Leukoaraiosis is associated with clinical symptom severity,poor neurological function prognosis and stroke recurrence in mild intracerebral hemorrhage:a prospective multi-center cohort study
Tian-Qi Xu ,Wei-Zhi Lin ,Yu-Lan Feng ,Fan-Xia Shen,Jie Chen,Wei-Wen Wu,Xiao-Dong Zhu,Lin Gu,Yi Fu,
Abstract Leukoaraiosis (LA) results from ischemic injury in small cerebral vessels,which may be attributable to decreased vascular density,reduced cerebrovascular angiogenesis,decreased cerebral blood flow,or microcirculatory dysfunction in the brain.In this study,we enrolled 357 patients with mild intracerebral hemorrhage (ICH) from five hospitals in China and analyzed the relationships between LA and clinical symptom severity at admission,neurological function prognosis at 3 months,and 1-year stroke recurrence.Patients were divided into groups based on Fazekas scale scores:no LA (n=83),mild LA (n=64),moderate LA (n=98) and severe LA (n=112).More severe LA,larger hematoma volume,and higher blood glucose level at admission were associated with more severe neurological deficit.More severe LA,older age and larger hematoma volume were associated with worse neurological function prognosis at 3 months.In addition,moderate-to-severe LA,admission glucose and symptom-free cerebral infarction were associated with 1-year stroke recurrence.These findings suggest that LA severity may be a potential marker of individual ICH vulnerability,which can be characterized by poor tolerance to intracerebral attack or poor recovery ability after ICH.Evaluating LA severity in patients with mild ICH may help neurologists to optimize treatment protocols.This study was approved by the Ethics Committee of Ruijin Hospital Affiliated to Shanghai Jiao Tong University (approval No.12) on March 10,2011.
Key Words:clinical symptom severity;functional dependence;intracerebral hemorrhage;leukoaraiosis;modified Rankin scale;National Institute Health of Stroke Scale;prognosis;stroke recurrence;white matter hyperintensities
Introduction
Spontaneous intracerebral hemorrhage (ICH) refers to the non-traumatic rupture of cerebral vessels.The global lifetime risk of ICH after the age of 25 years is estimated as 8.2% (GBD 2016 Lifetime Risk of Stroke Collaborators et al.,2018).ICH is a severe disease with high rates of functional dependence and stroke recurrence,causing heavy burdens on societies and families (Yan et al.,2018).Previous studies have reported that damage to small cerebral vessels is closely related to the course of ICH (Boulouis et al.,2016;Debette et al.,2019).Leukoaraiosis (LA) is a common white matter lesion seen in neuroimaging of older adult individuals (Lin et al.,2015),and is equivalent to what the neuroimaging field typically calls white matter hyperintensities (Zhu et al.,2020).LA is thought to be the result of ischemic injury in small cerebral vessels,which may be attributable to decreased vascular density,blood-brain barrier dysfunction,decreased cerebral blood flow,or impaired cerebral microcirculation (Debette and Markus,2010;Hall et al.,2014;Hainsworth et al.,2017;Moroni et al.,2020).We hypothesized that LA severity may be a potential marker of individual ICH vulnerability,which can be characterized by poor tolerance to ICH attack or poor recovery ability after ICH.
A previous study reported that larger LA volume was associated with higher National Institute of Health Stroke Scale(NIHSS) score at admission,independent of age and infarct size,in small vessel occlusion stroke (Ryu et al.,2017).Their findings indicate that there may be a relationship between LA severity and clinical symptom severity at the time of admission in stroke patients.Inspired by this research,we wondered if LA severity is also associated with the severity of neurological impairment in ICH patients at admission.Because severe ICH patients often present with large hematomas in locations that cause severe disability,we aimed to recruit conscious ICH patients who had relatively mild symptoms and did not require surgery.Additionally,although previous studies have found an association between poor neurological functional outcome and LA in ICH patients (Caprio et al.,2013;Yu et al.,2019),it was unclear whether LA affects functional outcome in mild ICH patients.Furthermore,the relationship between LA and stroke recurrence in ICH patients was unknown.In this study,we aimed to explore the relationships between LA severity and clinical symptom severity at admission,functional dependence and stroke recurrence in mild ICH patients.
