Hair follicle-targeting drug delivery strategies for the management of hair follicle-associated disorders
aInstitute of Pharmaceutics,College of Pharmaceutical Sciences,Zhejiang University,Hangzhou 310058,China
bZhejiang Huanling Pharmaceutical Technology Company,Jinhua 321000,China
cThe Third People’s Hospital of Hangzhou,Hangzhou 310009,China
dJiangsu Engineering Research Center for New-type External and Transdermal Preparations,Changzhou 213149,China
Keywords:Follicular drug delivery Androgenetic alopecia Acne vulgaris Nanotechnology Microneedles
ABSTRACT The hair follicle is not only a critical penetration route in percutaneous absorption but also has been recognized to be a target for hair follicle-associated disorders,such as androgenetic alopecia (AGA) and acne vulgaris.Hair follicle-targeting drug delivery systems allow for controlled drug release and enhance therapeutic efficacy with minimal side effects,exerting a promising method for the management of hair follicle-associated dysfunctions.Therefore,they have obtained much attention in several fields of research in recent years.This review gives an overview of potential follicle-targeting drug delivery formulations currently applied based on the particularities of the hair follicles,including a comprehensive assessment of their preclinical and clinical performance.
1.Introduction
The stratum corneum (SC) and hair follicle delivery routes are the most crucial pathways allowing transdermal drugs to penetrate the skin [1].Improving the bioavailability of transdermal medicine has been an urgent pharmaceutical challenge,as non-permeable corneocytes occupy large areas of skin [2,3].Under physiological conditions,the intact SC significantly prevents large hydrophilic substances and particulate structures from skin penetration.In contrast,the presence of hair follicles provides a way to pass through this barrier.Below the skin surface,hair follicles located deep into the dermis offer a large surface area for the prospective absorption of drugs or substances.The hair follicles function as reservoirs and portals for dermally applied substances[4,5].Over the past several years,hair follicle-targeting drug delivery has become a very appealing strategy for treating hair follicle-related disorders,including androgen-associated diseases,hair loss[6,7],and acne vulgaris[8].The importance of follicular delivery systems reflects in promoting the topical treatment efficiency of such diseases and reducing systemic side effects.Several studies have demonstrated the advantages of the transfollicular route on porcine ear skin[9,10].Additionally,particles-containing formulations could be detected within the hair follicles even after 10 days,while nanoparticles in the SC reservoir stored for only one day,indicating that hair follicles can function as a promising tool for sustained drug release[11].
Various hair follicular diseases probably result from the follicles’ complex cycle and structure.Hair loss and acne vulgaris are probably the most common disorders closely related to hair follicles,as hair follicles on the face and scalp occupy as much as 10% of entire hair follicles[12].In such cases,hair follicle-targeting drug delivery is becoming an essential element of different therapies.Androgenetic alopecia (AGA),as a common form of alopecia,is a multifactorial and age-related chronic disease and seriously affects patients’psychology as well as the quality of life [13].Nearly 80% and 50% of Caucasian men and women are reported to experience some degree of AGA by the age of 70 years [14].Conventional medical treatment consists of topical minoxidil and oral finasteride (FIN) formulations to stimulate hair regrowth.However,the existing treatment regimens for AGA are not able to adequately deliver drugs directly to the hair follicles,resulting in the emergence of systemic side effects [15,16] and a lack of efficacy [6].Acne vulgaris is a common skin dysfunction of pilosebaceous units(PSU) [17] and is related to excessive sebum production,follicular keratinization,immunological changes,and bacterial proliferation in the hair follicles.Topical retinoids,including adapalene,tazarotene,and tretinoin,have been approved by the US Food and Drug Administration to manage acne vulgaris [18].However,common adverse effects such as skin irritation and discomfort may affect the tolerability of topical therapies [19].Furthermore,hair follicles are partly or wholly occluded by excessive keratin and dead cells in the early stage of acne vulgaris [20],further aggravating the development of the disease.Thus,it is critical to create an effective and safe follicular drug delivery system for the topical treatment of AGA and acne vulgaris.
The preferential deposition of drugs in hair follicles is determined by the physicochemical properties of the drug itself and the type of carrier applied in the formulations.Many drug delivery systems,including polymeric nanoparticles(NPs),lipid nanoparticles,and microneedles,have been broadly investigated to enhance the specific delivery of active pharmaceutical ingredients to hair follicles.This review’s major goal is to critically introduce and analyze hair follicletargeting delivery systems,thereby providing a reference for more advanced and safer formulations to cure follicular disorders.
2.Features of the hair follicle
2.1.The structure and barrier of the hair follicle
Previous studies have proven that hair follicles play a vital role in topical drug delivery as a trans-appendage pathway and trans-epidermal route [21].The complex three-dimensional structure of the hair follicle and cyclical activity must be considered when designing follicular drug delivery systems.As Fig.1Ⅰshows,the permanent part of the hair follicle includes the infundibulum,isthmus,and bulge region from top to bottom [22].The infundibulum at the upper part of the hair follicle is covered by an impermeable and intact SC.In contrast,the permeability dramatically increases in the lower infundibulum as the epidermis differentiates into a trichilemmal pattern,which is readily accessible for transdermal compounds [23].The inner root sheath surrounding the hair follicle canal is related to the shape of the hair.Furthermore,the outer root sheath plays a regulatory role through interactions with melanocytes.The representative character of the hair follicle is its cyclical growth (Fig.1Ⅱ),which undergoes the anagen,catagen,and telogen phases and then re-enters the anagen phase[24].The bulge containing the hair follicle stem cells (HFSCs) in the outer root sheath plays a crucial role in regulating the hair cycle [25].Furthermore,the upper hair follicles are surrounded by plenty of immune cells,such as dendritic cells and Langerhans cells,indicating that hair follicle targeting might be a meaningful tool for transcutaneous immunization [26].Notably,the sebaceous glands provide extra target sites that have drawn therapeutic interest for conditions like AGA,acne vulgaris,and other sebaceous gland disorders[27].
2.2.The mechanism of hair follicle-targeting drug delivery
The penetration through the hair follicle route is a complex process resulting from the hair follicle’s complex structure,and the exact mechanism has not been clearly understood[23].Generally,the transepidermal transport reduces once the drug is encapsulated in particulate carriers because particles tend to penetrate and preferentially deposit in the orifices of hair follicles (Fig.2Ⅰ;[29]).The process of hair follicle delivery is affected by many factors involving the physicochemical characteristics of drug molecules,such as the oil-water partition coefficient,molecular size,molecular weight,etc.,and carriers,such as particle size,lipophilicity,surface charge,etc.[30-32].
