Heart failure with reduced,mildly reduced,or preserved left ventricular ejection fraction: Has reasoning been lost?
Andrew Xanthopoulos,Grigorios Giamouzis,John Skoularigis,Filippos Triposkiadis
Andrew Xanthopoulos,Grigorios Giamouzis,John Skoularigis,Filippos Triposkiadis,Department of Cardiology,University Hospital of Larissa,Larissa 41110,Greece
Abstract Left ventricular (LV) ejection fraction (LVEF),defined as LV stroke volume divided by end-diastolic volume,has been systematically used for the diagnosis,classification,and management of heart failure (HF) over the last three decades.HF is classified as HF with reduced LVEF,HF with midrange or mildly reduced LVEF,and HF with preserved LVEF using arbitrary,continuously changing LVEF cutoffs.A prerequisite for using this LVEF-based terminology is knowledge of the LVEF normal range,which is lacking and may lead to erroneous conclusions in HF,especially at the higher end of the LVEF spectrum.
Key Words: Arbitrary;Cut off;Guidelines;Limitations;Normal left ventricular ejection fraction range;Phenotypic persistence
TO THE EDITOR
Left ventricular (LV) ejection fraction (LVEF),defined as LV stroke volume divided by LV end-diastolic volume,is the only biomarker that has been systematically used for the diagnosis,classification,and management of heart failure (HF) over the last three decades[1].Accordingly,HF has been classified into HF with reduced LVEF (HFrEF),HF with midrange or mildly reduced LVEF (HFmrEF),and HF with preserved LVEF (HFpEF) using various,continuously changing LVEF cutoffs.A mandatory prerequisite for the use of this LVEF-based terminology is the definition of the normal LVEF range,which is lacking.From this perspective,we discuss the limitations related to the current LVEF-based classification of HF and provide examples of erroneous conclusions that can be drawn,especially in HF patients at the higher end of the HF spectrum.
The LVEF-based classification of HF was initially applied several decades ago in the clinical trials of neurohormonal inhibitors in which LVEF cutoffs of <35% or 40% were chosen arbitrarily to define patients with HF perceived to be at greatest risk (HFrEF).Several years later,clinical trials with similar agents and endpoints were conducted in patients with HF with an LVEF of ≥ 40%-50% (HFpEF),but they were considered unsuccessful for various reasons[2,3].Recently,another HF phenotype (HFmrEF)was added based on the underrepresentation of patients with HF with an LVEF of 40%-50% in clinical trials.The LVEF cutoffs used for HF classification have varied continuously in the guidelines issued by scientific societies (Figure 1)[4].The 2013 American College of Cardiology Foundation/American Heart Association guidelines defined HFrEF by an LVEF of ≤ 40%,borderline HFpEF by an LVEF of 41%-49%,and HFpEF by an LVEF of ≥ 50%[5].By contrast,the National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand guidelines defined HFrEF and HFpEF by an LVEF of <50% and ≥ 50%,respectively,and did not recognize borderline HFpEF or HFmrEF as a distinct entity[6].Furthermore,in the recent Universal Definition and Classification of Heart Failure[7],which was adopted by the European Society of Cardiology[8],HF classification includes HFrEF with an LVEF of ≤40%,HFmrEF with an LVEF of 41%-49%,and HFpEF with an LVEF of ≥ 50%.Subsequently,another classification of HF was proposed,which defines HFrEF by an LVEF of <40%,HFmrEF by 40% ≤ LVEF
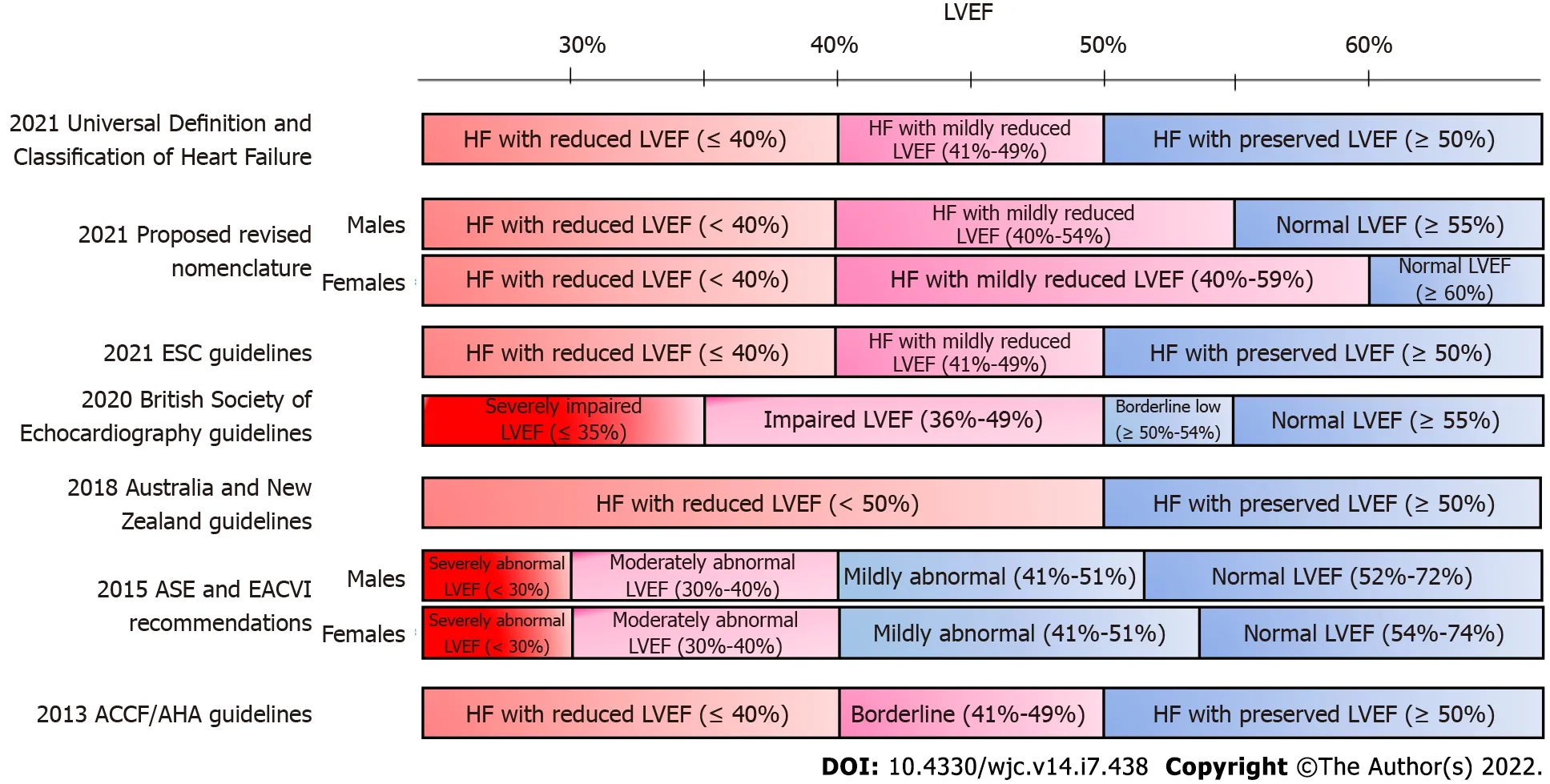
Figure 1 There is significant discordance in the normal values of left ventricular ejection fraction reported by several major scientific societies and associations.

