肺癌合并具有自身免疫特征间质性肺炎的生存分析及预后因素
王榕 刘绍霞 张国俊
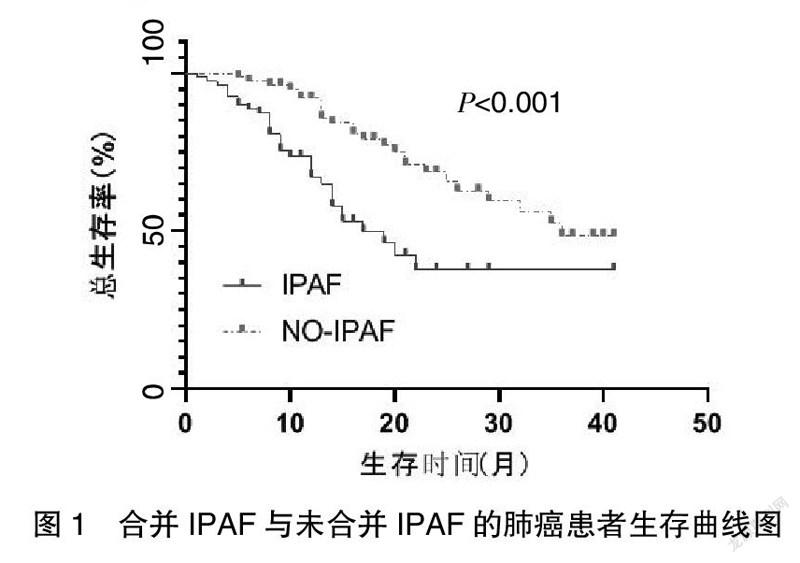

[摘要] 目的 间质性肺炎(ILD)是肺癌(LC)发生的独立危险因素。但具有自身免疫特征的间质性肺炎(IPAF)对肺癌的预后是否有影响尚不明确。本研究旨在探讨IPAF是否影响肺癌的预后。 方法 回顾性收集2018年1月至2020年12月就诊于郑州大学第一附属医院的80例合并IPAF的肺癌患者为研究组,选择80例单纯肺癌患者为对照组,对研究组临床特点及生存时间、预后因素进行观察分析,采用Kaplan-Meier法及log-rank检验和Cox回归模型用以评估不同组的生存差异和死亡风险。 结果 合并IPAF的肺癌患者中的大多数是老年男性吸烟者,研究发现76.3%为男性,63.8%为既往吸烟者。病理类型主要为腺癌(42.5%),与未合并IPAF的LC患者相比,合并IPAF的患者总生存时间更差,差异有统计学意义(17个月vs. 36個月,Log-rank,P<0.001);Cox多因素分析结果显示,IPAF是肺癌患者的独立预后因素(P=0.003);对肺癌合并IPAF的患者进行Cox多因素分析结果提示,肿瘤病理类型、C-反应蛋白是肺癌合并IPAF的独立预后因素(P=0.027;P=0.018)。 结论 与单纯肺癌患者相比,合并IPAF的患者生存期明显缩短。肺癌合并IPAF的治疗具有挑战性,需要谨慎选择抗癌方案。
[关键词] 肺癌;具有自身免疫特征的间质性肺炎;生存分析;预后因素
[中图分类号] R734.2 [文献标识码] B [文章编号] 1673-9701(2022)14-0037-07
Survival analysis of lung cancer complicated with interstitial pneumonia with autoimmune features and its prognostic factors
WANG Rong LIU Shaoxia ZHANG Guojun
Department of Respiratory Medicine,the First Affiliated Hospital of Zhengzhou University,Zhengzhou 450052,China
[Abstract] Objective Interstitial lung disease (ILD) is an independent risk factor for the onset of lung cancer (LC).However,it is not clear whether interstitial pneumonia with autoimmune features (IPAF) has an impact on the prognosis of lung cancer.This paper is intended to discuss whether IPAF affects the prognosis of lung cancer. Methods A total of 80 patients suffering from lung cancer complicated with IPAF treated in the First Affiliated Hospital of Zhengzhou University from January 2018 to December 2020 were retrospectively collected as the study group,and 80 patients with simple lung cancer were selected as the control group. The clinical characteristics, survival time and prognostic factors of the study group were observed and analyzed. Kaplan-Meier method,log-rank test and Cox regression model were used to evaluate