横窦变异对完全/部分前循环梗死临床转归影响的研究
吴连爽 赵维纳 尹昌浩 徐丹
[摘要] 目的 探討有无横窦变异对前循环梗死患者的临床转归的影响。 方法 收集2019年2月至2020年12月发病且发病48 h内就诊于牡丹江医学院附属红旗医院、第二医院神经内科的已行头颅CT/DWI/MRI检查前经脑梗死牛津郡社区卒中项目(OCSP)临床分型明确为完全前循环梗死(TACI)患者和部分前循环梗死(PACI)患者,最终对75例前循环梗死患者进行磁共振静脉血管成像(MRV)及颈静脉彩超检查,根据检查结果分为横窦无变异与横窦变异两组,记录横窦变异分级、颈内静脉管径、梗死体积、基线NIHSS评分、90 d mRS评分。分析横窦变异对完全/部分前循环梗死部位、梗死体积及临床转归的影响。 结果 前循环梗死患者中,横窦变异侧与同侧前循环梗死的形成有关,差异有统计学意义(P<0.05)。横窦变异同侧的颈内静脉管径显著小,差异有统计学意义(P<0.05)。完全前循环梗死合并横窦变异组患者的基线NIHSS和90 d mRS评分均高于部分前循环梗死合并横窦变异组,差异均有统计学意义(P<0.05)。完全前循环梗死横窦变异组90 d mRS评分高于无变异组,差异有统计学意义(P<0.05)。 结论 横窦变异更容易发生同侧前循环梗死,且横窦变异同侧的颈内静脉管径显著小;合并横窦变异的完全前循环梗死与部分前循环梗死比较,临床症状重、预后差;完全前循环梗死合并横窦变异组的预后更差。
[关键词] 脑梗死;前循环;横窦变异;转归预后
[中图分类号] R743.3 [文献标识码] A [文章编号] 1673-9701(2022)09-0021-05
Study on the impacts of transverse sinus variation on the clinical outcome of total/partial anterior circulation infarcts
WU Lianshuang1 ZHAO Weina2,3 YIN Changhao2,3 XU Dan2,3
1.Mudanjiang Medical University, Mudanjiang 157000, China; 2.Department of Neurology IV, Hongqi Hospital Affiliated to Mudanjiang Medical University, Mudanjiang 157000, China; 3.Key Laboratory of Ischemic Stroke Prevention and Control in Heilongjiang Province,Mudanjiang 157000,China
[Abstract] Objective To investigate the impacts of the presence or absence of transverse sinus variation on the clinical outcome of patients with anterior circulation infarcts. Methods Patients who were admitted to the Department of Neurology of Hongqi Hospital Affiliated to Mudanjiang Medical University and The Second Affiliated Hospital of Mudanjiang Medical University from February 2019 to December 2020 with onset within 48 hours and who had undergone cranial computed tomography (CT)/diffusion weighted imaging (DWI)/ magnetic resonance imaging (MRI), and clinically diagnosed with clinical typing of total anterior circulation infarcts (TACI) and partial anterior circulation infarcts (PACI) by the Oxfordshire Community Stroke Project (OCSP) for cerebral infarction were selected as the study subjects. 75 patients with anterior circulation infarcts who underwent magnetic resonance venography (MRV) and jugular vein ultrasound examination were divided into the non-transverse sinus variation group and the transverse sinus variation group according to the examination results. The grading of transverse sinus variation, internal jugular vein diameter, infarct volume, the score of National Institute of Health Stroke Scale (NIHSS) at baseline, and 90-day modified Rankin Scale (mRS) score were recorded. The impacts of transverse sinus variation on the site, infarct volume, and clinical outcome of TACI/PACI were analyzed. Results In patients with anterior circulation infarcts, the transverse sinus variant was associated with the formation of ipsilateral anterior circulation infarcts,with statistically significant difference(P<0.05). The diameter of the internal jugular vein on the ipsilateral side of the transverse sinus variant was significantly smaller, with statistically significant difference(P<0.05).The baseline NIHSS and 90-day mRS scores were higher in the TACI combined with transverse sinus variant group than those in the PACI combined with transverse sinus variant group, with statistically significant differences(P<0.05).The 90-day mRS score was higher in the TACI combined with transverse sinus variant group than that in the non-transverse sinus variation group, with statistically significant difference(P<0.05). Conclusion Transverse sinus variation is more likely to result in ipsilateral anterior circulation infarcts, and the internal jugular vein diameter on the ipsilateral side of transverse sinus variation is significantly smaller. Compared with the PACI combined with transverse sinus variant group, there are severer clinical symptoms and worse prognosis in the TACI combined with transverse sinus variation group. In addition, the prognosis of TACI combined with transverse sinus variation group is worse than that of the PACI combined with transverse sinus variant group.