Subjects and Methods
Study population
The sample size was calculated based on a significant difference test for the incidence of adverse clinical outcome(α=0.05,1–β=0.8,power=0.8) via PASS 15 software(NCSS LLC.,Kaysville,UT,USA).Additionally,logistic and Cox regression analyses indicated that the sample size should be 10 times greater than the number of independent variables included in the models (Cesana and Antonelli,2016;Tripathi et al.,2020).Conscious ICH patients in the prospective cohort study who had relatively mild symptoms and did not require surgery were recruited from the neurology wards from August 2012 to April 2019 at five independent general hospitals:Ruijin Hospital Affiliated to Shanghai Jiao Tong University,Minhang Hospital Affiliated to Fudan University,Zhongshan Hospital Qingpu Branch Affiliated to Fudan University,The First Hospital of Jiaxing and Ruijin North Hospital.The inclusion criteria were as follows:age ≥ 18 years;diagnosed with acute mild ICH with computed tomography (CT) scan;and complete clinical and imaging data were obtained.The exclusion criteria were as follows:secondary ICH;CT scan performed over 3 days after onset;incomplete clinical or imaging data;no follow-up data;coma;required craniocerebral surgery;and co-occurrence of severe systemic disease that may affect the prognosis.We followed up with the enrolled ICH patients for 1 year.
This study was approved by the Ethics Committee of Ruijin Hospital Affiliated to Shanghai Jiao Tong University (approval No.12) on May 10,2011 (Additional file 1).We obtained the written informed consent form (Additional file 2) from enrolled patients or legally authorized representatives to collect clinical data and process follow-ups.This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidance for protocol reporting(Additional file 3).
Imaging data
All enrolled patients were examined with cranial CT scans.Magnetic resonance imaging examinations were performed with a GE Signa HDxT 3.0 T Superconducting magnetic resonance imaging system (Boston,MA,USA).Relevant imaging parameters were reported in our previous study (Yang et al.,2017).The susceptibility weighted imaging parameters were as follows:time of repetition/time of echo=36/45 ms;flip angle=20°;contiguous slice thickness=2 mm;matrix,448 × 384;number of excitations=0.75.Hematoma location was divided into lobar hematoma and non-lobar hematoma(Samarasekera et al.,2015).Cerebral hematoma volume was calculated by the formula 1/2ABC,where A was the longest diameter of the hematoma on axial CT,B was the diameter that was perpendicular to the longest diameter,and C was the product of the thickness of each layer and the thickness of adjacent layers (Boulouis et al.,2016).
LA was identified as white matter hyperintensities in the fluid attenuated inversion recovery sequence.According to the Fazekas scale (0–6),ICH patients were divided into four groups:no LA (0),mild LA (1–2),moderate LA (3–4) and severe LA (5–6)(Fazekas et al.,1987;Patti et al.,2016).LA severity was regarded as an ordinal categorical variable.Two different radiologists agreed on the assessment of the Fazekas scale (weighted kappa=0.92;P<0.001).Cerebral microbleeds (CMBs) were defined as round or oval lesions with a low signal intensity or loss of signal on susceptibility weighted imaging sequence.CMB diameters generally ranged from 2–5 mm,with the maximum reaching 10 mm.CMBs were divided according to severity into:mild (n=1),moderate (n=2–4) and severe (n≥ 5) (Wilson et al.,2019).Silent brain infarction was defined as a round or oval lesion of cerebral spinal fluid signal with a diameter of 3 to 20 mm.Hyperintensities were shown on the T2-weighted sequence and hypointensities with a hyperintense rim were shown on fluid attenuated inversion recovery sequence.Patients with silent brain infarction should not have definite stroke history or neurological function impairments (Gupta et al.,2016).
Neurological function
The National Institute of Health Stroke Scale score (0–42)was evaluated for each ICH patient at admission to assess clinical symptom severity (Kwah and Diong,2014).This scale consisted of 11 items of neurologic examination,including consciousness,visual fields,eye movements,facial movements,upper limb movements,lower limb movements,ataxia,sensation,language,dysarthria,and hemispatial neglect.Higher NIHSS scores indicate more severe clinical symptoms (Demchuk et al.,2012).After discharge,phone call follow-ups were implemented by the neurologists every 3 months for 1 year.
There were two prognostic endpoints:functional dependence at 3 months after onset and stroke recurrence within 1 year after onset.Functional dependence was defined as modified Rankin Scale (mRS) score >2 (Delcourt et al.,2017).Stroke recurrence was defined as readmission to a hospital with a definite diagnosis of stroke.
