Efficacy and safety of traditional Chinese medicine in the treatment of coronary heart disease complicated with anxiety and/or depression after PCI: A systematic review and meta-analysis
Qian Liu, Hai-Yan Wang, Hai-Tao Xie, Xiao-Hu Chen
1. Nanjing University of Chinese Medicine, Nanjing 210023, China
2. Affiliated Hospital of Nanjing University of traditional Chinese Medicine, Nanjing 210029, China
ABSTRACT Objective: The clinical efficacy and safety of traditional Chinese medicine in the treatment of anxiety and/or depression after PCI for coronary heart disease were systematically evaluated.Methods: The databases of CNKI, Wanfang, VIP, CMB, PubMed, Web of Science, PubMed,Web of Science and Cochrane Library were searched by computer, and the Chinese and English randomized controlled trials(RCTs)of traditional Chinese medicine in the treatment of anxiety and/or depression after PCI of coronary heart disease published from the database to November 2020 were included. The Cochrane bias risk tool and the modified Jadad scale were used to evaluate the quality of the included literature, and the RevMan 5.3 and Stata 16.0 software were used for Meta-analysis. Results: A total of 23 RCTs were included, including 1837 subjects, including 917 cases in the treatment group of traditional Chinese medicine, 920 cases in the control group, the baseline situation between groups was consistent, comparable.Meta-analysis results show that TCM treatment improves the total clinical effective rate[OR=2.34,95%CI(1.61,3.40),P<0.00001],and the efficacy of TCM syndrome[OR=5.19,9 5%CI(2.74,9.86),P<0.00001],reduce Hamilton anxiety scale HAMA score[SMD=-0.96,95%CI(-1.78,-0.14),P=0.02],Hamilton Depression Scale HAMD score[SMD=-1.10,95% CI(-1.79,-0.41),P=0.002],SAS self-rating scale score[SMD=-1.20,95% CI(-1.75,-0.65),P<0.0001],SDS self-rating scale score[SMD=-1.14,95% CI(-1.62,-0.65),P<0.00001] and other indicators are better than the control group, and the difference is statistically significant (P<0.05).Conclusion: The combination of traditional Chinese medicine intervention and conventional western medicine treatment after PCI can further improve the clinical efficacy of patients with anxiety and/or depression after PCI of coronary heart disease and has good safety. Due to the general quality of the literature included in this study, the above conclusions need to be further confirmed by high-quality randomized controlled double-blind clinical trials.
Keywords:Traditional Chinese medicine PCI after coronary heart disease Anxiety Depression Meta-analysis
1. Introduction
Coronary atherosclerotic heart disease refers to coronary artery atherosclerosis caused by luminal stenosis or occlusion, resulting in myocardial ischemia and hypoxia or necrosis caused by heart disease, referred to as coronary heart disease, also known as ischemic heart disease[1].Interventional therapy, drug therapy and surgical treatment are known as the three means of coronary heart disease treatment. In September 1977, Gruentzig carried out the first percutaneous coronary angioplasty in the world, creating a new historical era of interventional cardiology. At present, PCI treatment is still one of the preferred treatment methods after the diagnosis of coronary heart disease, which is of great significance in reducing the mortality of patients. However, PCI is not the end point of coronary heart disease treatment, the biological process of atherosclerosis in patients after PCI has not stopped, and often accompanied by anxiety and/or depression and other psychological disorders. The study found that[2] After PCI, 46.10%of patients with anxiety,36.09%of patients with depression, and 23.77%of patients with anxiety and depression, which not only affects the rehabilitation of patients after surgery, but also makes patients with poor compliance and poor prognosis, resulting in a series of cardiovascular events.
Therefore, how to effectively prevent and treat mental and psychological disorders such as anxiety and/or depression after PCI in coronary heart disease has become a research hotspot in the cardiovascular field. At present, many clinical studies have reported that traditional Chinese medicine has good clinical efficacy in the treatment of coronary heart disease complicated with anxiety and/or depression after PCI. However, due to the small sample size of single study, it is difficult to provide strong support for the evaluation of its clinical efficacy. Therefore, this study refers to the PRISMA statement, analyzes and evaluates the methodological quality of published Chinese and English literature according to the requirements of Cochrane systematic evaluation, systematically evaluates the effectiveness and safety of traditional Chinese medicine in the treatment of coronary heart disease complicated with anxiety and/or depression after PCI, and provides a reliable basis for traditional Chinese medicine intervention.
2. Data and methods
2.1 Inclusion criteria
2.1.1 Research types
Clinical randomized controlled trials (RCT).
2.1.2 Research objects
The diagnosis of coronary heart disease referred to Guidelines for diagnosis and treatment of chronic stable angina[3], Guideline for diagnosis and treatment of unstable angina (UA) and non-ST segment elevation myocardial infarction[4] and Guidelines for diagnosis and treatment of acute ST-segment elevation myocardial infarction[5].Hamilton Anxiety Scale (HAMA), Depression Scale(HAMD), Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS)were used to evaluate the severity of anxiety and/or depression.
2.1.3 Intervention measures
In addition to conventional western medicine treatment after PCIfor coronary heart disease, the control group was treated with blank control or combined with western medicine anti-anxiety and depression drugs, while the treatment group was treated with Chinese medicine, including Chinese medicine decoction, Chinese medicine ointment, Chinese patent medicine, or combined with western medicine anti-anxiety and depression drugs.
2.2 Exclusion criteria
①Non-clinical randomized controlled trials;②animal experiments,case reports, pharmacological studies, experience, case reports,reviews, conference literature, etc.③literature with incomplete or wrong data;④Patients with other serious diseases, such as heart failure, severe liver, brain and kidney diseases.⑤ repeated research;⑥Literatures with other diagnostic criteria or outcome indicators that were not concerned in this study.
2.3 Outcome indicators
Efficacy indicators include:①Clinical total effective rate;②HAMA scale score;③HAMD scale score;④SAS self-rating scale score;⑤SDS self-rating scale score;⑥TCM syndrome curative effect.
Safety indicators:adverse reactions, including the treatment group,the control group after the occurrence of adverse events recorded.
