A systematic review of the treatment of lower eyelid retraction and our attempt of a dermal-orbicularis oculi suspension flap
Yi Ding ,Xing Huang ,Lin Lu,Rui Jin,Di Sun,Jun Yang ,Xusong Luo
Department of Plastic and Reconstructive Surgery,Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai 200011,China
Keywords:Lower eyelid retraction Dermal-orbicularis oculi suspension flap Orbicularis retaining ligament
ABSTRACT Lower eyelid retraction describes the inferior displacement of the lower eyelid with or without inversion or ectropion.Based on the causes of lower eyelid retraction,we divided the forming factors of lower eyelid retraction into three categories:(1) change in the balance of forces associated with the lower eyelid margin;(2) excessive loss of lower eyelid volume;(3)changes in the relative position of the eyeball and lower lid margin.In this review,the corresponding treatment methods are elaborated on individually for the above three forming factors.We also reported,for the first time,a new treatment for lower eyelid retraction.We created a dermal-orbicularis oculi suspension flap on the lateral side of the canthus and suspended it upward and inward on the dense connective tissue over the lateral bony surface of the orbital rim.The longest follow-up time was one year,and the results were satisfactory.
1.Introduction
The lower lid is anatomically divided into three layers:anterior,middle,and posterior.The anterior layer includes the skin and orbicularis oculi muscle;the middle layer includes the orbital septum and orbital fat;and the posterior layer includes the tarsus,conjunctiva,and lower lid retractors(Fig.1).The position of the lower eyelid depends on the balance between several factors:tension of the horizontal canthal ligaments,lower eyelid length and tonicity,distensibility of the vertical lower eyelid retractors,adequacy of the fornix and palpebral conjunctivae,location of the canthal ligament,tension of the orbicularis oculi,and degree of eye prominence.1
Lower eyelid retraction describes the inferior displacement of the lower eyelid with or without inversion or ectropion.In severe cases,it may cause tearing,dry eye,ocular irritation,corneal scarring,exposure keratitis,and even corneal ulcers.In contrast,most current studies rely on two main indicators to define lower eyelid retraction:margin reflex distance 2 (MRD2) and inferior scleral show (ISS).Lower eyelid retraction can be identified by an ISS >0 and/or an MRD2 >6(Fig.2).2Some scholars suggested that the MRD2 at the lateral limbus and tarsal marginal are more sensitive in identifying eyelid retraction and eversion.3

Fig.2.When a light source is placed in front of the patient,MRD2 is defined as the distance between the lower eyelid margin and the central reflective cornea.ISS is defined as the scleral exposure between the lower eyelid margin and the lowest point of the iris.MRD2,margin reflex distance 2;ISS,inferior scleral show.
The main anatomical causes of lower lid retraction are prominent eyes,lateral canthal tendon laxity,middle lamella scarring,and midface descent.4The main causes of lower lid retraction are congenital,traumatic,infectious,tumorous,neurogenic,and,increasingly in recent years,medical and esthetic,such as lower eyelid blepharoplasty and undergoing of procedures for lowering the lower eyelid.5
Therefore,we can divide the factors that result in lower eyelid retraction into three main categories:(1)change in the balance of forces associated with the lower eyelid margin,including the downward pull caused by factors such as vertical gravitational aging that leads to midface descent and middle lamella scarring,as well as the horizontal pull caused by eyelid laxity,which results in a longer eyelid length and lower canthus;(2) excessive loss of lower eyelid volume;(3) changes in the relative position of the eyeball and lower lid margin.For these different formative factors,we review relevant articles,discuss the latest developments,and describe different treatments.We also report our innovative work in the treatment of lower eyelid retraction.We developed a dermal-orbicularis oculi suspension (DOS) flap at the lateral side of the canthus and suspended it on the dense connective tissue over the lateral bony surface of the orbital rim.The DOS flap had sufficient upward traction,which could effectively correct lower eyelid retraction caused by different reasons,and it had persistent effects.
2.Correction of the force imbalance associated with the lower eyelid margin
2.1.Frost suture
In response to vertical gravity or tension,a Frost suture tarsorrhaphy to the eyebrow is usually placed with 5-0 Prolene sutures to immobilize the lower eyelid postoperatively for 7 days in case of retraction.It should be noted that Frost suture is only an adjunct treatment,instead of an individual treatment,and it usually needs to be used in combination with other treatments.It could be a supporting measure after surgery or part of lower eyelid retraction correction surgery.