As shown in Fig.2Ⅱ,previous studies have underscored the strong effect of “particle size” on the depth and extent of follicular delivery systems [33,34].Thus,appropriately sized carriers play a critical role in the penetration of different skin layers and target sites within the hair follicle.Furthermore,keratin cells can function as a pumping system,and they can transmit carriers mechanically into the hair follicles along with hair movement [35].The hair movement potentiates the follicular penetration of nanoparticles with the mean diameter between the thickness of keratin cells and the diameter of hair follicles.The optimal size of particles was found to be in the range of 400 -700 nm to penetrate deeply into the hair follicle.In contrast,smaller particles mainly reached the deeper skin layers,and larger particles primarily remained on the skin’s surface [36].Earlier studies have demonstrated that smaller nanoparticles(20 nm) had a quicker accumulation in hair follicles during a time-dependent process (Fig.2Ⅲ),while these smaller nanoparticles are more likely to reach the lower layer of skin in the end.In summary,smaller substances exhibit a tendency to penetrate the skin through the transfollicular pathway into the living tissues surrounding the hair follicles,but the particles with optimal size tend to accumulate preferentially within the hair follicles[37].It is crucial to perform customized designs by controlling the particle size according to the medication positioning requirements.Moreover,dissolving microneedles could penetrate the skin and release their loaded therapeutics directly into dermal layers to enrich hair follicles [29],thereby making them a potential choice for targeting the hair follicles.
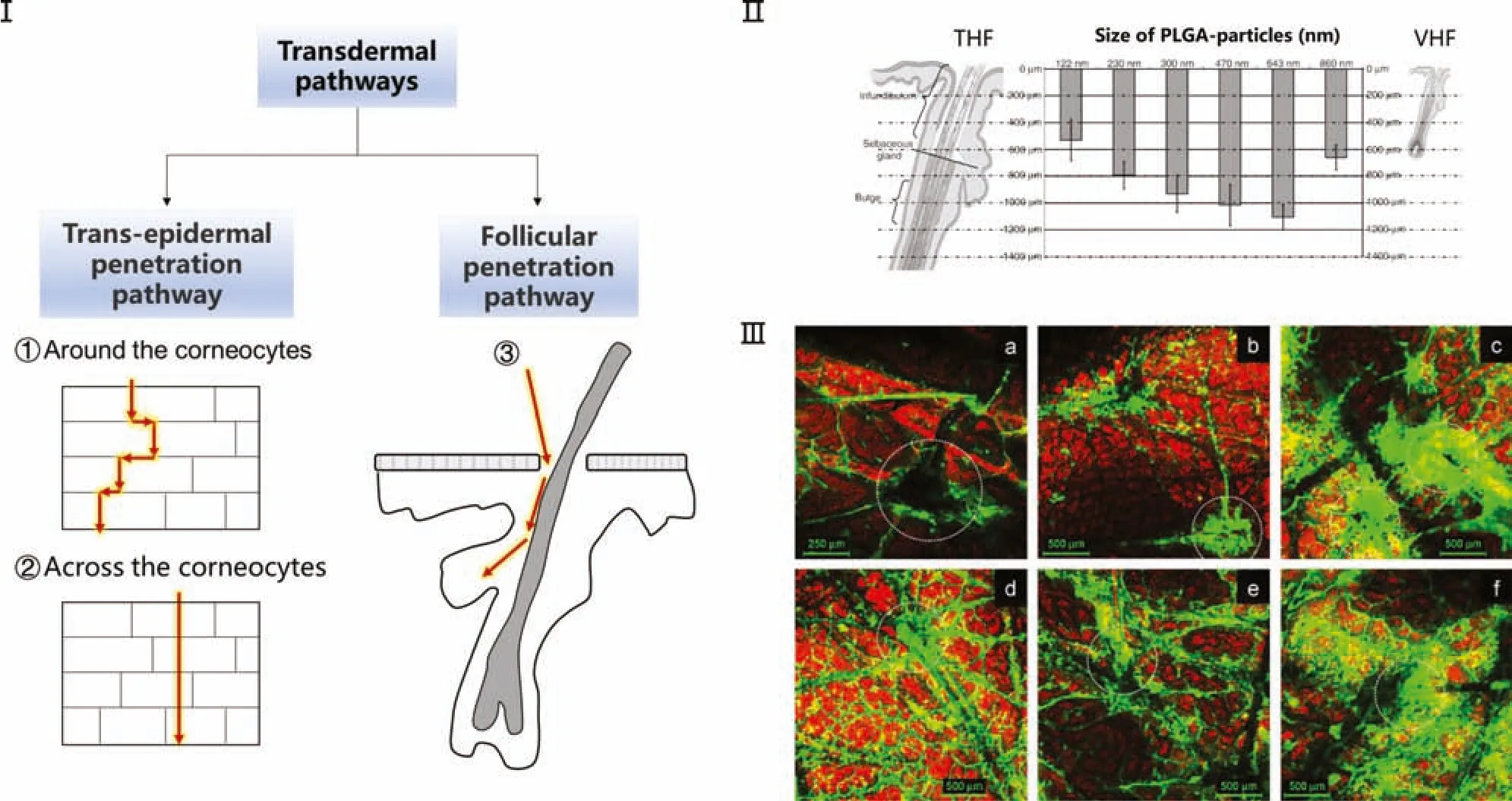
Fig.2-Mechanism and factors of the follicular penetration process.Ⅰ.Illustration for the penetration route of transdermal drug delivery system.Penetration pathways of transdermal drug:(1)Trans-epidermal penetration pathway around the corneocytes;(2)Trans-epidermal penetration pathway across the corneocytes;(3)Follicular penetration pathway.Particles tend to penetrate and preferentially deposit in the orifices of hair follicles.Ⅱ.The size effects of PLGA nanoparticles on penetration depths associated with the target sites in terminal hair follicles(THF)and vellus hair follicles(VHF).[40] Ⅲ.x-y images showing the nanoparticle accumulation in hair follicles after applying nanoparticles(20 nm,200 nm)for(a,d)30 min,(b,e)1 h,and(c,f)2 h.The circles in white represent hair follicles.[41]
Furthermore,the influence of NPs’ surface charge on hair follicle targeting was extensively studied but remains unclear.Interestingly,there are conflicting findings among different studies.A recent study proved that hair follicles could abundantly accumulate NPs with negative surface charge and lipophilic surface features.Negatively charged poly(D,L-lactide-co-glycolide)(PLGA)nanoparticles and PLGA nanoparticles coated with phospholipids facilitated follicular uptake on a pig ear skin model [38].However,another study[39]indicated nanostructured lipid carriers(NLCs)containing cationic surfactants exhibited higher follicle accumulation.
3.Strategies for hair follicle targeting
Hair follicles can efficiently bypass complex intercellular permeation pathways and enter deeper skin layers,which makes the hair follicles become an exciting target site.Given the complexity of follicular penetration,three different strategies taking advantage of the hair follicle targeting have been applied and schematically illustrated in Fig.3.Nanotechnology-based particles are utilized to deliver therapeutic substances into the pre-determined target sites of the hair follicle.Moreover,microneedles can break the skin barrier and deliver the therapeutic substances directly to the sites around the hair follicle,achieving accurate and fast mapping.Or nanoparticles equipped with a specific release mechanism are applied to deeply deliver medicinal substances into the hair follicle,where exogenous stimulations accelerate drugs’active release.