[Key words] Cerebral infarction; Anterior circulation; Transverse sinus variation; Outcome and prognosis
前循环梗死(anterior circulation infarction,ACI)是导致患者具有更高的缺血性卒中发生率及预后差的梗死类型[1-2]。根据OCSP临床分型前循环脑梗死分为完全前循环梗死(TACI)和部分前循环梗死(PACI)[3]。研究表明[4-5],急性脑梗死中,TACI患者的神经功能损害最重,康复时间最长,预后最差。脑循环包括动脉和静脉系统,既往研究过多的关注于动脉血管变化,但静脉、静脉窦在脑血流及颅内压力改变中居主要地位[6]。颅内静脉变异较多,但大多数患者无临床症状[7]。横窦(transverse sinus,TS)是正常人静脉窦变异的最常见类型[8],且越来越多的研究表明[5],TS变异在整个脑静脉及静脉血流动力学中有重要作用。
笔者认为TS变异在动脉梗死事件中的作用可能涉及以下2个方面:①先天横窦变异影响动脉血液回流,长年累月使动脉粥样硬化的进程加重;②横窦变异影响动脉回流,导致大面积前循环梗死急性期的水肿加重,直接影响预后。本研究通过对前循环梗死患者的横窦变异分析,评估其对前循环梗死的发生率、疾病严重程度的影响以及临床转归等方面的临床价值,现报道如下。
1 资料与方法
1.1 一般资料
收集2019年2月至2020年12月发病且发病48 h内就诊于牡丹江医学院附属红旗医院、第二医院神经内科的已行头颅DWI/MRI证实为前循环梗死的75例患者,并在48 h之内完成头MRV及颈内静脉彩超检查,检查结果由一名有经验的影像、超声科医师和一名神经科医师经过培训后进行盲法评估。课题研究通过牡丹江医学院医学伦理委员会的审批,所有被试者均需签署知情同意书。
1.2 磁共振成像方法
均采用荷兰飞利浦公司3.0T TX磁共振仪进行影像学系统扫描,常规行T1WI、T2WI、Flair、DWI、MRV检查,MRV检查参数:采用三维相位对比(phase contrast,PC),流速编码Venc=15 cm/s,TR/TE=25 ms/6 ms,翻转角10°,矩阵256×256,层厚0.8 mm。
1.3 诊断标准
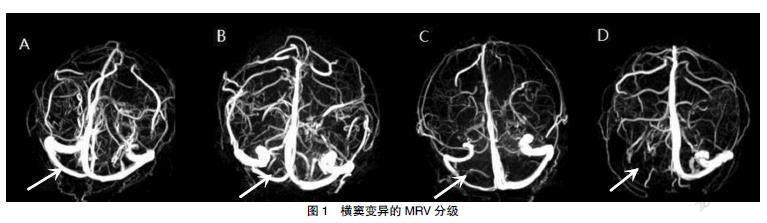
TS变异不对称分级标准:由于TS中段易于识别及测量,故选择中段测量TS管径(cm)。在MRV中,根据双侧TS是否不对称,被分成4级[9]。TS变异是指2级及3级。MRV见图1。
根据TS是否对称MRV分为4级。A:0级(TS双侧不对称≤10%,箭头);B:1级(TS不对称>10%,且≤50%,箭头);C:2级(TS不对称>50%,箭头;D:3级(TS纤细或者缺失,箭头)。
静脉彩超评定标准:双源彩色超声通过7-MHz线性传感器(iU22;美国飞利浦医药系统)传导,技术人员对患者临床信息行盲法评定。在颈内静脉中段(J2)和上段(J3)记录以下参数:时间平均中位流速和管腔横截面积。
1.4 统计学方法
应用SPSS 25.0统计学软件处理数据,计量资料用均数±标准差(x±s)表示,采用t检验。计数资料用[n(%)]表示,采用χ2檢验。P<0.05为差异有统计学意义。
2 结果
2.1 横窦变异率及横窦变异的意义
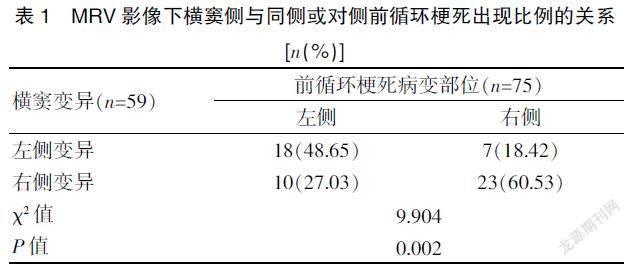
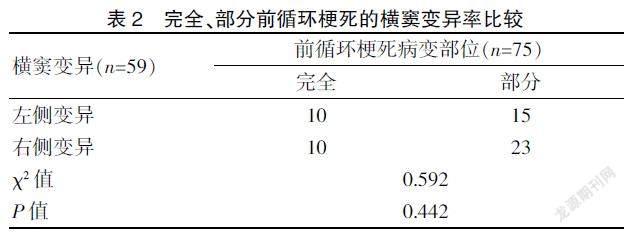
