Network meta-analysis of randomized controlled trials on esophagectomies in esophageal cancer: The superiority of minimally invasive surgery
Lajos Szak6, David Németh,Nelli Farkas,Szabolcs Kiss,Réka Zsuzsa Dimotor,Marie Anne Engh, PeterHegyi, Balint Eross,Andras Papp
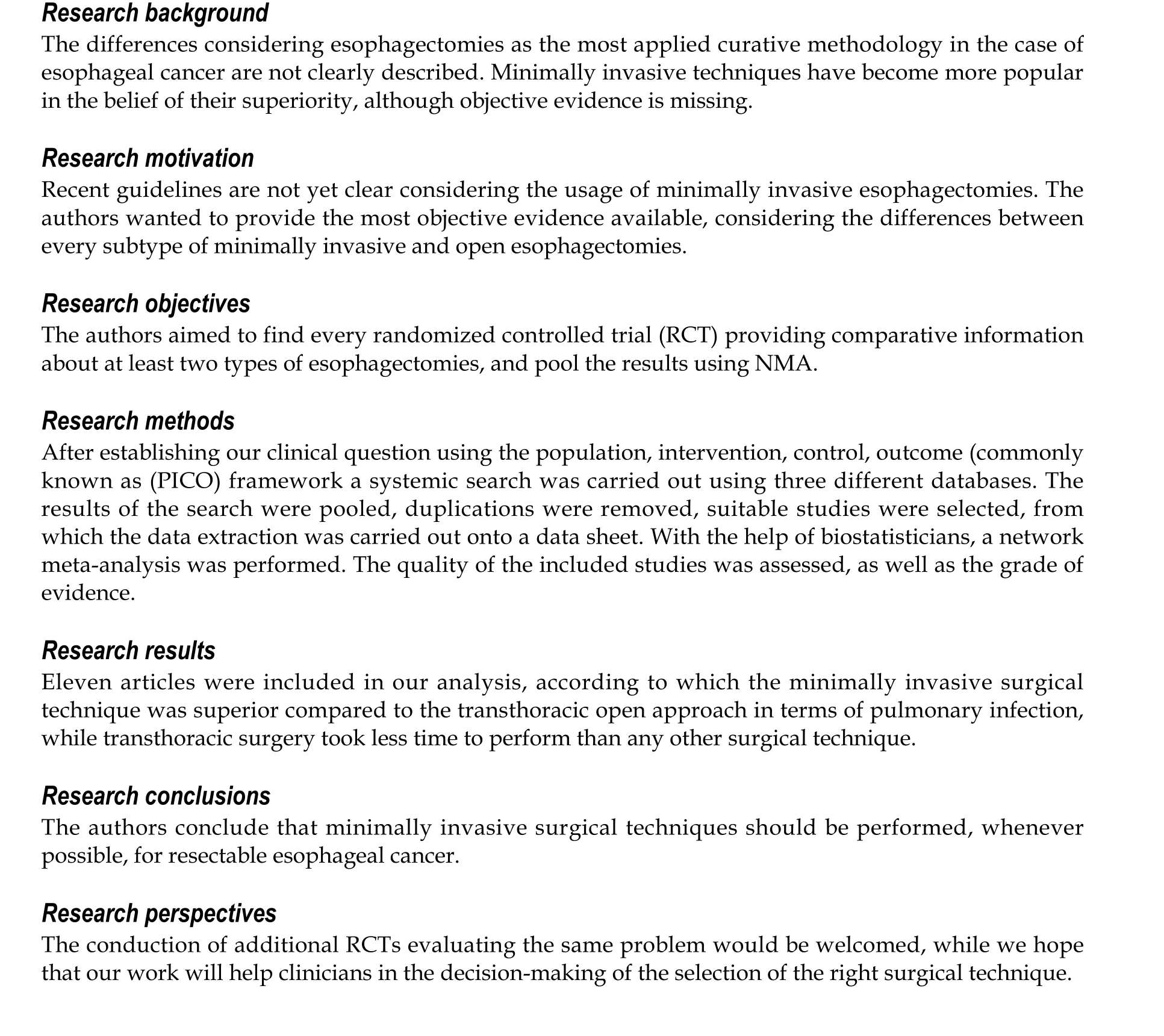
Abstract
Key Words: Surgery; Esophageal cancer; Esophagectomy; Network meta-analysis; Minimally invasive;Laparoscopy
lNTRODUCTlON
Esophageal cancer is the eighth most common type of cancer worldwide[1], with an incidence of 5.2 per 100000 for squamous cell cancer (SCC) and 0.7 per 100000 for adenocarcinoma (AC)[2]. While the prognosis varies between the two histological diagnoses, both AC and SCC are associated with poor clinical outcomes, with a 5-year survival rate of 20%[3].