Fig 3-Scheme of current strategies for hair follicle targeting.Ⅰ.Nanotechnology-based particles are utilized to deliver therapeutic substances into the hair follicle.Ⅱ.Microneedles are utilized to deliver the therapeutic substances directly to the sites around the hair follicle.Ⅲ.Exogenous stimulations lead to an active release of the drugs from the particles equipped with specific release mechanisms.
3.1.Nanotechnology-based formulations for follicular drug delivery
Current strategies for follicular drug delivery mainly focus on using nanostructured drug delivery systems,such as polymeric nanoparticles,nanoemulsions,lipid nanoparticles,and metallic nanoparticles.An overview of NPs related to hair follicle delivery is shown in Table 1.Various types of NPs possess individual characteristic behaviors and different physicochemical characteristics regarding skin and follicular penetration.Though the exact mechanism of hair follicle targeting by nanoformulations is unclear,particle size is a determinant for targeting delivery and retention in hair follicles.Besides,the occlusive effect is also an important factor in the process of nanoparticles entering into hair follicles[42].Nanosized particles can guarantee close contact with superficial junctions of the SC.After the evaporation of water,the hydrated SC will enlarge the space between the keratinocytes,thereby enhancing the drug transport to hair follicles [43].The general merits of nanoparticle local drug delivery systems can be summarized as follows: enhanced physical and chemical stability,increased drug accumulation,better solubility,and sustained release of drugs [44,45].Though hair follicles account for less than 0.1% of the total skin area [46],the penetration of follicular drugs obtained through nanotechnology-based formulations improves by creating particles of small size to enlarge the surfaces with the SC.Particularly,drug-loaded nanoparticles access and accumulate preferentially in the orifices of hair follicles,which function as drug reservoirs for controlled drug diffusion that can reduce the doses and frequencies to overcome side effects of therapy.
3.1.1.Polymeric nanoparticles
Polymeric nanoparticles are solid particles in the nanometer range,prepared using biodegradable and biocompatible polymers or monomers,such as chitosan,cellulose,polystyrene,PLA,PLGA,polyvinylalcohol,and polyethyleneimine [87].NPs with a diameter between 1 nm and 1000 nm are more likely to reach their target organs or tissues through various barriers in the body.A previous study[88] traced the fate of NPs in the skin by incorporating Nile red into the NPs and demonstrating efficient drug delivery to hair follicles (Fig.4Ⅰ).Although NPs themselves can’t pass through the skin barrier completely,they can be entrapped deeply within the hair follicle.Additionally,the high surface area to volume ratio enhances the contact between particles and target cells.NPs systems penetrate preferentially into the follicle in a time-dependent manner;meanwhile optimal size NPs exhibit higher follicular accumulation [41].Thus,polymer-based synthetic nanotechnology-based formulations have gained growing interest since the last decade as a follicular drug delivery treatment.
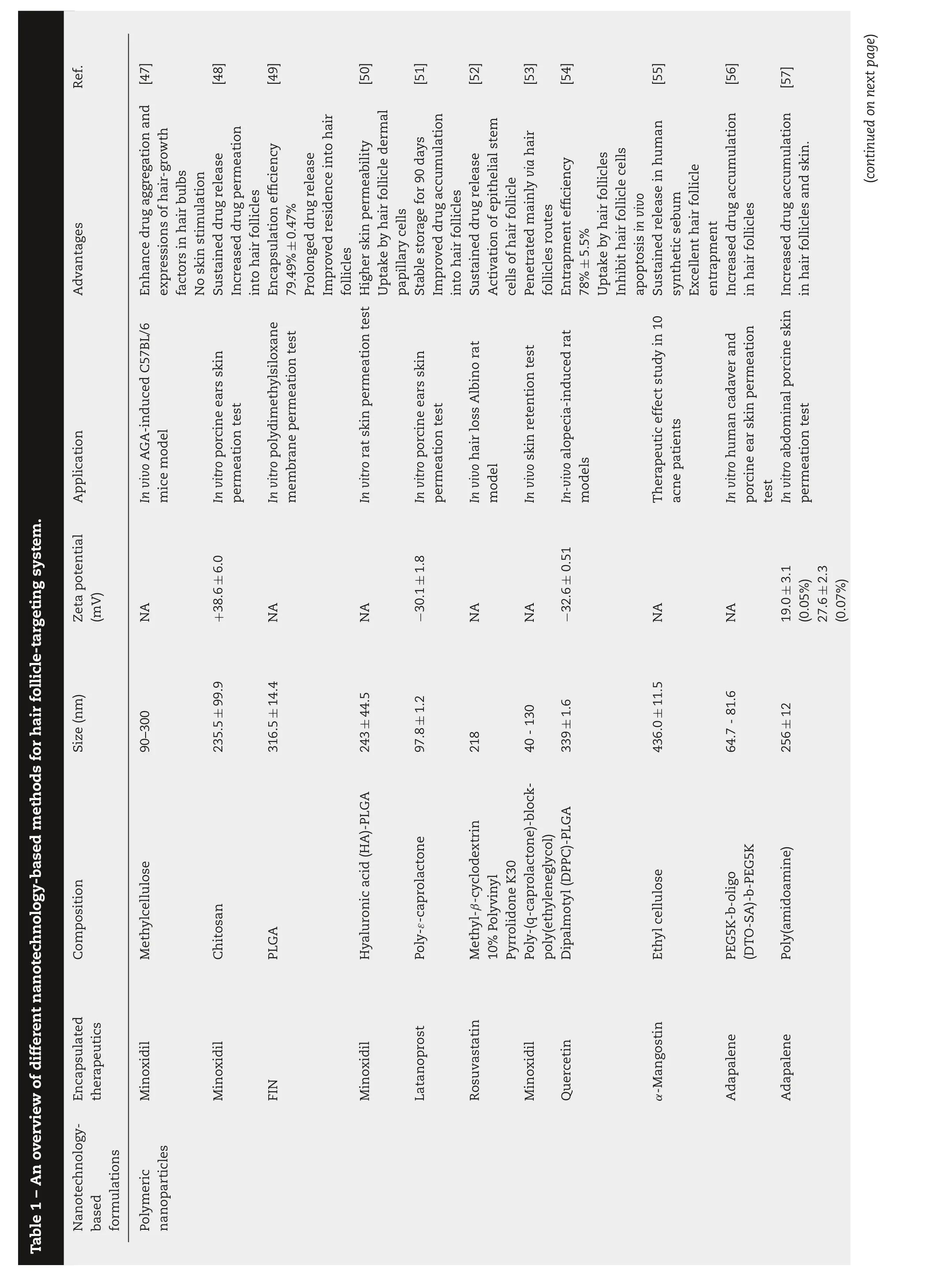




Fig.4-Application of polymer nanoparticles in hair follicle-targeting drug release system and for the treatment of hair loss.Ⅰ.Nile red/ROX-loaded nanoparticles for hair follicle targeting after 1 h of incubation time.[88] Ⅱ.Fluorescence microphotographs of rat skin incubating with RhB labeled HA-PLGA NP for 4,6,8,and 12 h.Scale bar=100 μm.[50]Ⅲ.Cyanoacrylate surface biopsies of(A)Nile red labeled TyroSpheres and(B)Nile red solution treated porcine ear skin.[56] Ⅳ.Confocal laser scanning microscope(CLSM)images of abdominal porcine skin deposited(a)FITC-labeled Polyamidoamine dendrimers and(b)free FITC solution for 8 h.[57]V(A)The x-y CLSM images of porcine skin treated with(a)Nile Red solution,(b)Nile Red-loaded polymeric micelles,and(c)x-z image of porcine skin treated with Nile Red loaded polymeric micelles.Scale bar=50 μm.(B)The CLSM images at depths of(a)14 μm,(b)150 μm,and(c)400 μm of Nile Red loaded polymeric micelles deposited porcine skin.Scale bar=100 μm.[65]