在所有前循环梗死患者中,横窦变异在同侧前循环梗死的发生率高,差异有统计学意义(P<0.05)。在完全、部分前循环梗死患者中横窦变异率比较,差异无统计学意义(P>0.05)。见表1~2。
2.2 完全前循环梗死患者的横窦变异情况
一例78岁老年男性患者,DWI示左侧完全前循环梗死(图2A,箭头),入院第3天临床症状加重,行头CT示:梗死面积较前增大(图2B,箭头),MRV显示同侧横窦变异(图2C,箭头)。一例67岁老年女性患者DWI示左侧完全前循环梗死(图2D,箭头),入院第5天临床症状加重,行头CT示:梗死面积较前增大,出现脑水肿且同侧侧脑室受压(图2E,箭头),MRV显示对侧横窦变异(图2F,箭头)。
2.3 颈内静脉管径不对称的意义
横窦变异同侧的颈内静脉管径显著小,其与非变异横窦侧比较,差异有统计学意义(χ2=33.446,P<0.001)。见表3。
2.4 前循环梗死合并有无横窦变异与责任病灶体积的关系
在前循环梗死患者中,合并TS变异的梗死体积明显增大(表现为大、中、小梗死灶均较无横窦变异组人数增多)。见图3。横窦无变异与横窦变异组中各种梗死灶体积的大小比较,差异无统计学意义(P>0.05)。见表4。
2.5 前循环梗死患者与横窦有无变异间临床转归分析
与PACI组比较,合并横窦变异的TACI组具有更差的NIHSS及90 d mRS评分,差异均有统计学意义(P<0.05),TACI合并横窦变异组与无横窦变异组比较,90 d的mRS评分更差,差异有统计学意义(P<0.05)。见表 5。
注 *TACI横窦变异与PACI横窦变异组相比,P<0.05,且NIHSS、mRS评分,分别为t=8.108,P=0.000;t=8.108,P=0.001;#TACI横窦无变异与PACI横窦无变异组相比,P<0.05,但NIHSS、mRS评分的统计值分别为t=3.799,P=0.055;t=2.267,P=0.053;^TACI横窦变异与TS无变异组相比,P<0.05,而NIHSS、mRS评分的统计值分别为t=0.219,P=0.829;t=3.213,P=0.012;&PACI横窦变异与无变异组相比,P<0.05,但NIHSS、mRS评分的统计值分别为t=0.781,P=0.438;t=0.612,P=0.543
3 討论
3.1 前循环梗死与TS变异相关性分析
3.1.1 前循环梗死与TS变异率 本研究中右侧TS变异33例,变异率为56.0%,但与完全/部分前循环梗死的发生率比较,差异无统计学意义(P>0.05)。研究结果与既往文献一致,认为TS通常不对称,TS发育不良或发育不全是一种常见的解剖学变异,约30%左右的病例会出现TS一侧闭锁或发育不良,且半数以上的病例以右侧TS为主[10]。TS变异可能与先天解剖结构、发育异常有关。如果TS在发育过程中迅速增大和减小,可能会发生TS的变异,如直径和边缘不规则、间隔形成和节段缺失[11]。
3.1.2 前循环梗死形成与TS变异 本研究结果显示,TS变异更容易发生同侧前循环梗死,即TS变异与同侧ACI的形成有关,其与非变异横窦侧比较,差异有统计学意义(P<0.05)。研究结果与Drozdov等[12]的结果符合,通过观察5例MCA梗死后出现致死性脑水肿的患者中有4例出现TS横窦变异,与出现同侧颅内静脉引流异常的结果符合。可能原因是TS变异引起脑静脉血液回流障碍,导致颅内静脉的引流异常,在静脉系统和毛细血管内淤积的血液,引起局部的脑组织肿胀,进而导致颅内压增高[13]。颅内压增高损害脑血管自主调节功能,延长脑循环时间,影响动脉血液回流,加速动脉粥样硬化的进程[14],从而易形成同侧动脉血栓且导致临床症状加重。虽然本实验中发现横窦变异与同侧前循环梗死的发生率相关,但样本量较小,仍需大样本实验证实。