the survival difference and death risk of different groups. Results Most of the patients suffering from lung cancer complicated with IPAF were elderly male smokers. Our study found that 76.3% of those patients were male and 63.8% were former smokers. The main pathological type was adenocarcinoma(42.5%). The overall survival time of the LC patients with IPAF was shorter than that of the LC patients without IPAF, and the difference was statistically significant(17 months vs. 36 months,log-rank P<0.001). Cox multivariate analysis results showed that IPAF was an independent prognostic factor in patients with lung cancer(P=0.003).The Cox multivariate analysis for the LC patients with IPAF showed that tumor pathological type and C-reactive protein were independent prognostic factors for lung cancer complicated with IPAF(P=0.027;P=0.018). Conclusion The survival time of the LC patients with IPAF is significantly shorter than that of the patients with simple lung cancer.The treatment of lung cancer complicated with IPAF is challenging, and the anticancer regimen needs to be carefully selected.C73FD96A-1540-4816-9711-45BDBA821030
[Key words] Lung cancer; Interstitial pneumonia with autoimmune features; Survival analysis; Prognostic factors
肺癌(lung cancer,LC)是全世界目前最常见的癌症(占所有癌症诊断的11.6%),也是癌症相关死亡率的主要原因[1]。在中国肺癌是最常见的恶性肿瘤之一[2]。间质性肺炎(interstitial lung disease,ILD)是一组异质性肺病[3],在以往的研究中发现,ILD患者患肺癌的风险增加[4-6]。ILD最常见的病因之一是结缔组织病(connective tissue diseases,CTD),然而,相当一部分继发性ILD患者的临床和实验室特征表明存在自身免疫性疾病,但不符合特定CTD的分类标准[7-8]。2015年,欧洲呼吸学会和美国胸科学会(ERS/ATS)联合会议创造了具有自身免疫特征的间质性肺炎(interstitial pneumonia with autoimmune features,IPAF)一词[9]。此外,有研究人员评估发现LC-ILD患者的预后相比无ILD的LC患者更差[10-12]。上述研究针对LC合并IPAF回顾性分析肺癌合并IPAF的临床特征,评估IPAF对肺癌预后的影响。ILD是LC的主要预后因素,在LC治疗中应予以考虑。需要进一步的研究以确定LC-ILD人群的最佳治疗策略,现报道如下。
1 资料与方法
1.1 一般资料