Surgical therapy plays an essential role in the treatment of esophageal cancer. However, it cannot be routinely used due to the late diagnosis, as symptoms usually occur when the cancer is already unresectable[4]. Traditionally, open surgical interventions are performed, including transhiatal and transthoracic techniques. A meta-analysis comparing these two open surgical modalities did not find a significant difference in 5-year survival[5]. While both techniques are successful in terms of removing the neoplasm, open esophagectomies are associated with significant limitations, most importantly,postoperative morbidity[6,7].
A transition to non-open surgical techniques has been the trend in almost every field of surgery in recent years[8]. A wide variety of non-open techniques are available, including minimally invasive surgery (thoracolaparoscopic) surgery or even robot-assisted esophagectomy[9,10]. In the form of hybrid surgical intervention, a combination of open and non-open technique is available[11].
Previous meta-analyses have compared the different types of surgical techniques, with variable success and significant limitations[12-19]. To date, convincing evidence is missing regarding the optimal surgical approach of resectable esophageal cancer, as it is presented in a recent guideline[20].
Network meta-analysis (NMA) is a relatively novel methodology, which allows the direct and indirect comparison of multiple interventions, thus providing more information than traditional metaanalyses. Indirect comparisons can be made in the case of missing trials comparing two interventions if those are compared with a third intervention[21]. Several meta-analyses were carried out focusing on esophageal cancer surgery, but none of those addressed the problem of the wide variety of surgical techniques.
The purpose of our study was to provide objective evidence considering the surgical treatment of resectable esophageal cancer by comparing each treatment modality in the form of an NMA and possibly rank the different approaches.
MATERlALS AND METHODS
The NMA was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses-NMA guideline[22].
Protocol
The NMA protocol was registered in advance in PROSPERO under the number CRD42020160978.Analyses of the mortality and quality of life could not be carried out due to the low number of reporting articles. The risk of bias was assessed using an updated risk assessment tool.
Search strategy and inclusion criteria
We conducted a systematic search of the MEDLINE (viaPubMed), EMBASE,Reference Citation Analysis(https://www.referencecitationanalysis.com/) and Cochrane Central Register of Controlled Trials(CENTRAL) from initiation until 2019 November to identify studies, comparing at least two types of esophagectomies from transthoracic, transhiatal, hybrid, laparoscopic or robot-assisted approach treating esophageal cancer without the restriction of histological subtype and an NMA was performed.The following search key was used: (((esophagus OR oesophagus OR esophageal OR oesophageal)AND (tumor OR tumour OR malign* OR cancer OR adenocarcinoma OR carcinoma)) AND(esophagectomy OR oesophagectomy OR Ivor-Lewis OR „Ivor Lewis” OR hybrid OR laparoscop* OR„minimal invasive”)) AND random*. We also reviewed the reference lists of eligible articles for further studies. Only randomized controlled trials (RCTs) were included.