Statistical analysis
SPSS 19.0 (IBM,Armonk,NY,USA) was used for linear regression analysis,logistic regression analysis and Cox regression analysis.Clinical data were compared between ICH patients with different LA levels (novs.mildvs.moderatevs.severe).Kolmogorov-Smirnov normal test was first performed on continuous variables.If the data fit the normal distribution in the form of mean ± standard deviation (SD),one-way analysis of variance test was used.For non-normal continuous variables,the Kruskal-Wallis test was applied for comparisons of median (interquartile range).For categorical variables,the Chi-squared test or Fisher’s exact test was used for comparisons of frequency (percentage).
We used linear regression analysis to explore the effect of LA severity on admission NIHSS.Logistic regression analysis was used to investigate the relationship between LA severity and 3-month functional dependence.Cox regression analysis was used to explore the effect of LA severity on 1-year stroke recurrence.We first performed univariate regression analysis to assess for potential risk factors.And then we conducted the backward stepwise multivariate regression analysis.Age,sex and baseline clinical factors associated with dependent variables in the univariate analysis (P-value <0.1) were included in the multivariate regression models.We also assessed ICH patients with no LA as a reference to explore the effects of mild and moderate-to-severe LA on admission NIHSS,functional dependence and stroke recurrence.
Results
Baseline data of spontaneous ICH patients
Of the 400 spontaneous ICH patients recruited for the study,20 patients did not have completed clinical or radiological data,18 patients did not have prognostic data,and 5 patients refused to participate in the study.Therefore,43 ICH patients were excluded.Of the 357 included ICH patients,83 patients did not have LA,64 patients had mild LA,98 patients had moderate LA and 112 patients had severe LA (Figure 1).During the 1-year follow-up,7 patients died because of stroke recurrences,1 patient died due to lung infection and 1 patient died because of heart disease.The mean age of the final cohort was 63 ± 13 years.Two hundred and seventythree patients (66.4%) were male.The median hematoma volume was 5.5 mL (interquartile range,2.0–12.8 mL),the median score of admission NIHSS was 3 (interquartile range,2–6),and the median score of admission Glasgow coma scale (GCS) was 15 (interquartile range,15–15).When the baseline characteristics of the study population were divided by LA severity,we found that age,hypertension,prior stroke,admission NIHSS,admission glucose,CMBs,functional dependence and stroke recurrence differed between LA severity groups (Table 1).
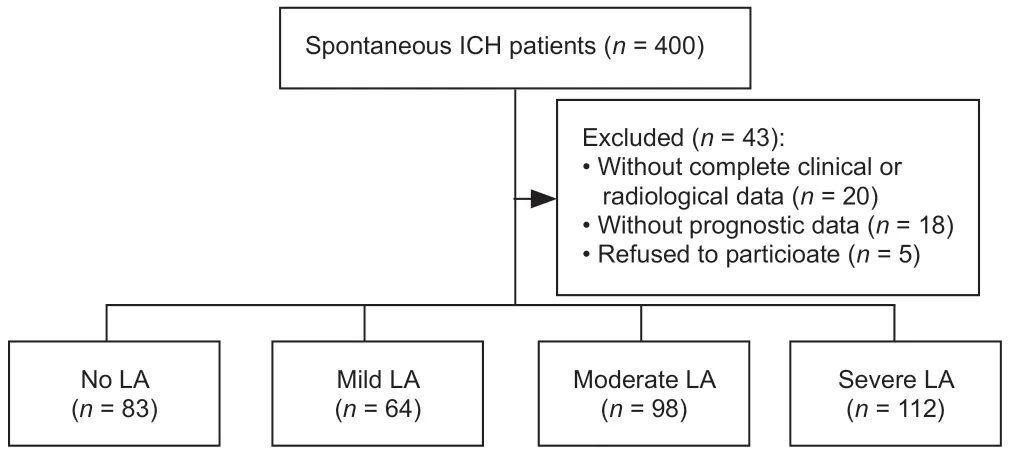
Figure 1|Flow chart of patient assignment.
LA severity is associated with admission NIHSS in linear regression analysis
The severity of clinical symptoms at admission was measured by NIHSS (0–42).We first performed univariate regression analysis to identify risk factors that might be associated with admission NIHSS (Additional Table 1).Then,variables with aPvalue <0.1 in the univariate analysis were included in the regression model for multivariate analysis.We found that LA severity,hematoma volume and admission glucose were positively correlated with admission NIHSS in ICH patients.Additionally,the clinical symptoms of patients with lobar ICH were milder than those of patients with non-lobar ICH (Table 2).