本研究回顾性收集来自郑州大学第一附属医院2018年1月至2020年12月期间80例确诊为合并IPAF的LC患者作为研究组,80例单纯LC患者为对照组。收集患者的完整临床病历资料,包括患者的性别、年龄、吸烟史等一般情况,实验室检查结果,影像学检查,病理资料。纳入标准:①所有患者均经病理学或细胞学确诊为肺恶性肿瘤,TNM分期参考国际肺癌研究协会第8版标准[13-14]。②具有自身免疫特征间质性肺炎[9](interstitial pneumonia with autoimmune features,IPAF),诊断符合2015欧洲呼吸学会和美国胸科协会(ERS/ATS)公布的分类标准。以下三个领域中任意两个特征的组合的存在:临床领域、由特定的胸外特征组成;血清学,由特定的自身抗体组成;和形态学,由特定的胸部成像、组织病理学或肺部生理特征组成。排除标准(满足任意一条):①患有其他原发恶性肿瘤的患者;②合并慢性阻塞性肺疾病者;③合并心、肝、肾、血液疾病等其他系统严重疾病患者;④患者缺乏完整的病历资料。
1.2 研究结果及随访
本研究随访终止时间为2021年5月,总生存期(overall survival,OS)定义为从肺癌诊断日期至因任何原因引起死亡或最后一次随访时间的时间间隔,以月为单位,随访终止日期仍存活或失访定义为删失。
1.3 观察指标
应用χ2检验对各组间临床特征进行比较,采用电话随訪及门诊进行随访,统计患者生存情况,对患者临床资料如年龄、性别、是否吸烟、肿瘤类型、肿瘤分期、肿瘤大小、实验室指标乳酸脱氢酶(lactic dehydrogenase,LDH)、C-反应蛋白(c-reactive protein,CRP)、癌胚抗原(carcinoembryonic antigen,CEA)、神经元特异性烯醇化酶(lactic dehydrogenase,NSE)、细胞角蛋白19(cytokeratin fragment,CYFRA21-1)进行单因素生存分析,将与预后相关的因素纳入多变量回归模型中进一步分析。
1.4 统计学方法
所有数据均采用SPSS 25.0统计学软件进行分析,计量资料用均数±标准差(x±s)表示,计数资料用[n(%)]表示。组间特征比较计量资料应用t检验,计数资料比较用χ2检验,检验水准α=0.05,Kaplan-Meier法用于生存分析,Log-rank检验比较两组之间的差异。用Cox回归模型进行单因素分析得出有意义的临床病理因素(P<0.10)后,纳入Cox回归模型进行多因素分析。生存曲线使用GraphPad Prism 8.0软件作图。P<0.05为差异有统计学意义。
2 结果
2.1 患者临床特征
本研究纳入80例LC合并IPAF的患者和80例单纯LC患者,基本情况见表1。研究组临床特征:男61例,女19例;平均年龄(68.00±7.46)岁,≥65岁54例,<65岁26例。患者主要症状为咳嗽(70%)和胸闷(47.5%)。既往有吸烟史的患者51例(63.7%),无吸烟史29例(36.3%);临床分期Ⅰ~Ⅱ期者20例,Ⅲ期者24例,Ⅳ期者36例,最常见的病理类型为腺癌占42.5%,鳞癌占40%,小细胞癌占17.5%。37例(46.2%)占位位于上肺叶,38例(47.5%)位于下肺叶,5例(6.3%)位于中肺叶。大多数患者最初的肿瘤治疗方案主要为化疗(77.5%),早期患者更倾向选择手术。
2.2 患者生存时间
LC合并IPAF患者的中位总生存时间(OS)为17个月(95%CI:11.457~22.453),单纯LC患者的中位OS为36个月,全部LC患者的中位OS为29个月,对两组进行比较,是否合并IPAF的OS比较,差异有统计学意义(Log-rank,P<0.001)。见图1。
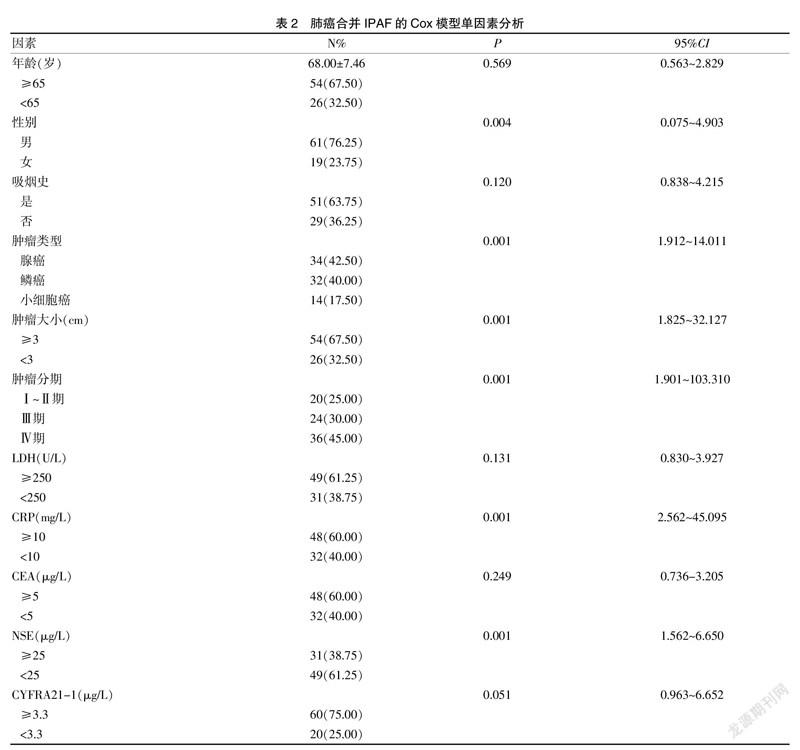
2.3 影响LC合并IPAF患者OS的预后因素分析
纳入分析LC合并IPAF的预后因素主要有:性别、年龄、病理类型、肿瘤大小、肿瘤分期以及实验室指标乳酸脱氢酶(LDH)、C-反应蛋白(CRP)、癌胚抗原(CEA)、神经元特异性烯醇化酶(NSE)、细胞角蛋白19(CYFRA21-1)。见表2。同时将单因素分析结果P<0.10(年龄、病理类型、肿瘤大小、肿瘤分期、吸烟、CRP、NSE)纳入多变量回归模型中进一步分析,同时将预后作为因变量,存活=1,死亡=2,单因素分析有意义的项目作为自变量进行赋值。见表3。结果显示,肿瘤病理类型、CRP是LC合并IPAF的独立预后因素(P=0.027,95%CI=1.62~23.62;P=0.018,95%CI=1.36~26.83),差异有统计学意义(P<0.05)。见表4。C73FD96A-1540-4816-9711-45BDBA821030