Selection and data extraction
After the removal of duplications, two independent reviewers (Szakó L, Engh MA) executed the selection first by title, second by abstract, last by full text following pre-discussed aspects. Data extraction was done by the same two independent reviewers (Szakó L, Engh MA) onto a pre-established Excel worksheet (Office 365, Microsoft, Redmond, WA, United States). Extracted data consisted of the year of publication, name of the first author, study design, country, applied surgical modalities,mortality, overall survival rate (referred as survival), adverse events (AEs), blood loss, length of hospitalization, length of surgical procedure, and demographic data including age, male-female ratio, and SCC/AC ratio. Disagreements regarding both selection and data extraction were resolved by consensus.If consensus could not be reached, a third reviewer (Dömötör RZ) resolved the disagree-ment.
Statistical analysis
The Bayesian method was used to perform pairwise meta-analyses and NMAs. All analyses were carried out using a random effects model. To ensure the interpretability of the NMA results (pooled of direct and indirect data), we presented the geometry of the network, the results with probabilistic statements, and estimates of intervention effects along with their corresponding 95% confidence intervals (CIs), as well as forest plots for ranking the interventions, we chose to use the surface under the cumulative ranking (SUCRA) curve, which provides a numerical summary of the rank distribution of each treatment.
Risk of bias assessment and quality of evidence
The risk of bias assessment was performed at the individual study level, according to the Revised Cochrane risk-of-bias tool for RCTs[23].
The Grading of Recommendations Assessment, Development, and Evaluation system was used to assess the certainty of evidence into four levels: high, moderate, low, and very low. The certainty of the evidence was classified into four levels: high, moderate, low, and very low. Two independent reviewers(Szakó L, Engh MA) decided the overall quality of the evidence[24]. Disagreements were resolved by consensus. If consensus could not be reached, a third reviewer (Dömötör RZ) resolved thedisagreement.
RESULTS
Selection process
The database search yielded 3335 records, of which 2002 articles were left after removing duplicates.Twenty-one full-text articles were screened for eligibility. Finally, we included 11 RCTs (25-35),including 1525 patients, in the quantitative synthesis (Figure 1). Baseline characteristics of the enrolled studies are presented in Table 1[25-35].
Outcomes
A significant difference was found for pulmonary infection, which favored the minimally invasive intervention compared to transthoracic surgery (relative risk [RR]: 0.49, 95%CI: 0.23-0.99) (Figure 2).Operation time was significantly shorter for the transhiatal approach compared to transthoracic surgery(mean difference: -86 min, 95%CI: -150 to -29 min), hybrid intervention (mean difference -99 min, 95%CI:-190 to -9.4 min), minimally invasive technique (mean difference -130 min, 95%CI: -210 to -53 min), and robot-assisted esophagectomy (mean difference -150 min, 95%CI: -250 to -52 min) (Figure 3). We did not find significant differences regarding survival (Supplementary Figures 1-5), total AEs (Supplementary Figure 6), cardiac AEs (Supplementary Figure 7), anastomotic leakage (Supplementary Figure 8),atrial fibrillation (Supplementary Figure 9), wound infection (Supplementary Figure 10), total pulmonary AEs (Supplementary Figure 11), vocal chord paralysis (Supplementary Figure 12), length of hospital stay (Supplementary Figure 13), and blood loss (Supplementary Figure 14). The ranking and detailed results of the comparisons of the interventions are presented in the supplementary files (Supplementary Figures 1-14).
