolysin is an important virulence factor of pathopoiesis[27, 28]. With wide application ofB.subtilisand its increasingly osculating relationship with the production and living of people, therefore, the threat to the human health will also increase. The whole genome sequence ofB.subtilishas been completed, and the hemolysis associated genes from the genome annotation includedyqhC,yhdP,yhdT,yqhB,yugSandytjA[29]. Except thatytjAwas identified as hemolysis gene ofB.subtilis[30], the function of other several genes has not been identified. We assayed the changes of expression level ofyhdT,yqhB,yugS,yhdPandyqhCgenes and the results suggested that hemolysis genes were closely involved in the anti-growth process with the treatment of combination of NMT and TSH inB.subtilis.
Transcript abundance ofsaeRgene, a regulatory gene component of global virulence regulatory system SaeR/S, which plays an essential role in the development of staphylococcal skin lesions in mice[31], was down-regulated about 2-fold incubated with combination of the two drugs versus incubation with control inS.aureus.hla, encoding α-toxin, is a virulence factor responsible for dermonecrosis in mouse skin infections[32]. The transcript expression ofhlagene was down-regulated by the combination of NMT and TSH (P< 0.01).mecAencodes an altered penicillin-binding protein 2a to confer resistance toβ-lactam antibiotic[33]. The expression at transcription level was down-regulated more than 1-fold by treating with TSH combined with NMT compared with that in controls. In addition, the expression ofsbigene was analyzed using same methods.sbiencodes an immunomodulatory protein which is important in antibody and complement evasion[33]. The expression at transcription level was markedly up-regulated by TSH or NMT (P< 0.05), and was significantly up-regulated by treating with TSH combined with NMT (P< 0.01). The changes of expression at transcription level of virulence genes inS.aureus, including the SaeR/S virulence regulatory system, suggested that NMT combined with TSH may differentially regulate an even larger number ofS.aureusvirulence genes, which may support the hypothesis that the anti-growth activity of NMT combined with TSH toS.aureusmay correlate with the up- or down-regulation of the expression of virulence genes.
The combination of TSH and NMT has a strong antibacterial effect. Since NMT is a traditional Chinese medicine formulation with many ingredients, there is a logical causal relationship between the antibacterial activity of TSH and NMT combined with the up-regulation and down-regulation of the above multiple genes, which needs further research to confirm.