2.4 LC患者预后因素分析
影响肺癌患者的预后因素有:性别、年龄、吸烟、病理类型、肿瘤大小、肿瘤分期、是否合并IPAF及实验室指标CRP、LDH、CEA、NSE、CYFRA21-1,单因素分析结果显示,两组有差异的包括(P<0.10):肿瘤病理类型、肿瘤大小、肿瘤分期、是否合并IPAF及实验室指标CRP、LDH、CEA、NSE、CYFRA21-1。见表5。将预后作为因变量,存活=1,死亡=2,单因素分析中预后相关的因素作为自变量进行赋值。见表6。在Cox多因素分析中,是否合并IPAF是LC患者的独立预后因素,差异有统计学意义(P<0.05)。见表7。
3 讨论
目前对ILD-LC的治疗和预后的描述主要集中于结缔组织相关性间质性肺炎(CTD-ILD)、特发性肺间质纤维化(IPF)的肺癌患者的回顾性研究,IPAF诊断标准提出后,陆续有文献报道IPAF的回顾性临床研究[15-17],为IPAF诊断纳入ILD诊断分类提供充分的验证[18]。Guo等[19]的研究发现,IPF是ILD最常见的亚组,其次是IPAF和CTD-ILD。而对于LC合并IPAF的研究不够充分且有限。在此,本研究对80例LC合并IPAF的患者进行回顾性研究,旨在了解LC合并IPAF患者的临床特征,预后因素及生存。
本研究表明,与单纯LC患者相比,LC合并IPAF患者的生存率较低,中位生存期分别为17个月和36个月,Tzuvelekis等[20]最近报道,自LC诊断之日起,LC合并IPF患者的中位生存期为14个月。Alomaish等[12]报道LC合并ILD患者与单纯LC的中位生存期分别为15个月和59个月。先前关于LC合并ILD的研究(大多数研究集中于IPF及CTD-ILD的患者)也表明,与单纯肺癌相比,肺癌和ILD患者的生存率较低,死亡率较高。
先前大量关于LC合并ILD的研究[11,21-26]表明这些患者中的大多數是老年男性吸烟者,本研究发现76.3%为男性,63.8%为既往吸烟者。病理类型主要为腺癌(42.5%),与其他发现腺癌(56%)为常见类型的研究相比可发现类似分布。大部分患者确诊时已经有转移,选择的主要治疗方式为化疗[27]。对LC合并IPAF的患者进行多因素分析,分析提示肿瘤类型、CRP是独立预后因素。Olszewski等[28]研究提出与腺癌相比,患有鳞状细胞癌的LC患者的生存率(无论是否伴有ILD)更差。同时有文献报道小细胞癌合并ILD患者的生存率比腺癌合并ILD患者差[12]。近期Ueno等[29]发现血清CRP水平是预测ILD急性加重发生率的独立决定因素。无论肺癌的治疗有多有效,一旦先前存在的间质性肺炎发生急性加重,患者的死亡率将很高[30]。这项研究有几个局限性。首先,这项研究是在单中心进行的回顾性分析,可能导致了选择偏差。其次DLCO是评估ILD的重要指标,而肺功能检测缺失数据>20%,未能纳入研究。在肺癌合并ILD的情况下,抗肿瘤治疗后经常发生急性恶化。这提示在治疗选择上需要谨慎。在大多数临床试验中,伴有ILD的LC患者被排除在外,因此,关于这些患者预后的资料很少。未来需要更多的临床试验为患者提供安全有效的治疗方案。
[参考文献]
[1] Bray F,Ferlay J,Soerjomataram I,et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J].CA Cancer J Clin,2018,68(6):394-424.
[2] 郑荣寿,孙可欣,张思维,等.2015年中国恶性肿瘤流行情况分析[J]中华肿瘤杂志,2019(1):19-28.
[3] Duchemann B,annesi-Maesano I,Jacobe-de-Naurois C,et al. Prevalence and incidence of interstitial lung diseases in a multi-ethnic county of greater Paris[J].Eur Respir J,2017,50(2):1 602 419.