2.4 Literature retrieval strategy
CNKI, WanFang, VIP, CBM, PubMed, Web of Science, The Cochrane Library were searched from inception to November 2020.The search strategy of subject joint free words is adopted.Literature search terms:Chinese:coronary heart disease, coronary atherosclerotic heart disease, ischemic heart disease, angina pectoris,myocardial infarction, myocardial infarction, myocardial infarction,ACS, acute coronary syndrome, anxiety, depression, anxiety and depression, PCI, percutaneous coronary intervention, percutaneous coronary stent implantation, drug-eluting stent, randomized controlled, randomized controlled, RCT, Chinese medicine, Chinese medicine. English:Coronary heart disease、coronary atherosclerotic heart disease、ischemic heart disease、angina pectoris、myocardial infarction、myocardial infarction、myocardial infarction、ACS、acute coronary syndrome、Anxiety、depression、anxiety depression、PCI、percutaneous coronary intervention 、percutaneous coronary stent implantation、 drug-eluting stent、Randomized controlled、randomized、RCT、chinese medicine、traditional Chinese medicine、Traditional Chinese Medicine.
2.5 Literature screening and data extraction
Two researchers independently screened and retrieved the literature according to the inclusion and exclusion criteria specified in this study.They used Note Express literature management software and office software Excel to create data extraction tables, manage and extract research data and cross-check them.If the same experiment was reported many times by different literature, one of the most detailed reports was included.When the opinions are divided,the two sides agree, if the opinions are not unified, discuss with the third person.Data extraction included the first author's name,publication years, sample size, gender, age, interventions, course of treatment, outcome indicators and adverse reactions.Data extraction inconsistencies check the original literature, or discuss solutions, if necessary contact the author of the literature.
2.6 Quality evaluation
The Cochrane Collaboration Network bias risk assessment tool was used as the standard to evaluate the methodological quality of each study from seven aspects:random sequence generation,allocation concealment, blind method for researchers and subjects,blind method for evaluation of research results, integrity of outcome data, selective reporting of research results, and other bias.The methodological quality of each study was evaluated, which was divided into three levels risk', 'unclear', and 'high risk'.The evaluation was supplemented by the improved Jadad quality score method.[6]Among them, 1-3 was divided into low quality research, and 4-7 was divided into high quality research.
2.7 Statistical analysis
RevMan 5.3 and Stata 16.0 softwares were used for Metaanalysis of all data.Ratio ratio (OR) was used as the effect analysis statistic for binary variables, and standardized mean difference(SMD) was used as the effect index for continuous variables.The 95%confidence interval (CI) was calculated for both variables.The heterogeneity between the results was tested by X2 test.If there was no heterogeneity between groups (P≥0.10 and I2≤50%), it was considered that the heterogeneity between studies was small, and the fixed effect model was used for Meta analysis.On the contrary (P<0.10, I2>50%), the random effect model was selected and the sensitivity analysis was carried out to find the source of heterogeneity.Subgroup analysis or Meta regression analysis were performed on the factors that may lead to heterogeneity.If the heterogeneity is too obvious, especially the obvious clinical heterogeneity, and the data cannot be merged, descriptive analysis was used to explain the results of the study.In addition, if more than 10 articles were included in a certain outcome index, the inverted funnel plot was used to visually judge, and then the Begg rank correlation test and Egger linear regression were used to analyze the potential publication bias.If P>0.05, the risk of publication bias was small, and vice versa.
3. Results
3.1 Results of the literature search
A total of 261 relevant literatures were retrieved, 58 repetitive literatures were excluded by Note Express literature management software, 2 reviews and 1 systematic review were excluded, 168 literatures with inconsistent research contents, inconsistent control measures and intervention measures were excluded after reading the summary, 4 literatures with inconsistent non-randomized controlled trials and research methods were excluded, 3 literatures with inconsistent outcome indicators and 2 literatures with low quality were excluded after reading the full text, and 23 randomized controlled trials were finally included.The specific screening process is shown in Figure 1.
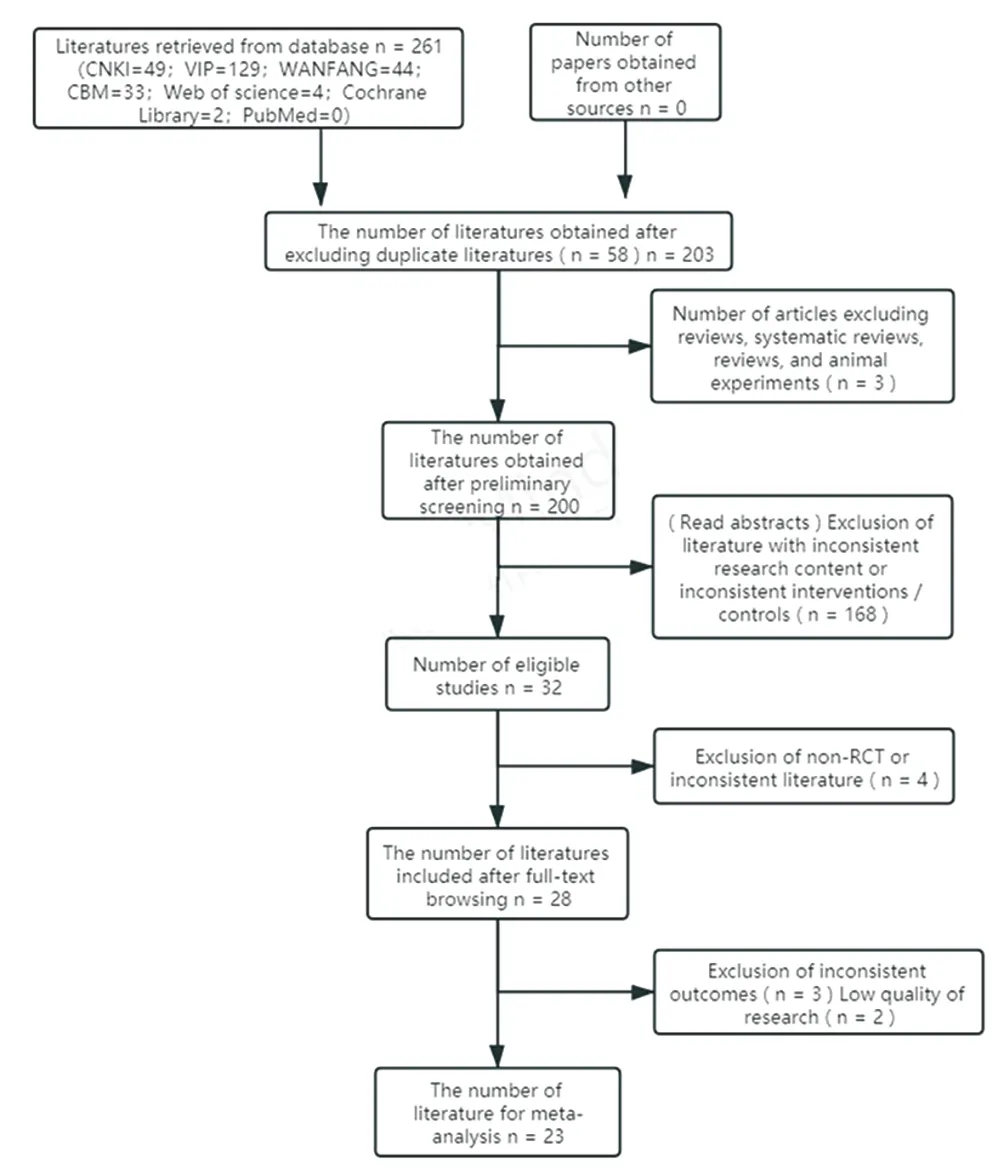
Figure 1 Literature screening process
3.2 Basic characteristics of included literature
A total of 23 randomized controlled trials[7-29] were included,including 1837 subjects, including 917 cases in the TCM treatment group and 920 cases in the control group.The study group had good inter-specific balance and comparability.In terms of intervention measures, in addition to postoperative conventional western medicine treatment, 14 articles[7, 8, 10, 12, 14, 15, 17, 18, 21, 23, 25-28]were combined with Deanxit, 7 articles[11, 13, 19, 20, 22, 24, 29]were blank control, and 2 articles[21, 28] were combined with Deanxit on the basis of traditional Chinese medicine treatment.In terms of adverse reactions, two literature[12, 17] clearly described no obvious adverse reactions, and 17 literature[7-11, 13, 15, 18-20, 22-26, 28, 29] did not describe whether adverse reactions occurred.Four studies[14, 16,21, 27] reported the adverse reactions in detail.In addition, the Jadad scale score of 8 articles[9, 13, 14, 1 7, 20, 22-24] was 4 points, and the scores of other articles were 3 points, as shown in table 1.