Though topical minoxidil is generally well tolerated,the efficacy of drug treatments remains low [89].The low effectiveness is likely due to low absorption: about 1.4%of topically applied minoxidil can be absorbed through a normal intact scalp [90].Minoxidil-encapsulated HA-PLGA NPs [50] have reportedly delivered drugs directly into hair follicles with time-dependent increase (Fig.4Ⅱ).At 4 h,most of the fluorescence was measured in the SC and epidermis,which meant that Rhodamine B (RhB)-HA-PLGA NPs were more likely to remain only on the skin surface.After 6 h,the total fluorescence of follicle cells increased while the SC decreased.Adapalene,the first-line treatment for acne vulgaris,belongs to a third-generation retinoid with the effects of prostration,keratinization,and antilipid secretion.Unfortunately,adapalene’s physicochemical properties(logP=8.04,pKa=4.23)limit its topical application in the skin and hair follicles.“Retinoid reactions” are the most common adverse effects of topical adapalene therapy,including erythema,burning feeling,and scaling in dosedependent.To overcome these limitations,Ramezanli et al.[56] developed biocompatible self-assembled nanoparticles(TyroSpheres)for follicular drug delivery of adapalene.In vivocyanoacrylate follicular biopsies test exhibited the effective release of fluorescent dye-labeled TyroSpheres within the hair follicle (Fig.4Ⅲ).The accumulation of adapalene was 51.5±10.8 and 33.0±11.8 μg/mm2respectively in hair follicles as a result of TyroSpheres and Differin®,indicating that the TyroSphere could significantly increase the drug deposition to the PSU.Besides,the partition coefficient values of the drug in sebum/water(Ksebum)and SC/water(Ksc)were calculated to be 39.5±7.1 and 18.6±1.5,respectively.These results suggest that TyroSpheres have been transported through PSU.Furthermore,the location of drug carriers is vital in hair follicle-associated disorders treatment.Studies demonstrated that nanoparticles accumulated in the follicles rather than penetrated into the deeper layers of the skin (Fig.4Ⅳ).For example,Pluronic® F127 micelles in nanoscale could be transmitted at the maximum 400 μm of hair follicles (Fig.4V),indicating they did not pass through the intact SC but selectively localized in skin structures.
3.1.2.Lipid nanoparticles
Lipid nanoparticles include solid lipid nanoparticles (SLNs)and NLCs,which are considered as suitable drug delivery systems due to their biocompatibility,degradability,and low toxicity.SLNs with a size of 40-1000 nm are lipid-based nanoparticles formed only from solid lipids.NLCs were designed to overcome some potential shortcomings of SLNs and exhibit a higher loading capacity and long-term stability[91].Hair follicles have been confirmed to be a potential pathway for NLCs penetration resulting from the lipophilic property of the follicular ducts (Fig.5Ⅰ).Moreover,a previous study has revealed that free fatty acids used to prepare SLNs and NLCs can function as efficient 5α-reductase inhibitors and stimulate hair growth[75].
The application of SLNs and NLCs to AGA therapy has been extensively investigated because they are able to pass through the skin through the hair follicle route.Lipid nanoparticles with smaller size and occlusive properties can attach themselves to the skin surface,promoting adhesiveness,increasing hydration,and maintaining sustained release stably in the following phase.Moreover,the nanoparticle size appears to be a vital factor affecting the penetration depth and speed of substances through the skin.The previous study has found that SLNs below 100 nm can aggregate into deep layers of skin mainlyviahair follicle pathways [92].Wang et al.[71]prepared minoxidil-encapsulated NLCs with oleic acid as the liquid lipid and stearic acid as the solid lipid.Compared to the minoxidil-loaded SLNs,minoxidil-NLCs showed better storage stability and 10.7-folds higher drug retention in the skin.NLCs broadly promoted the drug deposition in the follicles,which may be due to the fusion with sebum or the opening of inactive follicles.
Not only NLCs alone,but the combinations of NLCs and functional substances also represent a novel delivery strategy and aim to have synergistic effects in promoting hair growth.Aljuffali et al.[73] used anti-platelet-derived growth factor(PDGF)-conjugated NLCs to achieve active targeting of specific cells,which could precisely deliver the drug to follicles and dermal papilla cells (DPCs).The encapsulated minoxidil was largely deposited in the follicles (Fig.5Ⅱ) and penetrated into the DPCs,thereby accelerating cell proliferation and upregulating the expression of angiogenesis-related factors.In vivoskin permeation analysis demonstrated that anti-PDGF-NLCs could increase the accumulation of minoxidil in follicles by three-fold compared to the solution group.Furthermore,chitosan is considered a highly favorable material and possesses excellent biocompatibility and nontoxicity properties.Positively charged chitosan may be beneficial for skin and hair delivery,as it would be attracted to negatively charged skin and hair.And it has been proved that NPs with chitosan facilitated the hair follicle targeting delivery compared to nanoparticles without chitosan.Besides,Lauric acid itself has been proven to have a remarkable inhibitory effect on both type I and type II 5αreductase activity compared to other fatty acids,possessing significant antiandrogen activity.A recent report from Noor et al.[75] prepared lauric acid-chitosan oligomer-coated dutasteride NLCs,and found that the formulations could promote cell proliferation especially in DPCs.