[4] Kato E,Takayanagi N,Takaku Y,et al. Incidence and predictive factors of lung cancer in patients with idiopathic pulmonary fibrosis[J].ERJ Open Res,2018,4(1):111-116.
[5] Naccache JM,Gibiot Q,Monnet I,et al.Lung cancer and interstitial lung disease:A literature review[J].J Thorac Dis,2018,10(6):3829-3844.
[6] Whittaker Brown SA,Padilla M,Mhango G,et al. Interstitial lung abnormalities and lung cancer risk in the national lung screening trial[J].Chest,2019,156(6):1195-1203.
[7] Alevizos MK,Giles JT,Patel NM,et al. Risk of progression of interstitial pneumonia with autoimmune features to a systemic autoimmune rheumatic disease[J].Rheumatology (Oxford),2020,59(6):1233-1240.C73FD96A-1540-4816-9711-45BDBA821030
[8] Lee CT,Oldham JM.Interstitial pneumonia with autoimmune features: Overview of proposed criteria and recent cohort characterization[J].Clin Pulm Med,2017,24(5):191-196.
[9] Fischer A,Antoniou KM,Brown KK,et al. An official European respiratory society/American thoracic society research statement:Interstitial pneumonia with autoimmune features[J].Eur Respir J,2015,46(4):976-987.
[10] Kinoshita T,Azuma K,Sasada T,et al. Chemotherapy for non-small cell lung cancer complicated by idiopathic interstitial pneumonia[J].Oncol Lett,2012,4(3):477-482.
[11] Sato T,Watanabe A,Kondo H,et al.Long-term results and predictors of survival after surgical resection of patients with lung cancer and interstitial lung diseases[J].J Thorac Cardiovasc Surg,2015,149(1): 64-69.
[12] Alomaish H,Ung Y,Wang S,et al. Survival analysis in lung cancer patients with interstitial lung disease[J].PLoS One,2021,16(9): e0255 375.
[13] Travis WD,Asamura H,Bankier AA,et al.The IASLC lung cancer staging project:Proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer[J].J Thorac Oncol, 2016,11(8):1204-1223.