Table 1|Baseline characteristics of the study population divided by LA severity
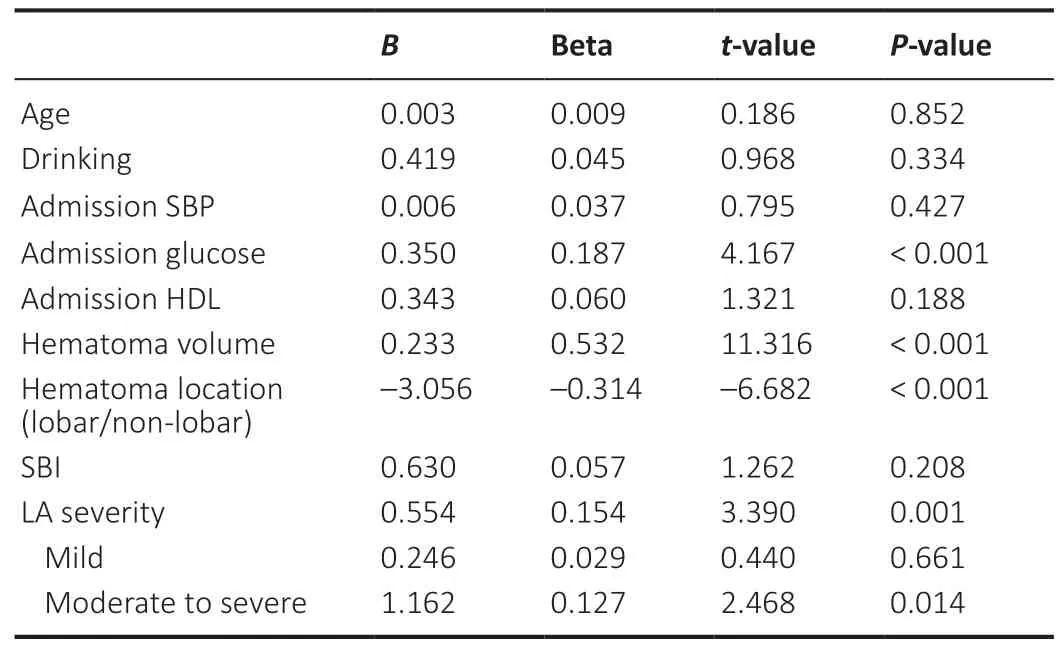
Table 2|LA severity is associated with admission NIHSS score in multivariate linear regression analysis
LA severity is associated with 3-month functional dependence in logistic regression analysis
During the follow-up period,62 patients (17.4%) experienced functional dependence at 3 months from onset;of those,6 (7.2%) had no LA,8 (12.5%) had mild LA and 48 (22.9%)had moderate-to-severe LA.We first performed univariate regression analysis (Additional Table 2),followed by multivariate regression analysis.LA severity,age,hematoma volume and hematoma location were associated with 3-month functional dependence in ICH patients (Table 3).
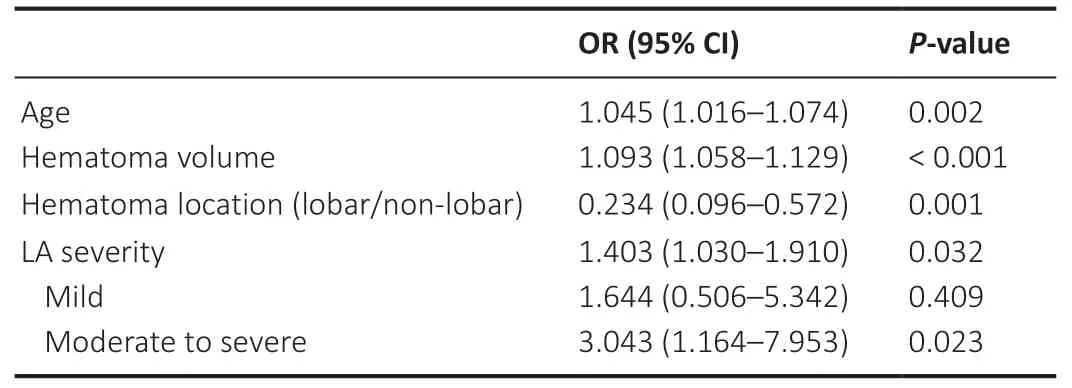
Table 3|LA severity is associated with 3-month functional dependence in multivariate logistic regression analysis
Moderate-to-severe LA is associated with 1-year stroke recurrence in Cox regression analysis
Forty-three patients (11.7%) suffered stroke recurrences within 1 year from onset;of those,30 patients suffered from cerebral infarction,12 suffered from ICH and one suffered from mixed stroke.In patients with no LA,five people (7.8%)were diagnosed with recurrent stroke,four with cerebral infarction and one with ICH.In mild LA patients,four people(6.3%) were diagnosed with recurrent stroke,three with cerebral infarction and one with ICH.In moderate-to-severe LA patients,34 people (16.2%) were diagnosed with recurrent stroke,23 with cerebral infarction,10 with ICH and one with mixed stroke.Univariate analysis was first performed to identify risk factors associated with stroke recurrence(Additional Table 3).A multivariate binary stepwise Cox regression analysis indicated that moderate-to-severe LA,admission triglyceride and silent brain infarction were related to 1-year stroke recurrence in ICH patients (Table 4).