Table 1 Basic characteristics of included literature
3.3 Quality assessment of included literature
3.3.1 Generation of random sequences
Of the 23 included literatures, all referred to the word'random', 8 of which were evaluated as'low risk'by random number table method[9,13, 14, 17, 20, 22-24]; The remaining 15 articles only referred to random grouping[7, 8, 10-12, 15, 16, 18, 19, 21, 25-29], and the specific random method was not described.For some authors who could query the contact mode, the research methods used in the above literature were still not clear after sending e-mail queries, and the evaluation was'unclear'.
3.3.2 Implementation of allocation concealment
None of the 23 literatures mentioned the allocation scheme hiding method, which belongs to'unclear'.
3.3.3 Blind method for researchers and subjects
Of the 23 included literatures, only one literature11 implemented'single blind method', but did not specify the implementation process of blind method.The remaining 22 articles did not refer to the implementation of the blinding method[7-10, 12-29].Taking into account the non-use of placebos and the differences between Chinese and Western dosage forms, it was considered that the possibility of blinding was not high and all were evaluated as'high risk'.
3.3.4 Outcome blind evaluation
None of the 23 articles reported blinding research outcomes, which were evaluated as'unclear.'
3.3.5 Integrity of outcome data
One literature reported the loss of follow-up or fall-off of 5 patients16.Among them, 3 patients in the control group fell off due to the adverse reactions of nausea and headache in the first week of medication, and 2 patients in the observation group fell off automatically without timely follow-up, which was evaluated as 'high risk'.One literature reported 5 patients lost to follow-up19,including 3 cases in the treatment group and 2 cases in the control group.The specific reasons were not explained and evaluated as'high risk'.The remaining 21 articles were evaluated as'low risk'without loss of follow-up or withdrawal from the study.
3.3.6 Results of selective reporting
All 23 articles reported pre-set outcome indicators, which were evaluated as'low risk'.
3.3.7 Other sources of bias
None of the 23 articles described other biases as'low risk'.The bias risk assessment results are shown in Figure 2.
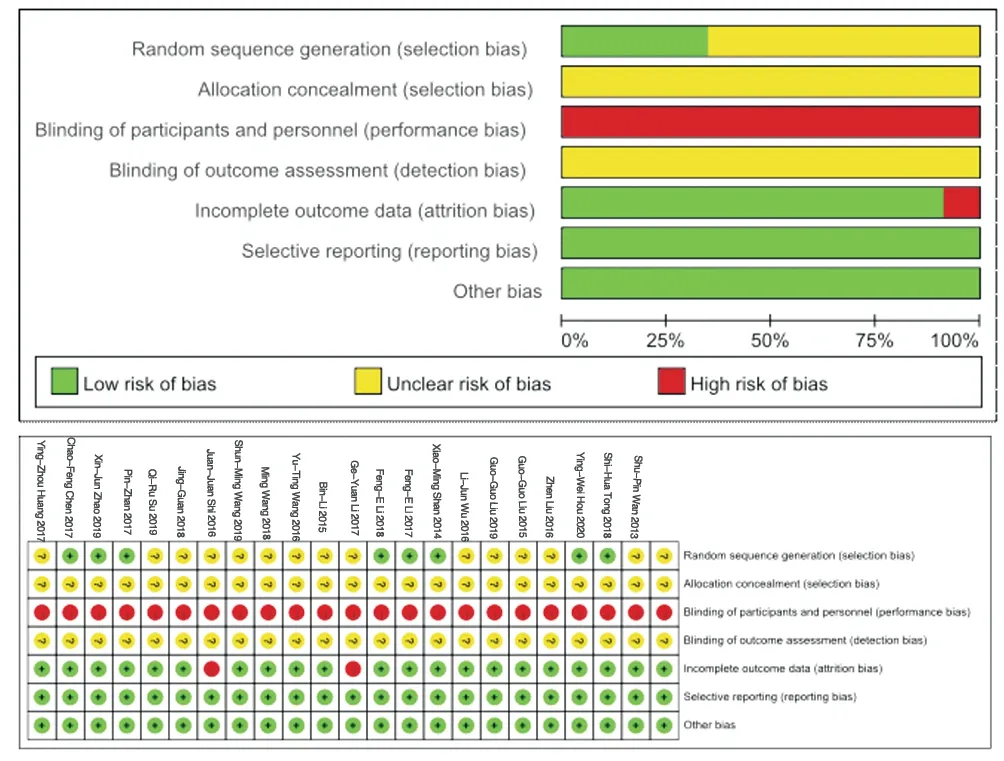
Figure 2 Quality evaluation of included studies
3.4 Meta-analysis results
3.4.1 Total clinical effective rate