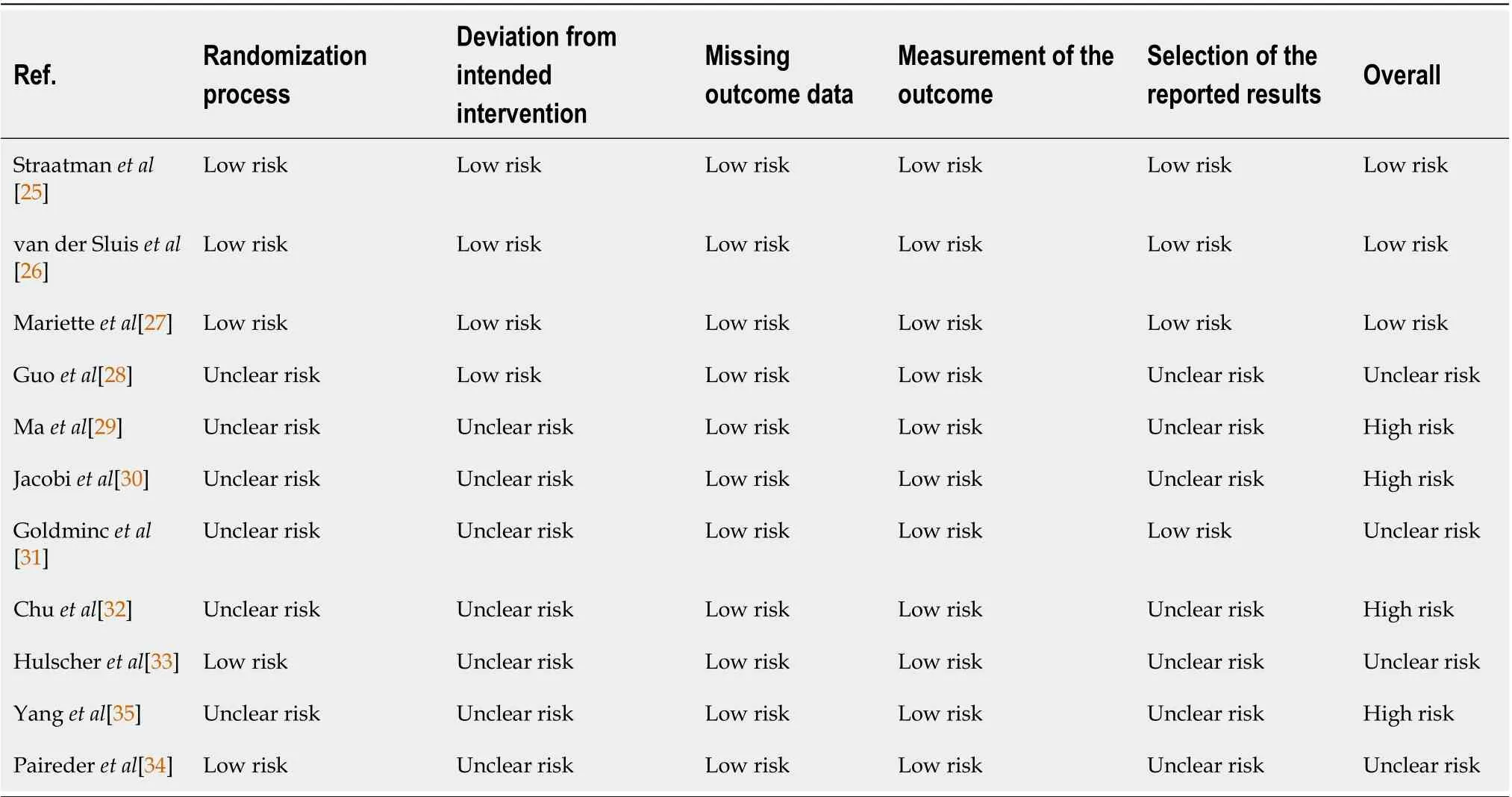
Table 2 The results of the risk of bias assessment by each domain
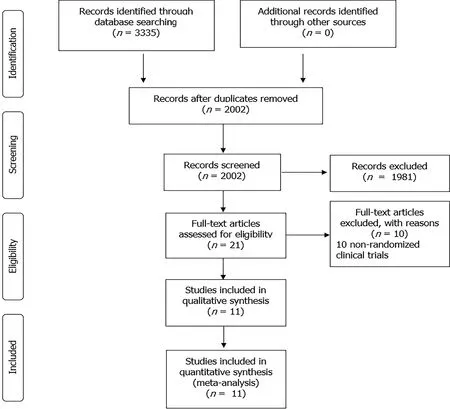
Figure 1 Results of the selection process according to the Preferred Reporting ltems for Systematic Reviews and Meta-Analyses guidelines. Available from: https://prisma-statement.org//prismastatement/flowdiagram.aspx.