2.2.Lateral canthal anchoring
The main causes of lateral canthal tendon laxity include senile/paralytic,congenital,traumatic,and/or medical and esthetic causes.Lateral canthal tendon laxity is the anatomical cause of lower eyelid retraction that is most easily repaired.
Lateral canthal anchoring is usually classified into lateral canthal anchoring without lysis (lateral canthopexy) and lateral canthal anchoring with lysis (lateral canthoplasty).
For the standard positioned eye,the lateral canthus is usually at the level of the inferior margin of the pupil.In most patients,only lateral canthopexy yields significant results.Lateral canthus anchoring is also called lateral canthopexy because it does not require lysis of the lateral canthal ligament and only the lateral canthus is sutured.In this case,for lateral canthopexy,1-0 non-absorbable sutures are used to sew the upper and lower joint tendons exactly at the level of the inferior margin of the pupil,with the ends of the sutures passing through the periosteum at least 4 mm medial to the lateral orbital rim;then,a knot is tied 3–4 mm from the outer periosteum of the lateral orbital rim.
Lateral canthoplasty is required to shorten the eyelids of patients with lateral canthal tendon laxity.An eyelid distraction test is used to define eyelid laxity.The lower eyelid is pulled away from the globe.If the distance created between the eyelid and globe is ≥8 mm,this indicates eyelid laxity.The surgeon can perform a traction test in which a finger is placed on the outer corner of the patient’s eye and the tendon is determined to be lax by applying upward and lateral pressure.In cases where preoperative traction tests confirm the presence of lower eyelid laxity,lysis of the lateral canthus is required.The lower lid margins are also shortened.Therefore,lateral canthal anchoring with lysis is also known as lateral canthoplasty.The amount of lysis can be determined by testing the degree of excess when the lateral edge of the lower eyelid is close to the lateral orbital edge.The sutures are the same as for the lateral canthopexy described above.The upper eyelid canthus tendon and lateral end of the lower eyelid tarsus are first sutured,followed by the same steps as for the lateral canthopexy.
2.3.Lateral tarsoconjunctival flap suspension treatment
Neurogenic lower eyelid retraction due to facial nerve and optic nerve palsy can be treated with suspension.Tao6proposed the use of a lateral tarsoconjunctival flap suspension procedure in patients with permanent unilateral paralytic eyelid malposition caused by facial nerve paresis.All patients generally showed improvement in eyelid position and cosmesis.Subsequently,Conger7used a tarsoconjunctival suspension flap in patients with post-blepharoplasty lower eyelid retraction,and functional and esthetic improvements were observed.
3.Supplement to the volume of the posterior and middle layers of the lower eyelid
Generally,there is a lack of volume in the middle layer of the lower eyelids.Injections of autologous fat and hyaluronic acid are effective and minimally invasive procedures that can correct both lower eyelid depression and retraction by pushing and stretching the entire anterior tarsus.In addition,stem cells in fat can play a role in combating scar recurrence.8Some researchers have recommended starting the injection slowly from the deep lower orbital rim.Closer to the lid margin,the injection is positioned more superiorly and closer to the surface.
When significant eyelid laxity,scar contracture,and edema are excluded,hyaluronic acid injection could be an effective treatment for senile/congenital or postsurgical retraction.Steinsapir9proposed the concept of altering the bulk modulus of the lower eyelid as the basis for improving lower eyelid retraction,suggesting that higher G-prime fillers should be favored over lower G-prime fillers,a finding consistent with clinical experience.The filler acts as a lift as it changes the balance in the lower eyelid,forcing it to move upward to gain a new balance.10These injections can effectively stretch the lower eyelid and push the eyelid margin upward.The filler effectively stretches the eyelid like a spring,creating the necessary elevation and internal rotation towards the eye.11,12The complications are minor,including bruising,swelling,and contour irregularities.13
4.Supplement to the structure of the posterior and middle layers of the lower eyelid
Spacer grafts are usually recommended in cases where the midposterior layer of the lower lid is structurally deficient.The general approach is as follows:(1) lysis of the middle lamellar scarring;(2)placement of a posterior lamellar spacer graft;(3) recruitment of the anterior lamella via midface lifting;(4) lower eyelid tightening;(5)vertical elevation and immobilization of the lower eyelid using a Frost suture.