12 studies[7, 9, 10, 12, 14, 17, 18, 24-28] (1062 patients) reported the total clinical effective rate, and there was no statistical heterogeneity among the studies (P=0.621, I2=0 %).The fixed effect model was used.Meta-analysis results showed that the total clinical effectiverate of traditional Chinese medicine combined with conventional western medicine after surgery was significantly higher than that of the control group[OR=2.34, 95%CI(1.61, 3.40)], and the difference between the two groups was statistically significant (P<0.00001), as shown in Figure 3 :
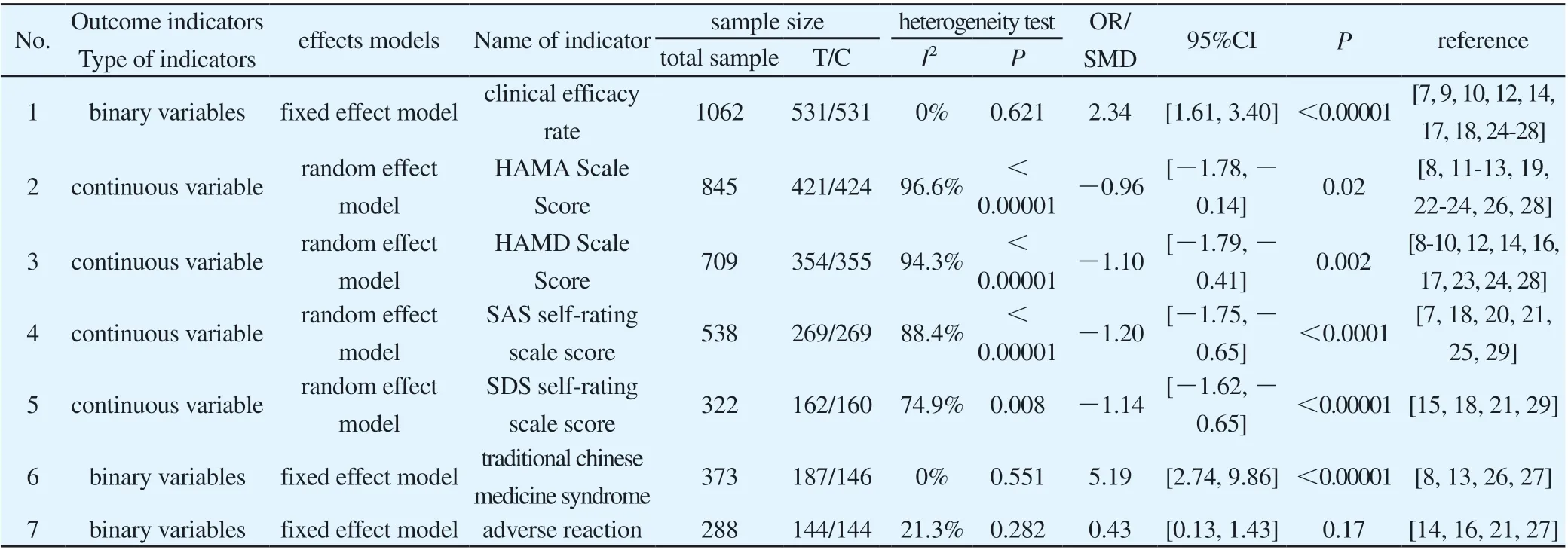
Table 2 Comparison of clinical outcome indexes between groups

Figure 3 Meta-analysis of total clinical effectiveness
3.4.2 HAMA scale score
10 studies[8, 11-13, 19, 22-24, 26, 28](845 patients) evaluated the improvement of anxiety by comparing the HAMA scores at the end of treatment between the two groups.The heterogeneity test showed that the heterogeneity between the studies was high (P<0.00001,I2=96.6 %).Therefore, the random effect model was selected.The results of Meta-analysis showed that the HAMA score in the treatment group was lower than that in the control group, and the difference was statistically significant[SMD=− 0.96, 95%CI(− 1.78,− 0.14), P=0.02], suggesting that the addition of traditional Chinese medicine on the basis of routine western medicine treatment after PCIcan further reduce the HAMA score of patients with anxiety after PCIof coronary heart disease.As shown in Figure 4 :
Figure 4 Meta analysis of HAMA scale score
3.4.3 HAMD scale score
10 studies[8-10, 12, 14, 16, 17, 23, 24, 28] (709 patients) evaluated the improvement of depression by comparing the HAMD scores at the end of treatment between the two groups.Heterogeneity test showed that the heterogeneity between the studies was high (P<0.00001,I2=98 %).Therefore, the random effect model was selected.The results of Meta-analysis showed that the HAMD score of the treatment group was lower than that of the control group, and the difference was statistically significant[SMD=-1.10, 95%CI(-1.79,-0.41), P=0.002].It was suggested that the addition of traditional Chinese medicine on the basis of routine western medicine after PCIcould further reduce the HAMD score of patients with coronary heart disease complicated with depression.As shown in Figure 5 :3.4.4 SAS self-rating scale score

Figure 5 Meta analysis of HAMD scale score
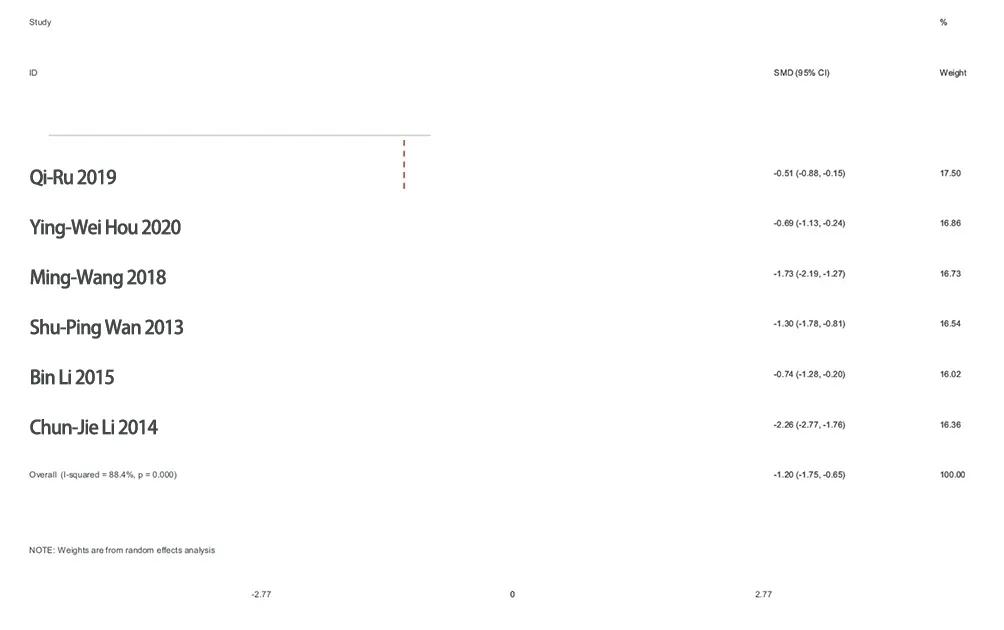
Figure 6 Meta-analysis of SAS self-rating scale score
3.4.5 SDS self-rating scale score
4 studies[15, 18, 21, 29](322 patients) evaluated the improvement of anxiety by comparing the SDS scores at the end of treatment between the two groups.Heterogeneity test showed that the heterogeneity between the studies was high (P=0.008, I2=74.9 %).Therefore, a random effect model was selected.Meta-analysis showed that the SDS score of the treatment group was lower than that of the control group, and the difference was statistically significant[SMD=-1.14,95%CI(-1.62, -0.65), P<0.00001].It is suggested that the addition of traditional Chinese medicine on the basis of routine western medicine can further reduce the SDS score of patients with coronary heart disease complicated with depression after PCI, as shown in Figure 7 :