[14] Asamura H,Chansky K,Crowley J,et al. The international association for the study of lung cancer staging project: Proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM classification for lung cancer[J].J Thorac Oncol,2015,10(12):1675-1684.
[15] Chartrand S,Swigris JJ,Stanchev L,et al. Clinical features and natural history of interstitial pneumonia with autoimmune features:A single center experience[J].Respir Med,2016,119:150-154.
[16] Ferri C,Manfredi A,Sebastiani M,et al. Interstitial pneumonia with autoimmune features and undifferentiated connective tissue disease: Our interdisciplinary rheumatology-pneumology experience, and review of the literature [J].Autoimmun Rev,2016,15(1):61-70.
[17] Oldham JM,Adegunsoye A,Valenzi E,et al. Characterisation of patients with interstitial pneumonia with autoimmune features[J].Eur Respir J, 2016,47(6):1767-1775.
[18] Luppi F,Wells AU.Interstitial pneumonitis with autoimmune features (IPAF):A work in progress[J].Eur Respir J,2016,47(6):1622-1624.
[19] Guo B,Wang L,Xia S,et al.The interstitial lung disease spectrum under a uniform diagnostic algorithm:A retros-pective study of 1945 individuals [J].J Thorac Dis,2020,12 (7):3688-3696.C73FD96A-1540-4816-9711-45BDBA821030
[20] Tzouvelekis A,Karampitsakos T,Gomatou G,et al. Lung cancer in patients with idiopathic pulmonary fibrosis.A retrospective multicenter study in Greece[J].Pulm Pharmacol Ther,2020,60:101 880.
[21] Yoon JH,Nouraie M,Chen X,et al. Characteristics of lung cancer among patients with idiopathic pulmonary fibrosis and interstitial lung disease-analysis of institutional and population data[J].Respir Res,2018,19(1): 195.
[22] Tomassetti S,Gurioli C,Ryu JH,et al. The impact of lung cancer on survival of idiopathic pulmonary fibrosis[J].Chest,2015,147(1):157-164.
[23] Zhang M,Yoshizawa A,Kawakami S,et al.The histological characteristics and clinical outcomes of lung cancer in patients with combined pulmonary fibrosis and emphysema[J].Cancer Med,2016,5(10):2721-2730.
[24] Otsuka H,Sugino K,Hata Y,et al. Clinical features and outcomes of patients with lung cancer as well as combined pulmonary fibrosis and emphysema[J].Mol Clin Oncol,2016,5(3):273-278.
[25] Lee T,Park JY,Lee HY,et al. Lung cancer in patients with idiopathic pulmonary fibrosis:Clinical characteristics and impact on survival [J].Respir Med,2014,108(10):1549-1555.
[26] Jafarinezhad A,Yektakooshali MH.Lung cancer in idiopathic pulmonary fibrosis:A systematic review and meta-analysis[J].PLoS One,2018,13(8): e0202 360.
[27] Barczi E,Nagy T,Starobinski L,et al.Impact of interstitial lung disease and simultaneous lung cancer on therapeutic possibilities and survival [J].Thorac Cancer,2020,11(7):1911-1917.
[28] Olszewski AJ,Ali S,Witherby SM. Disparate survival trends in histologic subtypes of metastatic non-small cell lung cancer:A population-based analysis[J].American Journal of Cancer Research,2015,5(7):2229-2240.
[29] Ueno F,Kitaguchi Y,Shiina T,et al. The interstitial lung disease-gender-age-physiology index can predict the prognosis in surgically resected patients with interstitial lung disease and concomitant lung cancer[J].Respiration,2020,99(1):9-18.
[30] Ikeda S,Kato T,Kenmotsu H,et al. Current treatment strategies for non-small-cell lung cancer with comorbid interstitial pneumonia[J].Journal of Thoracic Oncology,2021, 13(16): 3979.
(收稿日期:2021-11-18)C73FD96A-1540-4816-9711-45BDBA821030