4.1.Lysis of the middle lamellar scarring
It has been suggested that the inflammatory response of the orbital fat pad after cosmetic surgery has led to scarring between the orbital septum and capsulopalpebral fascia,causing retraction of the lower eyelid and posterior displacement of the orbital fat.These displacements may have contributed to postoperative lower eyelid depression and scleral exposure.14The surgeon can clarify the etiology by performing a vertical traction test,pushing the lower lid upward to the cornea with a finger;resistance to this movement may indicate the presence of a middle lamellar scar.Scar treatment aims to separate the capsulopalpebral fascia from the orbital septum.The conjunctiva and lid capsule fascia are released from the lower edge of the tarsus using a transconjunctival approach.The plane between the capsulopalpebral fascia and orbital septum is released from the scar tissue,allowing the orbital fat to return to its normal anatomic plane.A graft of similar thickness to that of the lid is selected and then placed at the lower edge of the tarsus,between the lid conjunctiva and capsulopalpebral fascia.
4.2.Placement of a posterior lamellar spacer graft
In some patients with lower eyelid retraction,there is usually a deficiency in the posterior and middle layers of the lower eyelid,and this can be corrected by choosing a spacer graft in combination with other operations.Various graft options are usually available and classified as autologous tissue grafts,alloplastic grafts,allogeneic grafts,and xenografts.
4.2.1.Autologous grafts
Autologous options include the hard palate,temporalis muscle mucosa,dermis fat,and ear/nasal septal cartilage.
The hard palate is the gold standard for implants because of its thickness,stiffness,and shape,which are most similar to that of the tarsus.First described by Siegel,15the hard plate generally measures at 5 mm × 20–25 mm and rarely exceeds 6 mm in vertical height.For every 1 mm of desired vertical lower eyelid lift,using 2–3 mm of hard palate graft is recommended.The upper edge of the hard palate is secured to the lower margin of the tarsus,and the lower edge is secured to the lower eyelid retractors.However,the hard palate has disadvantages of donor-site discomfort and a high incidence of donor complications.Custom-molded plates have been used to reduce donor-site discomfort.The hard palate should be placed below the eyelid to minimize contact with the cornea.The hard palate is also not effective in reconstituting orbital volume;therefore,it is not a substitute for other options of volume supplementation.Ding16attempted to repair lower lid retraction in anophthalmic patients with lower eyelid retraction by using a hard palate graft in combination with recession of inferior retractors and lateral tarsal strip suspension,which achieved long-term stable results.
Dermis fat is more easily available and is in sufficient supply to restore the lost orbital volume,also supporting the posterior wall.There are several donor site options for dermis fat grafts,including the gluteal,flank,and periumbilical regions.In general,dermis grafts should be at least 1.5–2.0-fold greater in size.Complete removal of the epithelium is essential to minimize keratin production and cilium transplantation.Below the orbicularis oculi muscle,there is a fat layer containing vessels and nerves,which is called suborbicularis oculi fat(SOOF).The fat side of the graft is directed towards the SOOF,and the dermis side is continuous with the ocular surface.However,dermal fat also has disadvantages,such as unstable absorption rates and possible changes in size with changes in weight.It also requires waiting for dermal conjunctival epithelialization,which may cause irritation to the eye.17
Ear cartilage and nasal septal cartilage-mucosa composite tissue are also options for autologous materials that are easily accessible,have relatively low complications at the donor site,and have a low rate of absorption after transplantation.The size of the cartilage to be obtained should match that of the defect.As the ear cartilage is not covered by mucosa and may increase the risk of corneal injury,the conjunctiva should be placed over the posterior graft to avoid ocular irritation.In contrast,the nasal septal cartilage-mucosa composite tissue is covered by a mucosal surface;thus,the recovery process is shorter.Care should be taken to protect and preserve the mucosa on the other side of the septum to reduce the formation of septal defects.However,as the cartilage is too stiff,it is important to avoid significant contour changes that are easily palpable after surgery.The size of the cartilage obtained is also limited.
4.2.2.Alloplastic graft
The alloplastic materials used include Medpor and polytetrafluoroethylene.Medpor is a good structural support,but it has a high risk of complications and failure and is more likely to cause bone growth.18These problems greatly restrict its clinical application.