Risk of bias assessment and grade of evidence
Results of the risk of bias assessment for the outcome of survival were assessed following the Cochrane Risk of Bias Assessment Tool 2. Details are shown in Table 2.
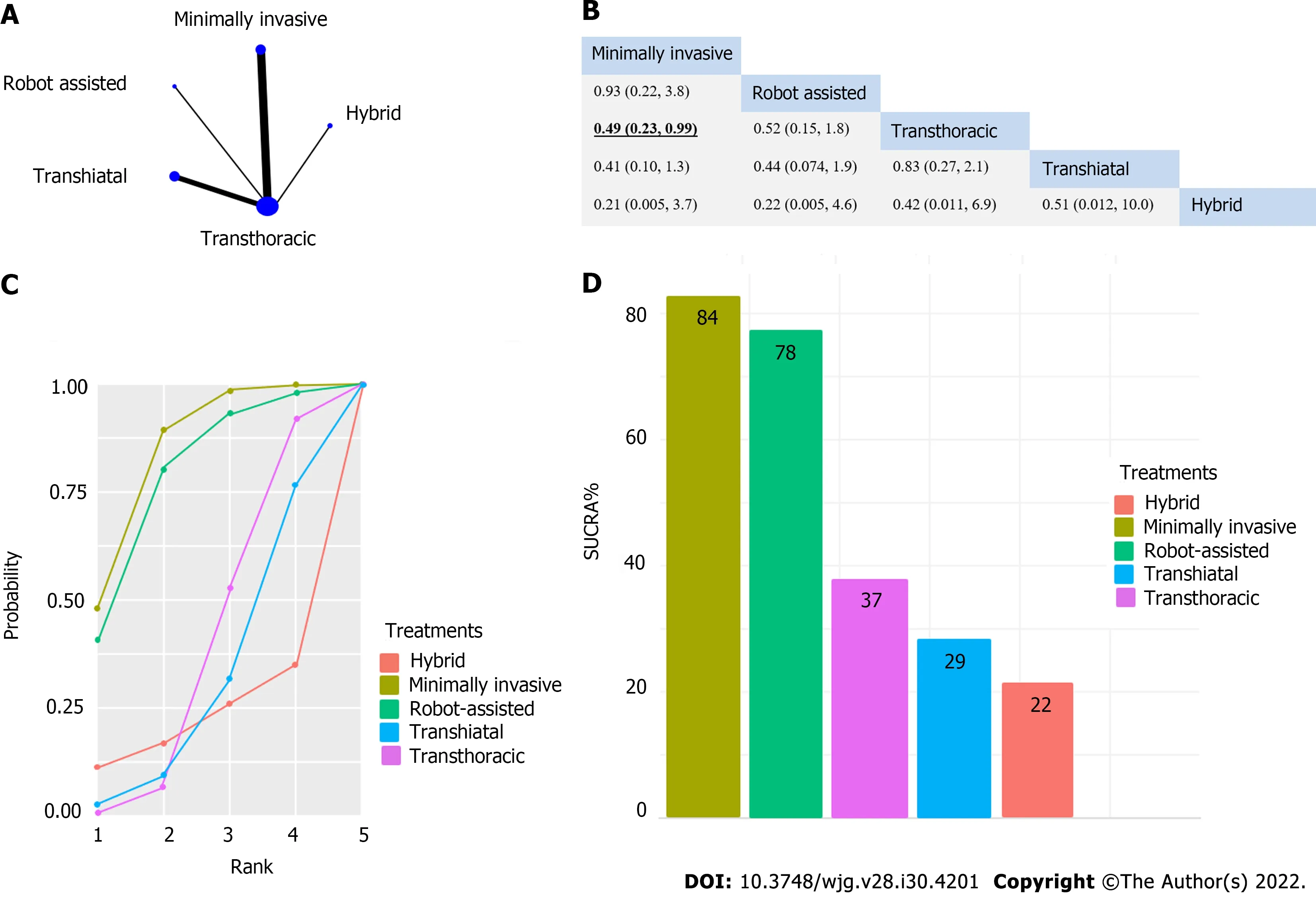
Figure 2 A significant difference was found considering pulmonary infection, which favored the minimally invasive intervention compared to transthoracic surgery. A: The network of eligible studies for pulmonary infection (the width of the lines is proportional to the number of trials comparing every pair of treatments, and the size of every circle is proportional to the number of randomly assigned participants [sample size]); B: League table of the analysis for pulmonary infection. Comparisons should be read from left to right. The values are presented in risk ratios, with corresponding credible interval.Significant result is in TextTitle and underlined; C: Cumulative probability of treatment rank; D: Treatment rank in SUCRA% histogram.