3.1.3.Metallic nanoparticles
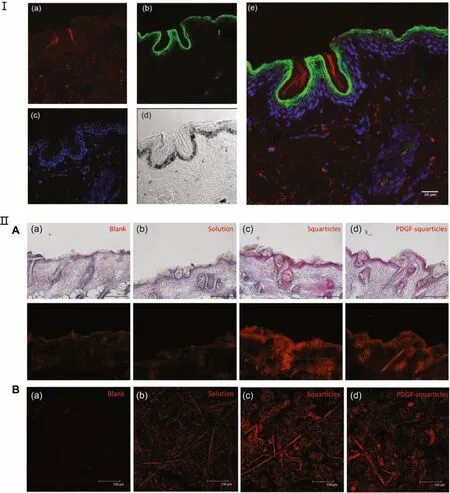
Fig.5-Lipid nanoparticles for hair follicle-targeting drug system.Ⅰ.Confocal microscopy images of human skin incubating with the fluorescence labeled NLC formulation:(a)rhodamine labeled NLCs(red);(b)Alexa Fluor 488 phalloidin labeled actin(green);(c)TO-PRO-3 labeled nucleus(blue);(d)bright field;(e)merge of(a),(b)and(c).[80]Scale bar=20 μm.Ⅱ.(A)H&E staining and fluorescence microphotographs of the skin treated with Nile red labeled minoxidil formulations after 4 h.Scale bar=150 μm.(B)Confocal micrographs showing the distribution of Nile red on the skin surface.Scale bar=150 μm.[73]
Drug molecules can be encapsulated either into the particle core or adsorbed on the particle surface of metallic nanoparticles,including metals (such as iron,gold,or silver)or metal oxides (such as TiO2,ZnO [93],and iron oxide [94]).The previous study [95] showed that metallic nanoparticles with a diameter of less than 10 nm were able to pass passively through the hair follicle pores through the skin and reach the deep region of the hair follicle.Gold nanoparticles(GNPs)possess varied unique features,such as intense visible light absorption,and high control over size and shape,making it an attractive metallic nanoparticle for hair follicle-targeting delivery.Recently,gold microparticles (GMPs) with inner silica cores have been introduced to treat acne vulgaris [96].GMPs applied to the skin surface accumulated abundantly into the PSU through the follicular pathway and combining diode laser pulses,which enabled the direct intercept to the pathophysiology by targeting the sebaceous glands.
Moreover,studies also showed that the size,shape,and surface ligands of metallic nanoparticles could affect the penetration performance of particles into hair follicles (Fig.6I A).For instance,Friedman et al.[97] explored the effects of size as well as the shape on GNPs regarding its possibility for hair follicle permeation.They found that particles with a diameter of 40 nm could penetrate a depth of 210 nm,and 250 nm particles penetrated up to 252 nm,while particles of 530 nm could not penetrate at all (Fig.6ⅠB).Studies on the morphology of GNP have shown that particles in spherical have lower penetration relative to nanorods.Furthermore,nanostars could abundantly accumulate in the PSU (Fig.6Ⅱ),indicating that the anisotropic shapes of nanoparticles play a significant role in particle accumulation.In addition to size and shape,functionalized surface ligands (such as neutral,anionic,cationic,and hydrophobic ligand) on gold nanorods(GNRs)have also been proven to influence the drug deposition into hair follicles in human skin sheets (Fig.6Ⅲ).Mahmoud et al.[98] indicated that hydrophobic polystyrene (PS)-GNRs might be more advantageous for hair follicle-targeting than PEGylated GNRs because of the lipophilic property of the follicular compartments (Fig.6Ⅳ).Consequently,a brannew composite formulation may enable greater follicular penetration of metallic nanoparticles.
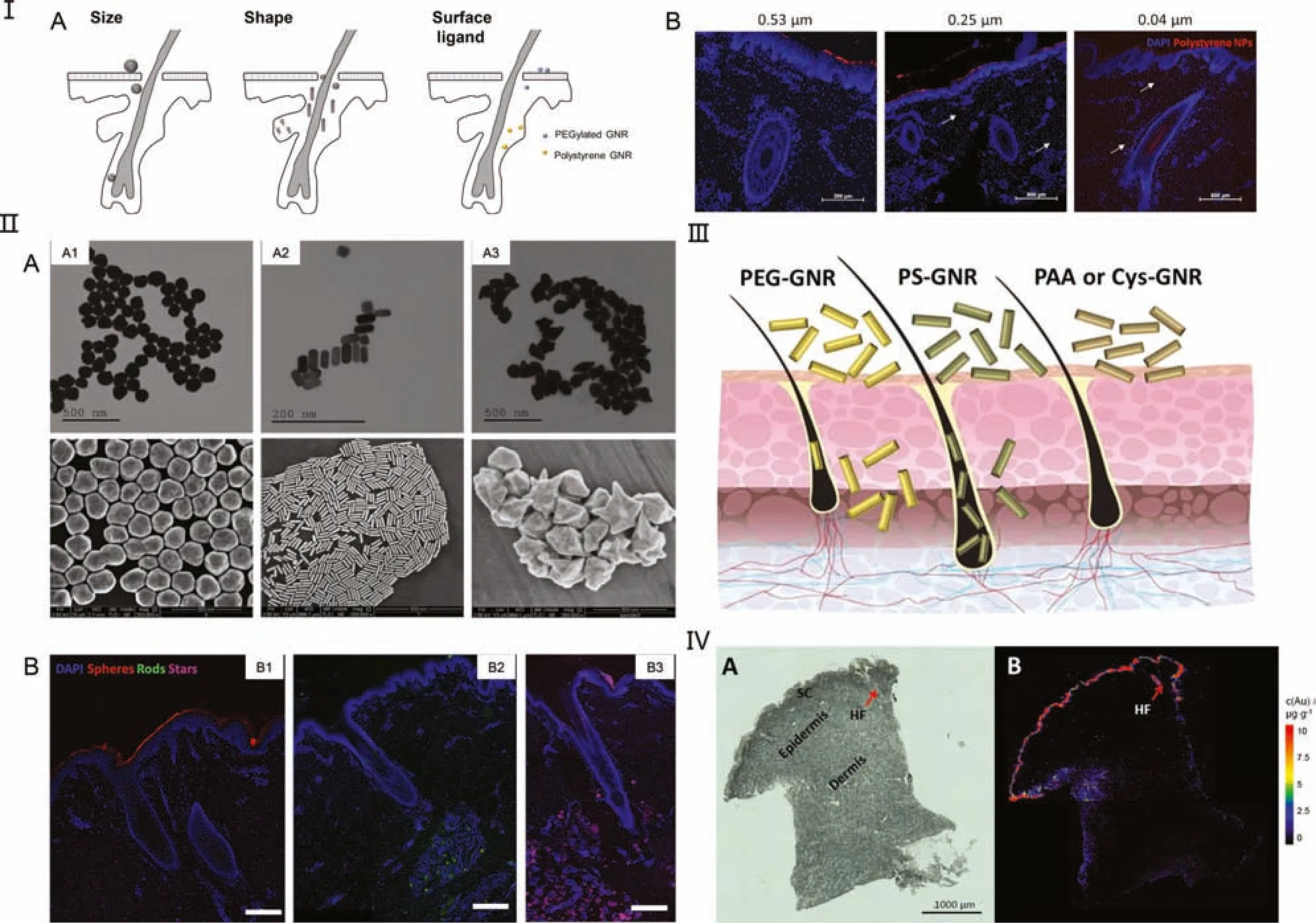
Fig.6-The effect of size,shape,and surface ligands on the capacity to follicular drug delivery of metallic nanoparticles.Ⅰ.(A)Schematic illustration of size,shape,and surface ligand effect of GNPs on follicular penetration.(B)Fluorescence microscopy images of full human skin samples treated fluorescence-labeled Polystyrene nanoparticles with different diameters(Red:fluorescence-labeled nanoparticles;blue:DAPI).[97]Ⅱ.The shape control of GNPs:(A)The transmission electron microscopy(TEM)and scanning electron microscopy(SEM)images of(A1)synthesized spheres,(A2)rods,and(A3)stars GNPs;(B)Follicular penetration of fluorescence-labeled gold(B1)nanospheres,(B2)nanorods,and(B3)nanostars.Scale bar=200 μm.[97]Ⅲ.The effect of surface ligands on the GNR deposition into the hair follicles in human skin(PS:hydrophobic polystyrene).[98]Ⅳ.(A)Microscopic and(B)LA-ICP-MS scanning image exhibiting the distribution of gold in SC,epidermis,dermis,and a hair follicle of human skin sample treated with PEG-GNR for 24 h.Scale bar=1000 μm.[98]
3.2.Microneedles
As a new mode of administration,microneedles (MNs) can easily break the SC barrier and release their loaded drug into the epidermal and dermal layers,thereby delivering drugs into hair follicles directly.MNs with enough mechanical strength are able to puncture into the skin to form microchannels,possessing the merits of self-administration,negligible pain,and relatively inexpensive cost[99-102].Remarkably,applying MNs alone could recruit growth factors through microwounds,at the same time,activate HFSCs and hair growth signaling pathways[103,104].Recently,MNs have been applied to disorders associated with hair follicles to increase the efficiency of percutaneous absorption and reduce dose frequency,which can act synergistically to enhance follicular drug delivery(Table 2).