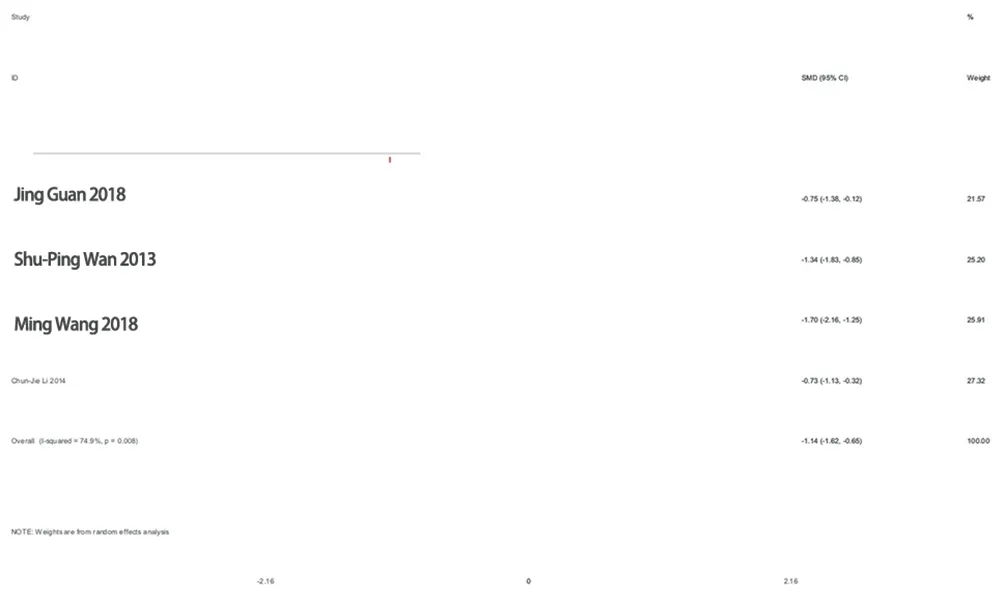
Figure 7 Meta-analysis of SDS self-rating scale score
3.4.6 Curative effect of TCM syndromes
4 studies[8, 13, 26, 27] (373 patients) evaluated the efficacy of TCM syndromes, and there was no statistical heterogeneity among studies(P=0.551, I2=0 %).Using a fixed effect model, Meta-analysis showed that the efficacy of TCM syndromes in the treatment group was significantly higher than that in the control group, and the difference was statistically significant[OR=5.19, 95%CI(2.74,9.86), P<0.00001], indicating that TCM treatment can significantly improve the efficacy of TCM syndromes in patients with anxiety and/or depression after PCI, as shown in Figure 8 :
Figure 8 Meta-analysis of the curative effect of TCM syndromes
3.4.7 Safety evaluation
Among the 23 RCTs included, 4 studies[14, 16, 21, 27] reported adverse reactions in patients (Table 3), and Li14 reported 2 cases of obvious dry mouth and 1 case of constipation in the control group;Shi16 reported that there were 3 cases of nausea and headache in the control group, and Wan21 reported that there were 2 cases of epigastric distention and pain in the treatment group, with a slight degree, and the symptoms disappeared after the addition of gastric mucosal protective agent.Liu27 reported one case of nausea in the control group;Meta-analysis (Fig.9) was performed.A total of 288 patients were included, and each group had homogeneity(P=0.282, I2=21.3 %).The fixed effect model was used for analysis.The results showed that there was no significant difference in the incidence of adverse reactions between the treatment group and the control group[OR=0.43, 95%CI(0.13, 1.43), P=0.17].Therefore, the incidence of adverse reactions between the treatment group and the control group was not clear.Therefore, it is necessary to pay attention to the occurrence of adverse reactions in the process of using traditional Chinese medicine.

Figure 9 Meta-analysis of adverse reactions
3.5 Sensitivity analysis
Chinese medicine treatment of coronary heart disease after PCIwith anxiety and/or depression in reducing HAMA score, HAMD score,SAS score, SDS score of Meta-analysis heterogeneity were I2=95%, I2=98 %, I2=93 %, I2=92 %, suggesting that the heterogeneity is large, excluding independent studies in turn, the remaining studies were re-analyzed, all the results of the point estimates fell in the combined effect of 95%CI(Figure 10, 11, 12, 13), indicating that the overall stability of the results of this study is good.