The results of the certainty of evidence are presented in Supplementary Table 1.
DlSCUSSlON
Our NMA confirmed the superiority of the minimally invasive esophagectomy over transthoracic open surgery regarding one of the main complications during these procedures, namely pulmonary infection.On the other hand, non-open surgical techniques require significantly more time to perform compared to open techniques. While statistically significant results were only achieved in the case of pulmonary infection, a clear tendency was demonstrated by the SUCRA curves, showing a preference for non-open techniques, which is also supported by the individual studies.
The results of previous meta-analyses and systematic reviews are not congruent regarding the comparison of minimally invasive and open surgical techniques. Kauppilaet al[14] described the superiority of minimally invasive esophagectomy (MIE) regarding quality of life (QoL), which our work failed to analyze, as there were not enough RCTs reporting on QoL. Guoet al[13] also described the advantages of minimally invasive techniques regarding total complication rate, intraoperative blood loss, wound infection, and pulmonary infection, supporting our findings. MIE was also favorable in the analysis of Wanget al[19] considering blood loss. Besides blood loss and hospital stay, fewer respiratory complications were also shown by MIE in a meta-analysis conducted by Nagpalet al[15]. The work of Yibulayinet al[18] also supports the superiority of MIE in terms of in-hospital mortality and postoperative morbidity. By contrast, Dantocet al[12] focused on oncological outcomes in their metaanalysis, where significant differences could not be proven. Sgourakiset al[17] showed that open surgery was more beneficial in terms of anastomotic stricture, while morbidity favored MIE. Ooret al[16] also described the benefit of open surgery in the case of hiatal hernia. The above comprehensive studies show that the inclusion of non-randomized studies carries a notable limitation.

Figure 3 Operation time was significantly shorter for transhiatal approach compared to transthoracic surgery, hybrid intervention,minimally invasive technique, and robot-assisted esophagectomy. A: The network of eligible studies for operation time [the width of the lines is proportional to the number of trials comparing every pair of treatments, and the size of every circle is proportional to the number of randomly assigned participants(sample size)]; B: League table of the analysis for operation time. Comparisons should be read from left to right. The values are presented in weighted mean difference (minutes), with corresponding credible interval. Significant results are in TextTitle and underlined; C: Cumulative probability of interventions rank; D:Intervention ranking in surface under the cumulative ranking (SUCRA)% histogram.
Although the results of our analysis are only supportive in terms of pulmonary complication, the future perspectives are promising regarding minimally invasive esophagectomy, as the limelight shifts towards robot-assisted surgical techniques. The technique is time consuming, but with the development of new robotic platforms, the benefit of less AEs and more precise procedure will overcome this limitation[36]. The steep learning curve will be possibly managed by allowing the intervention to be carried out only in larger centers, as it has been seen in northern countries[37]. Despite the missing cumulative evidence, minimal invasive techniques have become the gold standard interventions for esophageal cancer since the TIME study. The results of this RCT provide evidence for using minimally invasive surgery for patients with resectable esophageal cancer aimed toward improving postoperative outcomes (especially pulmonary complication) and QoL with comparable oncologic results[25].