Table 2-An overview of microneedles for hair follicle-targeting delivery.
Recent advances by Yuan et al.developed ceria nanozyme(CeNZ)-encapsulated microneedles(Ce-MNs)patch,achieving faster hair regeneration with high quality.The CeNZs were efficiently delivered into skin (200-300 nm deep) through MNs,which could relieve oxidative stress and stimulate angiogenesis to remodel the hair follicle’s microenvironment[105].Besides,Fang et al.[106] fabricated a polyvinyl alcohol(PVA)-dissolvable microneedle patch loading mesoporous iron oxide (MIO) and minoxidil (MX-MIO@MNs) to facilitate hair regrowth.MX-MIO@MNs could be triggered by the external magnetic field,promoting local heating and controlled drug release.The releasing MIOs further captured hydrophobic pharmaceuticals,and the hydrophobic substances are the vital substances supporting hair regrowth in the human body.MX-MIO@MNs with appropriate mechanical property could successfully deliver the minoxidil-loaded MIOs to the skin and achieve more than 8-fold improvements in hair growth with no irritation.Others including Cao et al.[107] developed squalene-containing microneedles mediated with FIN NLCs to enhance the permeability to hair follicles and reduce the systemic adverse effects resulting from oral administration.The lipidic composition of NLCs mimicking natural components of hair follicles markedly improved the coumarin 6 (C6)-NLCs uptake in human dermal papilla cells.In vitroandin vivopermeation tests both revealed that the combination of NLCs with MN had significantly higher skin retention compared that in a FIN-NLCs and FIN suspension(Fig.7Ⅰ).Detailed permeation analysis showed that C6-NLCs-MN presented a better delivery of follicular targeting than C6-NLCs or C6-suspension groups.Moreover,FIN-NLCs-MNs exhibited higher therapeutic efficacy of hair regeneration and telogen-to-anagen conversion than the FIN-NLCs or the commercial minoxidil groups on AGA-induced mice.
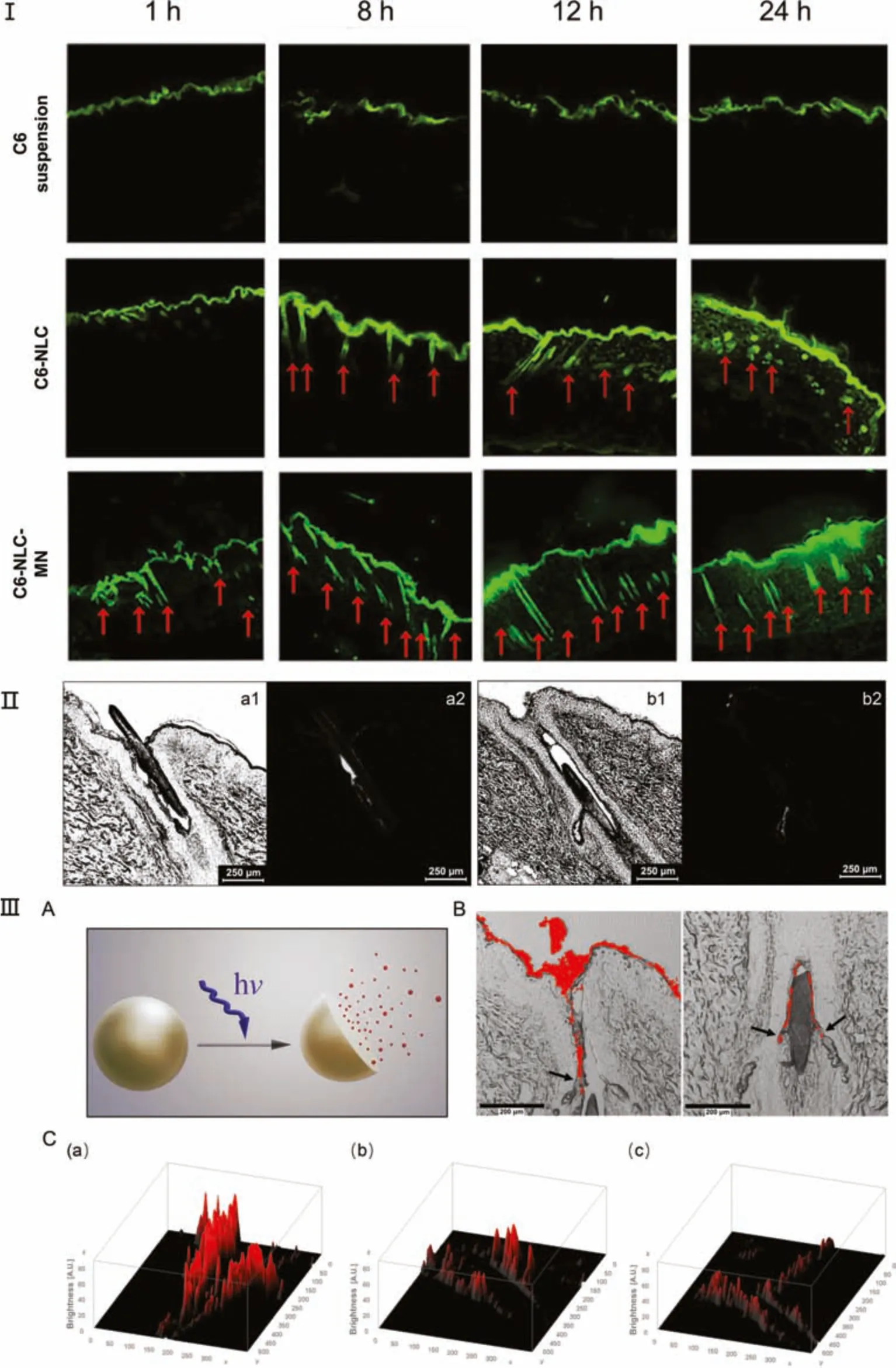
Fig.7-Microneedles and exogenous stimulation-mediated formulations for follicular drug delivery.Ⅰ.Visualization pathway of C6 suspension,C6-NLCs,and C6-NLCs-MN using CLSM after 24 h of permeation in rat skin.[107]Ⅱ.Laser scanning microscopy(LSM)image of a follicular cross-section in the(a1)transmission and(a2)fluorescence mode from the AuNP-doped BSA particles treated group;LSM image of a follicular cross-section with a visible sebaceous gland in the(b1)transmission and(b2)fluorescence mode from the AuNP-doped BSA particles treated group.Scale bar=250 μm.[110]Ⅲ(A)Schematic illustration of UVA-responsive nanocapsules(NCs).(B)CLSM images of porcine ear skin after 2 min of UVA irradiation and incubation with fluorescence-labeled NCs for 30 min.Scale bar=200 μm.(C)Three-dimensional plot images of porcine ear skin treated with fluorescence-labeled NCs after(a)0 min,(b)2 min,and(c)8 min of irradiation with UVA(power density:11.96 mW/cm2,peak wavelength=365 nm).[117]
3.3.Exogenous stimulation-mediated formulations for follicular drug delivery
Furthermore,nanoparticles should be equipped with an appropriate triggered release mechanism to achieve continuous drug release exogenously.In this regard,nanoparticles play an important role in transporting active substances to hair follicles.Different exogenous trigger mechanisms,including infrared light [110],pH[58],and ultrasound (US),ultraviolet (UV)-responsive,are investigated to stimulate a controlled drug release and enable translocation into hair follicles once released.Short periods of heat application may facilitate preferential drug delivery to hair follicles because the viscosity of human sebum reduces as the temperature increases[111].Previous research by Jung et al.showed an increased follicular penetration depth at 37 °C compared to that at 21 °C and 32 °C [112],suggesting that formulations can achieve enhanced follicle deposition above their cloud point temperature.Lademann et al.demonstrated that water-filtered infrared A radiation could facilitate the release of model drugs targeting the follicular structures [110].The plasmonic heat caused by radiation made stronger fluorescent