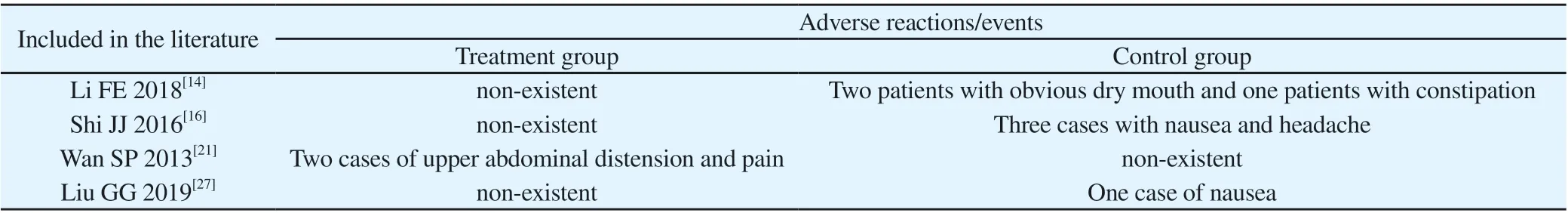
Table 3 Security judgement
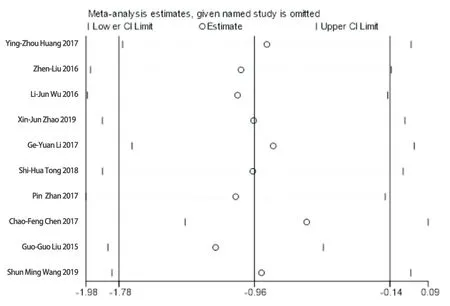
Figure 10 Sensitivity analysis of HAMA score
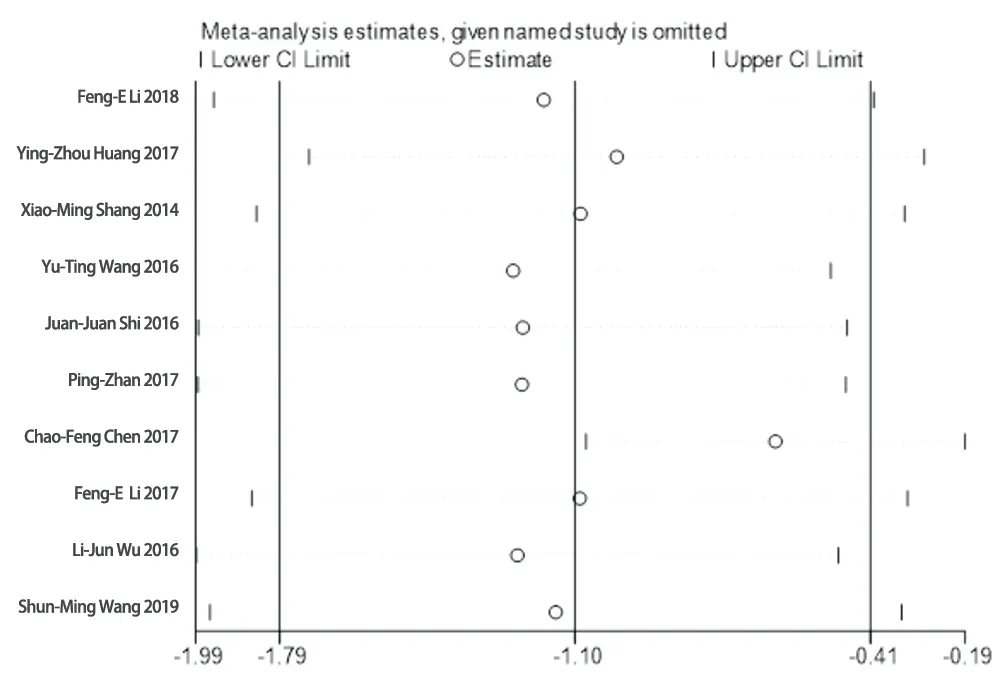
Figure 11 Sensitivity analysis of HAMD score
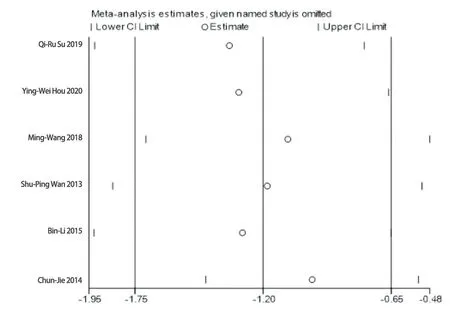
Figure 12 Sensitivity analysis of SAS score
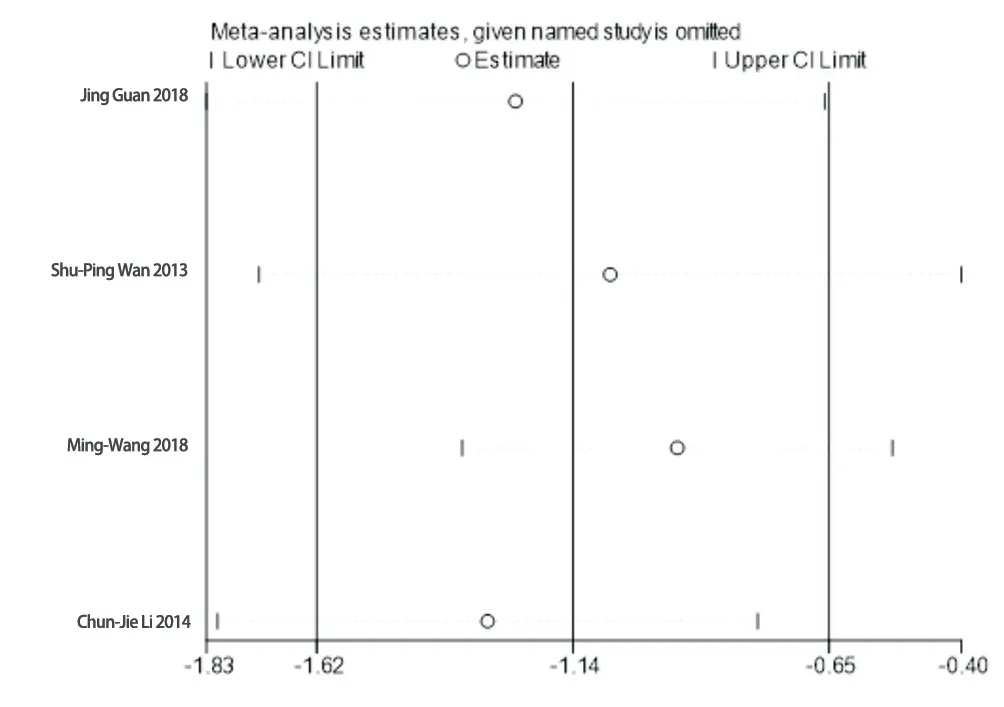
Figure 13 Sensitivity analysis of SDS score
After attempting to conduct subgroup analysis, the source of heterogeneity is still not found, which is considered to be related to the following factors:
(1) Cognitive behavioral therapy, systemic desensitization therapy, Morita therapy, biofeedback therapy, dietetic recuperation,psychological and exercise therapy and other non-drug therapy also play a crucial role in the treatment of anxiety and depression, but the 23 literatures involved in this paper did not mention whether non-drug therapy was used to intervene in patients, considering heterogeneity may come from this;
(2) The inclusion criteria are indefinite for the western medicine classification of coronary heart disease, TCM syndrome type,the severity of anxiety and/or depression, and the limitation of postoperative western medicine intervention is also relatively broad.There are differences in the treatment cycle and dosage of each independent literature, which reduces the external authenticity of the conclusions of this study and affects the reliability of the results.