3.1.3 前循环梗死TS变异与颈内静脉管径 因本研究行颈内静脉彩超时受技术所限未获得患者血流量相关数值,故只评估了管径,通过评估颈内静脉管径后发现,管径不对称比例约48%,且与横窦变异侧做分析后,结果提示TS变异同侧的颈内静脉管径显著小,这也与先前研究一致[15-17]。从血流动力学的角度来看,毛细血管和静脉是脑血管阻力的重要贡献者,但在生理条件下,它们在血流调节中的作用微乎其微,当出现缺血时,阻力小动脉和动脉最大限度地扩张并变得反应迟钝[18]。那么,横窦变异与颈内静脉管径不对称导致血流动力学异常也可以解释。但由于本研究中受限彩超技术,导致未获得颈内静脉血流量相关数值。
3.2 TS变异与前循环梗死患者梗死体积的关系
本研究中,梗死体积在TS无变异与TS变异组间比较,差异均无统计学意义(P>0.05),与Tumanova等[19]研究的梗死体积的增大在静脉窦变异后导致缺血性卒中水肿加重有关的结果不一致。可能与入组患者人数较少、临床严重程度中等程度偏上有关。静脉系统形态的异常是否类似于不完整的Willis环的后果仍需要纵向研究。
3.3 前循环梗死合并横窦变异的临床转归影响分析
王本孝等[20]发现OCSP的这四种临床类型中,TACI患者入院时病情、神经功能缺损重,梗死面积大,预后差,致残率高。NIHSS、90 d mRS是评价患者神经功能缺损严重程度、恢复情况的评估指标,评分越低意味着瘫痪程度越轻、预后越好。本研究中,完全/部分前循环梗死横窦不同变异类型之间,TACI横窦变异与PACI横窦变异组比较,TACI横窦变异组的NIHSS及90 dmRS评分更高,提示与严重的临床症状、预后差有关。TACI横窦变异与无变异组比较,TACI变异组的90 d mRS评分更高,提示预后差。本研究结果与早前的研究结果具有较好的一致性,如Kaartinen[21]等研究表明,在9例MCA梗死患者中有3例出现致死性水肿,脑血管造影显示同侧TS闭锁和颈内静脉发育不良,发现除梗死体积外,同侧颅内引流静脉发育不良或闭塞与MCA梗死早期致死性水肿有关,导致更严重的临床表现。另外,Munuera等[22]研究发现梗死同侧横窦闭塞或发育不良的患者预后差,同侧颈内静脉闭塞或发育不良的发生率与预后良好的患者相当。对侧横窦闭塞、发育不良或对侧颈内静脉闭塞、发育不良在预后较差的患者与功能良好的患者中比例相似。随着人们对脑静脉循环的兴趣的发展,应该更好地了解静脉及静脉窦及其在动脉缺血性脑水肿中的作用。本研究入组患者多数为中等程度的梗死,完全前循环梗死的患者数量相对较少,可能影响一些统计结果。
综上所述,TS变异更容易发生同侧前循环脑梗死,且TS变异同侧的颈内静脉管径显著小。合并TS的TACI组与PACI组比较,临床症状重、预后差。与TACI无变异组比较,合并TS变异组的预后更差。
[参考文献]
[1] Zhang K,Li T,Tian J,et al. Subtypes of anterior circulation large artery occlusions with acute brain ischemic stroke[J]. Sci Rep,2020,10(1): 3442.
[2] Flint AC,Bhandari SG,Cullen SP,et al. Detection of anter- ior circulation large artery occlusion in ischemic stroke using noninvasive cerebral oximetry[J].Stroke,2018,49(2):458-460.