signals for model drugs on the SC layers in addition to the sebaceous glands and follicular ducts in 95.2%of hair follicles(Fig 7Ⅱ).Furthermore,the utilization of the pH gradient is very promising because it has been proven that pH values range from 6.5 on the pig ear skin surface to 7.4 in lower HF regions [113],providing a clear direction for pH-triggered intrafollicular drug delivery.More recently,Dong et al.demonstrated the possibility of a pH-responsive burst drug release from Eudragit® L100 NPs.Electron paramagnetic resonance and CLSM investigations showed transfollicular penetration and increased aggregation into hair follicles [58].What’s more,Liao et al.developed an innovative integrated drug delivery platform by combing US energy with multifunctional microbubbles(MBs).The authors explored the effects of minoxidil-coated lysozyme-shelled MBs and albumin-shelled MBs with US.The results showed that the delivery platform could enhance the deposition of therapeutic drugs to the target structure of interest in the hair follicle,thereby offering new therapeutic opportunities both in hair loss and acne vulgaris [114-116].Similar results were observed by Busch et al.,who developed a follicular targeting ultraviolet A(UVA)-triggered drug system from nanocapsules([117];Fig.7 ⅢA and B).The fluorescence brightness of the model drug decreased with the increase of UVA irradiation time (Fig.7 ⅢC),possibly because the drug was insoluble in the intrafollicular environment.These results indicated that the drug preferentially accumulated in hair follicles.
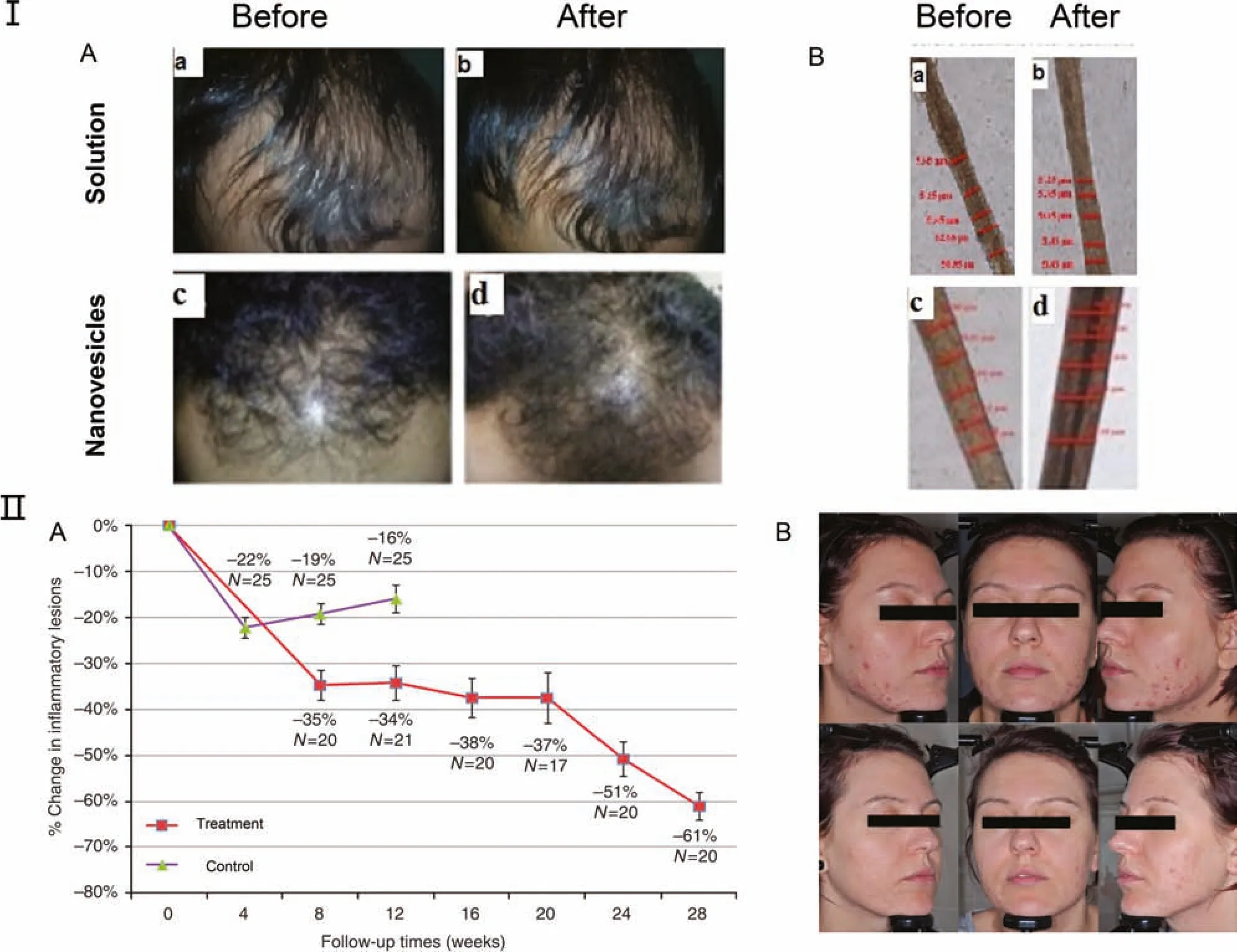
Fig.8-Clinical application of hair follicle-targeting delivery in the treatment of AGA and acne vulgaris.Ⅰ.(A)Two male patients with AGA(a,c)before therapy and(b,d)after 3-month treatment(top row:melatonin solution;bottom row:melatonin nanovesicles).(B)The hair shaft diameter of male patients with AGA(a,c)before therapy and(b,d)after 3-month treatment(top row:melatonin solution;bottom row:melatonin nanovesicles)[118]Ⅱ.(A)The mean percent of inflammatory lesions in the gold microparticles-treated group and control group after 3 months(N:the number of patients at different time point;bar:standard error of the mean).(B)Images showing the lesions of inflammatory acne vulgaris on the cheeks(top row:before therapy;bottom row:after 6-month treatment of gold microparticles).[119]
4.Clinical application
Whereas hair follicle-targeting drug delivery strategies are still limited by regulatory approval in clinical trials,breakthrough therapies are currently underway in small groups of patients.Roque et al.prepared FINloaded PLGA nanoparticles using a modified method for emulsification/solvent diffusion[49].In clinical safety testing,all formulation excipients did not cause any erythema or other untoward effects.Hatem et al.encapsulated melatonin in vitamin C-based nanovesicles to enhance its therapeutic efficacy and skin retention [118].Further studies showed that melatonin nanovesicles clinically increased hair density and diameter and reduced hair loss compared to melatonin solution (Fig.8Ⅰ).Additionally,two independent prospective randomized controlled clinical trials have investigated the topical application of gold-coated silica microparticles in managing moderate to severe acne vulgaris [119].Microparticles with a 15-nm-thick gold shell and 120-nm-diameter silica core,providing deep penetration into the sebaceous glands,appeared statistically effective treatment in each trial.In Trial 1,the lesions of inflammatory acne vulgaris were significantly cut down and reached -61%compared to the baseline at 28 weeks(Fig.8Ⅱ).