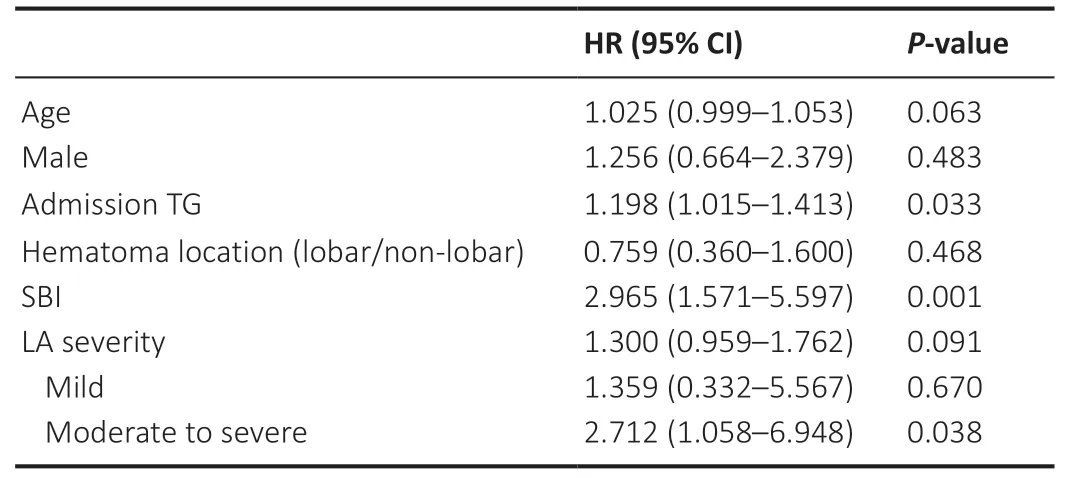
Table 4|Moderate-to-severe LA is associated with 1-year stroke recurrence in multivariate Cox regression analysis
Discussion
In the present study,we investigated the relationships between LA severity and clinical symptom severity at admission,functional dependence and stroke recurrence in mild ICH patients.We found that LA severity was positively associated with admission clinical symptom severity and 3-month functional dependence.In addition,moderate-tosevere LA was an independent predictor for 1-year stroke recurrence.
Our data showed that LA severity was positively associated with admission NIHSS score in mild ICH patients.LA severity was also positively associated with hematoma volume and location.These results suggest that LA severity may influence the early clinical manifestation.The ability to withstand acute hemorrhagic injury may be partly dependent on good cerebral blood flow and collateral flow and the integrity of white matter tracts connecting different parts of the brain.However,severe LA destroys white matter fiber integrity and reduces vascular density.It has been reported that reduced vascular density and microcirculatory dysfunction are associated with the aggravation of LA (Wardlaw et al.,2013).This may explain why LA severity was associated with admission NIHSS score in ICH patients in the present study.A previous study reported that in patients with small vessel occlusion stroke,higher LA volume was related to higher admission NIHSS score (Ryu et al.,2017),which is consistent with our findings in mild ICH patients.Our findings suggest that in mild ICH patients,it is necessary to consider the potential influence of LA severity on admission NIHSS score,in addition to hematoma volume and location.