3.6 Publication bias analysis
In this study, the OR value was used as the abscissa, and the logarithmic standard error SE (log OR) of OR value was used as the ordinate.According to the data of 12 studies[7, 9, 10, 12, 14, 17, 18, 24-28]with the total clinical effective rate as the outcome index, the funnel plot was drawn (Fig.14).The results showed that the corresponding scatter points in each literature were within the confidence interval,and the funnel plot was roughly symmetrical.The Begg rank correlation test (Fig.15A) was used, and the results showed that P=0.086>0.05, and P=0.127>0.05 obtained by the Egger linear regression method (Fig.15B).Both qualitative and quantitative tests suggested that there was no obvious publication bias in this study.
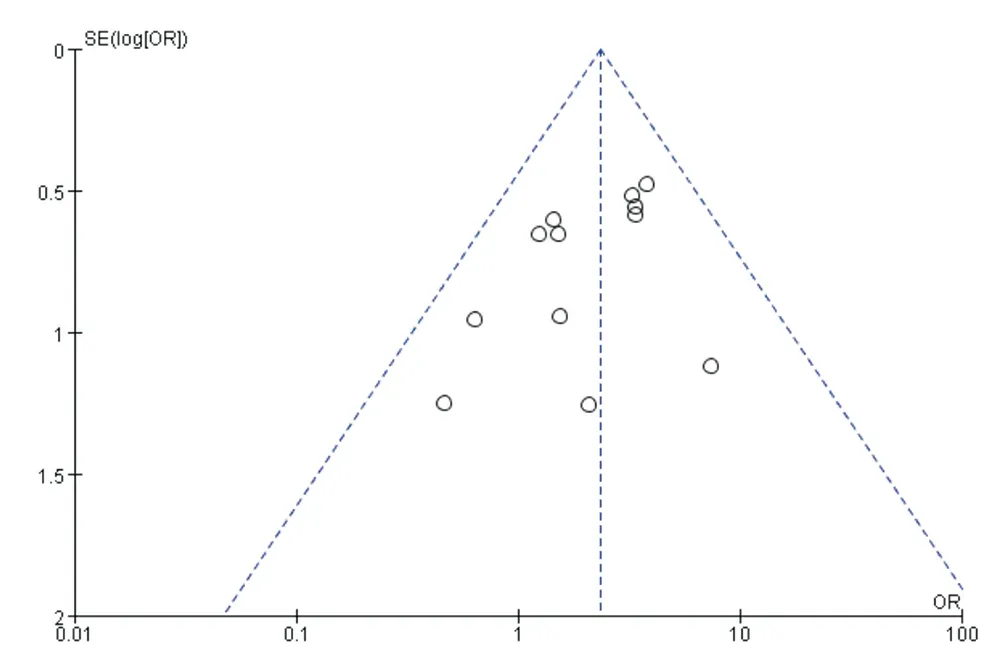
Figure 14 Inverted funnel plot of total clinical effectiveness
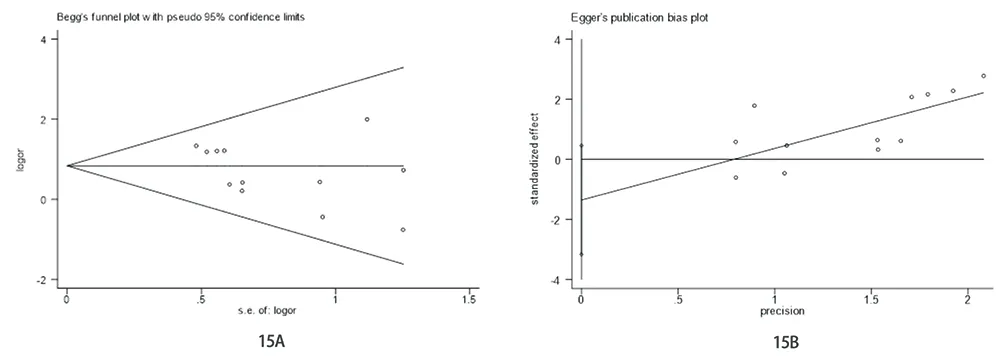
Figure 15 Publication of bias assessments
4. Discussion
At present, the pathogenesis of anxiety and/or depression in patients with coronary heart disease after PCI is not clear. The mainstream theory believes that it may be related to many factors,such as inflammation theory, autonomic nerve dysfunction,hypothalamic-pituitary-adrenal axis (HPA axis) dysfunction, platelet dysfunction, personality characteristics theory, gene polymorphism and so on. Zhang et al. [30] pointed out that although PCI can open blood vessels and save the dying myocardium in time, it can cause serious damage to vascular endothelium and increase the levels of endothelin-1 (ET-1), plasminogen activator inhibitor-1(PAI-1) and high-sensitivity C-reactive protein (CRP) in serum.At present, the principle of anxiety and/or treatment after PCI for coronary heart disease is that western medicine combined with anti-anxiety and depression drugs on the basis of conventional treatment of cardiovascular diseases. The commonly used antianxiety and depression drugs in clinic include benzodiazepines (such as alprazolam and clonazepam) and non-benzodiazepines (such as buspirone) anti-anxiety drugs, selective 5 - HT reuptake inhibitors(SSRIs), norepinephrine (NE) and 5 - HT dual uptake inhibitors(SNRIs), tricyclic and tetracyclic antidepressants. However, some anti-anxiety and depression drugs can cause a variety of adverse reactions, even cardiac toxicity, and the conventional treatment of Western medicine after operation is limited, which cannot effectively improve the mental and psychological disorders of patients. Traditional Chinese medicine uses the overall concept,multi-level and multi-target to comprehensively regulate the anxiety and/or depression associated with coronary heart disease after PCI, which can correct the local pathological factors of coronary heart disease and adjust the functional state of the whole body. Its unique advantages and significant clinical efficacy are increasingly recognized by clinical workers.