The current work demonstrates that hair follicle-targeting drug delivery could reduce side effects and generate more effective treatments.To date,there is a variety of researches concerning an increased follicular penetration when applied with strategies like nanocarrier systems.Still,only very few products based on the conception of hair follicle-targeting are available on the market.Most studies focused on the follicular permeationin vitroorin vivo,and the investigation about their clinical efficacy is rare at present.The relative translation still remains a considerable challenge.On one side,obtaining the same clinical outcomes from penetration experiments in the laboratory is extremely difficult.We often choose porcine,rat,mouse,or hamster skin as the substitute for human skin in the lab,and they invariably produce quite different permeation results.On the other hand,there are still concerns about nanoparticles’potential toxicity,requiring further explorations on the possible dangers and long-term fate of nanomaterials in hair follicles.
5.Conclusions and future perspectives
Hair follicle-targeting drug delivery formulations have been found to obtain overall performance enhancements,which improve drug efficacy by enhancing the skin and follicle drug delivery and decreasing side effects compared to conventional formulations.Based on the particularities of the hair follicles,the drugs trapped in hair follicles enable sustained and controlled release,allowing better patient compliance and treatment efficiency.During the past years,the potential of the hair follicle as a penetration pathway for the treatment of hair follicle-associated disorders like hair loss and acne vulgaris has been recognized.
So far and overall,hair follicle-targeting drug delivery represents a promising concept,and there are additional challenges (Fig.9).Hair follicles are more than a complex structure.For example,most human hair follicles will remain for 2-6 years in the anagen phase.They go through extensive changes with the transformation of the hair follicle cycle.Different cycles status certainly affect the follicular penetration and must be taken into consideration while designing formulations.Furthermore,the sebaceous content also hampers nanoparticle accumulation into the hair follicle.Topically applied substances can’t enter the ‘closed’ hair follicles,as the dry sebum and cell debris would block the hair follicles.Increasing the amounts of drugs that can enter the hair follicle with the presence of the SC should be the focus of future studies.Last but not least,every disease has its own characteristics,and it is difficult to design a compatible delivery system for a new bioactive molecule under a particular skin condition and purpose.It has been reported that the movement of the hair plays a crucial role in the hair follicle targeting process of nanoparticles [23].In disease states like hair loss,the interactions between particles and hair follicles and also the influence of hair should be considered in further studies.Thus,as a future research direction,the selection of corresponding nanocarrier types and more reliable skin models that can mimic the diseased state is absolutely vital for permeation experiments in follicletargeting drug delivery.

Fig.9-Research to clinical:the challenges in future prospect and clinical application for hair follicle-targeting drug delivery.IVIVC:in vivo and in vitro consistence.
CRediT authorship contribution statement
Yueting Gu: Investigation,Writing-original draft.Qiong Bian: Writing-review&editing.Yanjun Zhou: Participation in discussion.Qiaoling Huang: Conceptualization.Jianqing Gao:Conceptualization,Supervision.
Conflicts of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
 Asian Journal of Pharmacentical Sciences2022年3期
Asian Journal of Pharmacentical Sciences2022年3期
- Asian Journal of Pharmacentical Sciences的其它文章
- Gp350-anchored extracellular vesicles:promising vehicles for delivering therapeutic drugs of B cell malignancies
- Salvianolic acid B dry powder inhaler for the treatment of idiopathic pulmonary fibrosis
- New modular platform based on multi-adjuvanted amphiphilic chitosan nanoparticles for efficient lipopeptide vaccine delivery against group A streptococcus
- Sequentially releasing self-healing hydrogel fabricated with TGFβ3-microspheres and bFGF to facilitate rat alveolar bone defect repair
- Elaborately engineering of a dual-drug co-assembled nanomedicine for boosting immunogenic cell death and enhancing triple negative breast cancer treatment
- Changes in target ability of nanoparticles due to protein corona composition and disease state