[3] Tinker RJ,Smith CJ,Heal C,et al. Predictors of mortality and disability in stroke-associated pneumonia[J].Acta Neurol Belg,2021,121(2):379-385.
[4] Yang Y,Torbey MT. Angiogenesis and blood-brain barrier permeability in vascular remodeling after stroke[J].Curr Neuropharmacol,2020,18(12):1250-1265.
[5] Hua J,Liu P,Kim T,et al. MRI techniques to measure arterial and venous cerebral blood volume[J].Neuroimage,2019,187:17-31.
[6] Saposnik G,Barinagarrementeria F, Brown RD Jr, et al. Diagnosis and management of cerebral venous throm-bosis:A statement for healthcare professionals from the American Heart Association/American Stroke Association[J].Stroke,2011, 42(4):1158-1192.
[7] Quan T,Ren Y,Lin Y,et al. Role of contrast-enhanced magnetic resonance high-resolution variable flip angle turbo-spin-echo(T1 SPACE) technique in diagnosis of tra-nsverse sinus stenosis[J].Eur J Radiol,2019,120: 108 644.
[8] Gul B,Samanci C,Uluduz DU,et al. Does measurement of the jugular foramen diameter on MRI help to differentiate transverse sinus thrombosis from unilateral transverse sinus hypoplasia[J].Radiol Med,2021,126(3):430-436.
[9] Fofi L,Giugni E,Vadalà R,et al. Cerebral transverse sinus morphology as detected by MR venography in patients with chronic migraine[J]. Headache,2012,52(8):1254-1261.
[10] Arauz A,Chavarria-Medina M,Pati?觡o-Rodriguez HM,et al. Association between transverse sinus hypoplasia and cerebral venous thrombosis:A case-control study[J].J Stroke Cerebrovasc Dis,2018,27(2):432-437.
[11] Massrey C,Altafulla JJ,Iwanaga J,et al.Variations of the transverse sinus: Review with an unusual case report[J].Cureus,2018,10(9):e3248.
[12] Drozdov AA,Javan R,Leon Guerrero CR,et al. Asymmetry of medullary veins on multiphase CT-angiography in patients with acute ischemic stroke[J].J Stroke Cerebrovasc Dis,2020,29(10):105 064.
[13] Tong LS,Guo ZN,Ou YB,et al. Cerebral venous collaterals: A new fort for fighting ischemic stroke[J].Prog Neurobiol,2018,(163-164): 172-193.
[14] Liu M,Xu H,Wang Y,et al. Patterns of chronic venous insufficiency in the dural sinuses and extracranial draining veins and their relationship with white matter hyperintensities for patients with Parkinson's disease[J]. J Vasc Surg,2015,61(6):1511-1520.
[15] Vink A,Schoneveld AH,Richard W,et al. Plaque burden, arterial remodeling and plaque vulnerability:Determined by systemic factors[J].J Am Coll Cardiol,2001,38(3):718-723.
[16] Saiki K,Tsurumoto T,Okamoto K,et al. Relation between bilateral differences in internal jugular vein caliber and flow patterns of dural venous sinuses[J].Anat Sci Int,2013, 88(3):141-150.
[17] Matsuda W,Sonomura T,Honma S,et al. Anatomical varia- tions of the torcular Herophili: Macroscopic study and clinical aspects[J]. Anat Sci Int,2018,93(4):464-468.
[18] Connor-Schuler R,Daniels L,Coleman C,et al. Presence of spontaneous echo contrast on point-of-care vascular ultrasound and the development of major clotting events in coronavirus disease 2019 patients[J].Crit Care Explor,2021,3(1):e0320.
[19] Tumanova UN,Lyapin VM,Burov AA,et al. The possibility of postmortem magnetic resonance imaging for the diagno- stics of lung hypoplasia[J].Bull Exp Biol Med,2018,165(2):288-291.
[20] 王本孝,許平.急性脑梗死OCSP分型与颈动脉粥样硬化的相关性[J].中国动脉硬化杂志,2010,18(11):885-888.
[21] Kaartinen M,van der Wal AC,van der Loos CM,et al. Mast cell infiltration in acute coronary syndromes:Implications for plaque rupture[J].J Am Coll Cardiol,1998, 32(3):606-612.
[22] Munuera J,Blasco G,Hernández-Pérez M,et al. Venous imaging-based biomarkers in acute ischaemic stroke[J]. J Neurol Neurosurg Psychiatry,2017,88(1): 62-69.
(收稿日期:2021-05-12)