Considering the strengths of our analysis, by the inclusion of only RCTs, we managed to achieve a higher quality of evidence than previous works. Furthermore, a thorough methodology was applied.With the application of NMA, we were also able to make indirect comparisons. To date, this work is the most comprehensive review of the available RCTs.
One of the limiting factors of our study was the low number of cases and limited number of direct comparisons. Other limitations were the different enrollment criteria of the individual studies considering the histological subtype and stage of esophageal cancer. Furthermore, our analysis included many indirect comparisons, with weak direct comparisons. Additionally, we only included studies published until 2019.
We emphasize the application of MIE over open surgical techniques. Further analyses should focus on the outcomes of robot-assisted esophagectomies, and direct comparisons should be carried out between robot-assisted esophagectomy and thoracolaparoscopic intervention. Following recent trends,the centralization of upper gastrointestinal surgery is suggested, thus achieving the possibility of the implementation of such techniques without the limitation originating from the low number of cases and the learning curve of minimally invasive techniques.
CONCLUSlON
While practice is already shifting towards the application of minimally invasive techniques, it should be noted that clear evidence is still needed to form guidelines. As we aimed to fill this void, we were only able to prove the beneficial nature of these techniques regarding pulmonary infection. To further assess any other potential differences between the techniques, RCTs and systematic analysis of these trials are needed.
ARTlCLE HlGHLlGHTS
FOOTNOTES
Author contributions:Szakó L conceptualized the work, contributed to establishment of the search key, selection strategy, data extraction, interpretation of the results, and writing of the manuscript; Németh D and Farkas N performed the bio-statistical analyses, and contributed to the interpretation of the results and writing of the manuscript; Kiss S helped was involved in the conceptualization, coordination of the work, and writing the manuscript; Dömötör RZ conceptualized, wrote, and critically appraised the manuscript; Engh MA was involved in the conceptualization, data extraction, risk of bias assessment, writing of the manuscript, and language revision of the manuscript; Hegyi P contributed to the conceptualization, interpretation of the results, critical appraisal, and writing of the manuscript; Erőss BM conceptualized the work, interpreted the results, critically appraised and wrote the manuscript; Papp A provided supervision, and was involved in the conceptualization, interpretation of the results, critical appraisal, and writing of the manuscript.
Conflict-of-interest statement:All authors have no conflicts of interest to declare.
PRlSMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Hungary
ORClD number:Lajos Szakó 0000-0001-9783-4076; Dávid Németh 0000-0002-3258-6195; Nelli Farkas 0000-0002-5349-6527; Szabolcs Kiss 0000-0001-5032-866X; Réka Zsuzsa Dömötör 0000-0002-3561-2539; Marie Anne Engh 0000-0003-4269-5130; Péter Hegyi 0000-0003-0399-7259; Balint Eross 0000-0003-3658-8427; András Papp 0000-0002-2845-531X.
S-Editor:Ma YJ
L-Editor:Filipodia
P-Editor:Cai YX
 World Journal of Gastroenterology2022年30期
World Journal of Gastroenterology2022年30期
- World Journal of Gastroenterology的其它文章
- Alcohol-related diseases and liver metastasis: Role of cell-free network communication
- Benefits of minimally invasive surgery in the treatment of gastric cancer
- Contrast-enhanced ultrasound of a traumatic neuroma of the extrahepatic bile duct: A case report and review of literature
- ANGPT: Angiopoietin; VEGFA: Vascular endothelial growth factor; PGF: Placental growth factor; AFP: Alpha-fetoprotein; IQR: Interquartile range; SD:Standard deviation, SE: Standard error.
- Hepatocellular carcinoma, decompensation, and mortality based on hepatitis C treatment: A prospective cohort study
- Epidemiology of inflammatory bowel diseases in the state of Rio Grande do Sul, Brazil