Figure 2 Left ventricular ejection fraction adjusted hazard ratios in patients with heart failure (number of echocardiograms = 40616).

Figure 3 Incident rate of cardiovascular-related mortality.
Therefore,it is not surprising that the LVEF-based classification might lead to erroneous conclusions when interpreting the results of various studies enrolling HF patients at the upper end of the LVEF spectrum (Table 1).A typical example is the recently published Empagliflozin outcome trial in patients with chronic HF with preserved EF (EMPEROR-preserved trial),which reported a benefit with empagliflozin (compared with placebo) in HFpEF defined by an LVEF >40%[15,16] which is different from the 50% cutoff recommended in the Universal Definition and Classification of Heart Failure[7].It is noteworthy that in the EMPEROR-preserved trial,~90% of the patients suffered from hypertension,~49% from diabetes,and ~51% from atrial fibrillation.By contrast,in a study by Luponet al[17],which was used as evidence supporting phenotypic persistence in HFpEF[18],an LVEF cutoff of 50% was used and the patient characteristics were entirely different from those in the EMPEROR-preserved trial with approximately 12% of the participants suffering from hypertrophic cardiomyopathy and 36% from valvular heart disease.Thus,when interpreting these two HFpEF studies,it would be challenging to extrapolate the findings of one to the other.Therefore,no firm conclusions can be drawn regarding the effectiveness of empagliflozin or phenotypic persistence in HFpEF.

Table 1 Heart failure studies including patients with mildly reduced and preserved left ventricular ejection fraction
LVEF-based classification of HF phenotypes has served well over the years.However,HF is such a complex syndrome that no single marker can be used to classify those patients.Accumulating data from recent studies show that markers of contractility such as longitudinal strain[19] and cardiac power[20]outperform the LVEF.The incorporation of artificial intelligence (AI) in diagnostic modalities,outcome predictions,and management of HF (individualized precision medicine) constitutes a major development in the field of cardiovascular medicine.In this regard,developing and validating universally accepted scoring systems based on AI would be a fruitful area of research.The LVEF has been considered the holy grail for HF classification treatment guidance for years.The time for change has come,unless one wants to justify those claiming that most published research findings are false[21].
FOOTNOTES
Author contributions:Xanthopoulos A and Triposkiadis F conceived the study;Xanthopoulos A,Giamouzis G,Skoularigis J,and Triposkiadis F wrote the manuscript;Skoularigis J and Giamouzis G revised the manuscript critically for important intellectual content;All authors provided comments on the manuscript and gave final approval of the version to be published.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Greece
ORCID number:Andrew Xanthopoulos 0000-0002-9439-3946;Grigorios Giamouzis 0000-0002-7406-5427;John Skoularigis 0000-0001-7159-2478;Filippos Triposkiadis 0000-0001-6433-4016.
S-Editor:Zhang H
L-Editor:Filipodia
P-Editor:Zhang H
 World Journal of Cardiology2022年7期
World Journal of Cardiology2022年7期
- World Journal of Cardiology的其它文章
- COVID-19 vaccine-associated myocarditis
- Heart failure in general and cardiac transplant patients with COVID-19
- Is there a window of opportunity to optimize trastuzumab cardiac monitoring?
- Vitamin d deficiency and metabolic syndrome:The joint effect on cardiovascular and all-cause mortality in the United States adults
- National trend of heart failure and other cardiovascular diseases in people living with human immunodeficiency virus