4.2.3.Xenograft
Xenograft materials include the acellular dermal matrix (ADM) and decellularized bioengineered grafts (Tarsys).Among these,ADM is the most commonly used xenograft material.ADM also has good structural support,does not require an autologous donor,and has a relatively low incidence of complications.During the procedure,the surgeon needs to redrape a 1–2 mm conjunctival cuff over the superior border of the xenograft,thus facilitating conjunctival epithelialization.It is also important that ADM cannot restore orbital volume.Tao attempted to investigate the effectiveness and safety of ADM from different sources after repair of lower lid retraction,and the final success rate of the procedure was approximately 75%–100%.Minor complications included cyst formation,infection,chemosis,pyogenic granuloma,and corneal abrasion.No serious complications,such as blindness,anaphylactic reaction,or terminal disease transmission,occurred.The short-term results of ADM are satisfactory,and it fills the gap for patients who do not have an alternative graft.However,its long-term efficacy and safety remain unclear.19
Specifically,no difference was found between the hard palate mucosa and AlloDerm.In addition,no prospective randomized trials have compared the efficacy of one spacer graft material to another.All reviewed cohort studies comparing the two graft types failed to convincingly show that one graft type resulted in greater eyelid elevation than the other.Although one study showed that AlloDerm had a higher contracture rate than hard palate mucosa,this did not have an effect on eyelid elevation and longevity.20
5.Supplement to the struction of the anterior layer of the lower eyelid
A defect in the anterior layer of the lower eyelid,which includes the skin and orbicularis oculi muscles,is a common cause of lower lid recession.The defect may be due to thermal or chemical burns,trauma,cosmetic lower eyelid surgery,laser resurfacing,chemical peel,or topical use of retinoids.21Options for correct anterior lamellar defects include full-thickness skin grafts,local skin flap or myocutaneous flap graft,or a midface lift.
5.1.Full-thickness skin grafts
Ideal donor sites of full-thickness skin grafts should be considered in the following order of preference:excess upper eyelid skin,skin in front of or behind the ear,supraclavicular skin,medial upper arm,and inguinal area.First,whether the patient’s lower lid requires canthoplasty must be determined.Next,the lid margin is suspended with Frost sutures to provide a vertical upward pull.Then,a subciliary incision is made down the length of the lower lid,and the area of defect is measured after adequate release of the mid-layer scar.After full-thickness skin is obtained,sutures are placed and pressure bandaging is applied.
Modified Hughes conjunctival flaps are commonly used to repair fulleyelid defects.Chen22used these in patients with refractory cicatricial lower eyelid retraction to reconstruct above the tarsus with excision of the scarred lid margin and full-thickness graft skin over the tarsoconjunctival flap,which could reconstruct a new lower lid margin with a reduced risk of recurrence and complications.
5.2.Local myocutaneous flap
Lower eyelid skin requires a rich blood supply and has a potentially higher rate of necrosis and infection.In contrast,a local skin flap or myocutaneous flap can bring its own blood supply to the lower eyelid,which can be useful in patients with previous irradiation or trauma.
The Tripier flap is a bipedicle myocutaneous flap that is transposed from the upper to the lower eyelid.Variants of this flap have been described for treating the medial or lateral eyelid with a single pedicle but may be limited by the blood supply.23The Fricke flap is a temporal frontal unipedicle flap transposed to the upper or lower eyelid.To avoid distal necrosis,the length-to-width ratio should not exceed 4:1.24However,both of these flaps may cause eyebrow asymmetry,as seen with the Tripier flap,in which the upper eyelid is tightened,and with the Fricke flap,in which the eyebrow is elevated.
5.3.Midface lifting
Pascali25emphasized that midface lifting based on purely vertical repositioning makes it possible to recruit a considerable amount of“new”skin at the lower eyelid,thus ensuring a decrease in vertical distraction and correct recovery of the height of the external lamellar plane.
Sales-Sanz26attempted a reconstructive subperiosteal midface lifting through three different incisions,including a transconjunctival incision,an oral incision,and a temporal incision,for complete release of the midface soft tissues,allowing the surgeon to remove redundant skin from the scalp instead of the lower eyelid.The midface lift allows the midface tissue to be fixed in a direction opposite gravity,thus reducing the tension between the tissues.There is also less damage to the structural anatomy,which does not cause additional scarring due to donor-site excision.Moreover,there is a lower risk of inflammation and exposure caused by implantation.Min27compared cases of lower eyelid retraction caused by facial paresis using different suspensions and midface lifts and found that the midface lift group showed the greatest change in the ratio between the distance from the pupil center to the eyelid margin on the paralyzed side and that on the normal side.They believed that midface lifting was an optimal method for improving paralytic lower eyelid retraction.North28also pointed out that increased tissue manipulation may cause eyelid malposition in patients with complex trauma.