Expert consensus on TCM diagnosis and treatment of depression and/or anxiety before and after PCI[31] formulated by the Committee of Experts on Intervention in Cardiology of the Chinese Society of Traditional Chinese Medicine in 2015 classified the disease as'depression syndrome'in traditional Chinese medicine, and some scholars classified it as'lily disease', 'dirty mania'and'madness'according to its clinical manifestations. Most modern physicians believe that PCIfor coronary heart disease is an exogenous trauma, and the guide wire is placed into the stent from the radial artery or femoral artery, which belongs to the foreign body blocking the vein. It is bound to damage the collaterals and produce blood from the meridian. Blood stasis hides the inner heart, resulting in 'blood stasis syndrome'. Professor Chen et al. [32] believed that the body was damaged after operation, the Yuanqi was consumed, and the formation of blood stasis in meridians was aggravated, resulting in thoracic obstruction. The pathological process was similar to that of 'obstruction of heart and pulse' and 'obstruction of heart and pulse' in traditional Chinese medicine, belonging to the category of blood stasis syndrome. Professor Deng Tietao[33] believes that percutaneous coronary intervention and traditional Chinese medicine'Quxie'method is the same, with the effect of promoting blood circulation and removing blood stasis. Although it can solve the problem of myocardial reperfusion in a short time, and improve the symptoms of myocardial ischemia and chest pain to a certain extent, it can also damage vascular endothelial cells, resulting in a series of physiological and pathological manifestations. ‘ If the evil is gathered, the qi will be deficient ’. After PCI, the primordial qi is damaged, and the normal qi is dissipated, which affects the operation of qi and blood. The heart qi cannot promote the blood,and qi stagnation slows the blood flow, obstructs the meridians, and aggravates the formation of blood stasis. At the same time, after PCI,'qi-loss and qi-dissipation', qi-consumption and blood-injuries lead to blockage of heart and blood. The liver and heart are the viscera of mother and son, which interact with each other. The liver is the source of the disease, and the heart is the place of transmission.The disease is mostly caused by excessive anxiety, depression and anger[35]. Li et al. [36] also believed that PCIcould directly flow blood vessels to the location of the disease, which was equivalent to the method of 'activating blood circulation and removing blood stasis' in traditional Chinese medicine, and could remove blood stasis, phlegm turbidity and other evils. However, the operation itself consumed qi and hurt yin, which would lead to more deficiency of vital qi, poor qi movement, stagnation of liver and wood without occurrence,deficiency of heart qi, disturbance of heart monarch and long-term depression.
The results of Meta-analysis showed that on the basis of postoperative conventional western medicine treatment combined with traditional Chinese medicine treatment can further reduce the coronary heart disease patients with anxiety and/or depression after PCIHAMA, HAMD, SAS, SDS scale score, improve the curative effect of traditional Chinese medicine syndrome and clinical total effective rate, so we believe that traditional Chinese medicine treatment of coronary heart disease patients with anxiety and/or depression after PCI has significant curative effect, and good safety,worthy of clinical application. This study is the first time in China to systematically evaluate the efficacy of traditional Chinese medicine intervention in the treatment of coronary heart disease with anxiety and/or depression after PCI. Compared with the previous evaluation of traditional Chinese medicine in the treatment of this disease, this study is more fully retrieved. It is not only limited to the content of traditional Chinese medicine in the treatment of coronary heart disease with depression after PCI, but also included in the study of postoperative anxiety. The use of the latest control data not included in previous studies enriches the outcome indicators and contains more information. The safety of traditional Chinese medicine in the treatment of this disease is also evaluated, but there are still the following limitations:
(1) The overall quality of the included literature is low, and the description of the implementation of randomization grouping,allocation concealment and blind method is not clear enough;(2)The 23 studies included in this study were small sample studies without sample size calculation, which affected the credibility of the results to some extent. (3) The patients were not followed up in the included study. Only four studies clearly indicated the adverse reactions, and the other studies were not mentioned. Therefore, it is impossible to determine the long-term safety of traditional Chinese medicine for anxiety and/or depression after PCI in patients with coronary heart disease. (4) The course of the study is not equal, the end of the observation is not uniform, and the outcome indicators are diverse and different. Many indicators cannot be combined and analyzed, resulting in a significant reduction in the utilization of literature resources, which may reduce the reliability of the results.(5) Intervention programs vary greatly. Some studies only mentioned the addition of traditional Chinese medicine treatment in this paper,without syndrome differentiation of traditional Chinese medicine and providing specific doses and usages, which reduced the external authenticity of the conclusions of this study to some extent. (6) This study included only published Chinese and English literature, there may be publication bias. In conclusion, due to the quality limitations of included studies, this conclusion should be taken with caution.
Based on the above discussion, although the above limitations of this study will have different degrees of impact on the results of Meta-analysis, the conclusions still have certain reference value for clinical practice. It is suggested that in the future clinical research design, we should strictly follow the CONSORT37 report specification, try to select objective international general curative effect indicators, pay more attention to the evaluation of long-term prognosis, and improve the research level from the scientific design of clinical trials and the standardization of reports. We also look forward to more large sample, multicenter, long-term randomized double-blind controlled trials to further verify the clinical efficacy and safety of traditional Chinese medicine in the treatment of coronary heart disease with anxiety and/or depression after PCI.
Author’s contribution First author Liu Qian: Determine the search terms, responsible for literature retrieval, screening, data collection and processing and paper writing; Wang Haiyan: Determine search terms, responsible for article retrieval, screening, data collection and checking information; Xie Haitao: Participate in data collection and analysis,responsible for the improvement and revision of the content of the article; Communication author Chen Xiaohu: responsible for the article topics, design and review.
 Journal of Hainan Medical College2022年7期
Journal of Hainan Medical College2022年7期
- Journal of Hainan Medical College的其它文章
- Analysis on medication rule of traditional Chinese medicine treating chemotherapy-induced diarrhea based on traditional Chinese medicine(TCM) inheritance computing platform system
- Study on medication rules of traditional Chinese medicine for Meniere's disease based on data analysis
- Effect of Xifeng Capsule on blood stasis in patients with rheumatoid arthritis by regulating miR-126-VEGF/PI3K/AKT signaling pathway
- Design and characterization of a bifunctional bybrid antibacterial peptide LLH for bactericidal/endotoxin neutralization effects
- Box-Behnken response surface method combined with fingerprint to optimize the extraction process of total anthraquinone from Cassia seeds
- Effect of Zhiyang Pingfu Liquid on epidermal growth factor receptor inhibitor-related skin lesion