In addition,we found that ICH patients with severe LA were more likely to experience poor functional outcome and recurrent stroke.A previous study reported that moderateto-severe LA was related to 3-month functional dependence for ICH patients;the study used the visual rating scale (0–4) to assess the extent of LA (Uniken Venema et al.,2019).In our study,the Fazekas scale was adopted to grade the severity of LA,and also demonstrated that LA severity was associated with functional outcomes in ICH patients.Furthermore,Kumral et al.(2015) reported that mild stroke patients with LA had a higher recurrent stroke risk within 5 years.Our study adds to these findings by showing that in ICH patients,moderate-to-severe LA was associated with 1-year stroke recurrence.LA can lead to the destruction of myelin and proliferation of glial cells,and subsequently slow down neural network reorganization (Joutel and Chabriat,2017;Shaaban et al.,2017).These findings might explain the role of LA on worsening functional outcome.Microcirculatory dysfunction and decline in cerebrovascular angiogenesis were found to be related to the aggravation of LA (Yang et al.,2018).The influence of LA on the blood–brain barrier,cerebral blood flow,and cerebrovascular angiogenesis may contribute to the worse outcome and higher recurrence in ICH patients.
To the best of our knowledge,this is the first study to explore the relationship between LA and clinical symptom severity at admission in mild ICH patients.There were some limitations that should be addressed.First,the number of patients with recurrent cerebral infarction was insufficient,which made effective logistic regression analysis impossible,as was the number of patients with recurrent ICH.Therefore,we had to combine recurrent cerebral infarction cases and recurrent ICH cases as recurrent stroke.Second,our results showed that mild LA had no effect on stroke recurrence,which might be due to the relatively small sample sizes or short follow-up periods.Finally,we recruited conscious ICH patients who had relatively mild symptoms and did not require surgery from neurology wards.The median hematoma volume (5.5 mL,interquartile range:2.0–12.8 mL) of the enrolled patients was smaller than what has been reported in other studies (Boulouis et al.,2016),which may contribute to the lack of association between LA and hematoma volume in this study.
In conclusion,we found that LA severity was positively associated with clinical symptom severity at the time of admission,3-month functional dependence and 1-year stroke recurrence in mild ICH patients.These findings suggest that LA may be a useful marker of individual brain ICH vulnerability,which can be characterized by poor ICH tolerance and recovery ability.Assessment of LA severity in mild ICH patients may help neurologists optimize therapeutic decisions.
Author contributions:Study conception and design:YF;data collection:WZL‚YLF‚FXS‚JC‚WWW‚XDZ‚LG;statistical analysis and manuscript writing:TQX.All authors read and approved the manuscript
Conflicts of interest:The authors declare no conflicts of interest.
Financial support:The study was supported by the National Natural Science Foundation of China‚Nos.81771281 (to FXS)‚81471177 (to FXS);and the Natural Science Foundation of Shanghai of China‚No.20ZR1434200 (to YF).The funding bodies played no role in the study design‚collection‚analysis and interpretation of data‚in the writing of the report‚or in the decision to submit the paper for publication.
Institutional review board statement:This study was approved by the Ethics Committee of Ruijin Hospital‚which is affiliated with Shanghai Jiao Tong University School of Medicine (approval No.12) on March 10‚2011.
Declaration of patient consent:The authors certify that they have obtained all appropriate patient consent forms from the patients.In the forms‚the patients have given their consent for their images and other clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal the patients’identity.
Reporting statement:This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidance for protocol reporting.
Biostatistics statement:The statistical methods of this study were reviewed by the Department of Epidemiology and Biostatistician‚School of public health‚Shanghai Jiao Tong University.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Patient-related data will be shared upon request by the corresponding author or any qualified investigator.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal‚and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License‚which allows others to remix‚tweak‚and build upon the work non-commercially‚as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Nicholas D.Davenport‚Minneapolis Veterans Affairs Health Care System‚USA.
Additional files:
Additional file 1:Hospital ethics approval (Chinese).
Additional file 2:Informed consent form (Chinese).
Additional file 3:STROBE checklist.
Additional file 4:Open peer review report 1.
Additional Table 1:LA severity is associated with admission NIHSS score in univariate linear regression analysis.
Additional Table 2:LA severity is associated with 3-month functional dependence in univariate logistic regression analysis.
Additional Table 3:LA severity is associated with 1-year stroke recurrence in univariate Cox regression analysis.
- 中国神经再生研究(英文版)的其它文章
- Towards a comprehensive understanding of p75 neurotrophin receptor functions and interactions in the brain
- Microglia regulation of synaptic plasticity and learning and memory
- Stroke recovery enhancing therapies:lessons from recent clinical trials
- Functional and immunological peculiarities of peripheral nerve allografts
- MicroRNA expression in animal models of amyotrophic lateral sclerosis and potential therapeutic approaches
- Significance of mitochondrial activity in neurogenesis and neurodegenerative diseases