6.Correction of eye position
Hirmand29used a Naugle exophthalmometer to classify proptosis based on the degree of eye prominence.Based on these measurements,they were classified as deep-set eyes(protrusion ≤14 mm,type I),normal eyes(15–17 mm,type II),moderately prominent eyes(18–19 mm,type III),and very prominent eyes(≥20 mm,type IV).
The protrusion of the most anterior aspect of the globe past the malar eminence creates a disproportion between the bony support,soft tissues,and the eye,which is defined as a“negative vector”relationship.29This can be due to various factors,including thyroid-related eye disease,orbital space-occupying lesions,myopia,and age-related recession of the maxilla.Lower blepharoplasty with excessive eyelid tightening may further exacerbate lower lid retraction.When the degree of eye prominence is measured as type III or IV,the patient may be considered to have a“negative vector”relationship.
Most cases of prominent eyes are due to thyroid eye disease(TED)and Graves’ orbitopathy.Other possible causes include severe myopia,congenital shallow orbit,inflammatory orbital disease,and orbital tumors.In patients with TED,prominent eye is caused by augmented orbital soft tissue associated with fibrosis of the vertical retractors.
Scleral ectropion and lower lid retraction in patients with severe proptosis are best treated by reducing the protrusion.From a mechanical perspective,changes in the axial position of the globe may affect the position of the lower eyelid.In short,the curved protruding surface of the globe tends to push the eyelid forward,widening the palpebral fissure and exposing the sclera.Similarly,correction of prominent eyes could be sufficient to reverse lower lid retraction.Ma showed that lower eyelid retraction with coexisting entropion is attributable to the unique anatomical features of patients of East Asian ancestry.By building a numerical model of biomechanics to analyze von Mises stress and displacement at the lower eyelid,they found that,for the same pressure,East Asians experienced greater pressure on the eyelid margin,resulting in more displacement.30For patients with exophthalmos secondary to TED,blepharoplasty techniques that deal only with soft tissue can be effective in concealing the prominent eye but are more likely to fail if the underlying globe or orbit dystopia is not corrected.Fat decompression is a good option for patients with TED as their orbital fat is augmented;however,it is not recommended for non-TED patients.
Bone decompression is also an ideal surgical option and can involve single or multiple walls of the orbit depending on the patient’s desired outcome,such as proptosis reduction or globe displacement.Surgical techniques for orbital decompression include eyelid crease lateral-wall decompression,transconjunctival inferolateral-wall decompression,transcaruncular medial-wall decompression,or a combination of these.Previously,orbital decompression and lower eyelid retraction correction procedures were performed separately in staged operations.Taban et al.31showed that in patients undergoing combined orbital decompression and lower eyelid retraction surgery with or without Graves’orbitopathy,the position of the lower eyelid improved regardless of the cause of the lower lid retraction and proptosis or type of orbital decompression procedure used.The combined procedure can reduce the total number of procedures,patient anxiety,recovery time,and costs without compromising results.
7.Our work:DOS flap
As a review and summary of the work above,compensating for the lost tissue of the lower eyelid and correcting the force imbalance are important parts of the correction of lower eyelid retraction.The upward suspension of the relevant tissues in the treatment can achieve both goals.Previously,the tissues used for suspension were the orbicularis oculi muscle and SOOF,but these two are not tough enough,and fixation of the suspension is prone to loosening and dislodging.Our team had varying degrees of under-correction or recurrence in previous cases.Obtaining relatively tough tissues,such as autologous tendons,will result in an additional surgical area with donor area damage.In contrast,suspension with alloplastic material may involve the risk of material exposure due to the thin eyelid tissue.
We considered whether it is possible to directly suspend the dermal tissue on the lateral side of the lower lid.The dermal tissue is tough enough;therefore,the suspension is direct and strong,and the sutures are in direct contact with the connective tissue on the bony surface,which will form a strong adhesion that will not easily loosen.
In patients with lower eyelid retraction who have intact orbicularis muscle and lateral orbital periosteum,without an obvious middle lamellar scar,a semicircular area of approximately 10 mm in diameter is designed at the level of the external canthus before the surgery.An incision is made along the preoperative semicircle to remove the upper epidermal tissue.Subsequently,a DOS flap is created.The orbicularis retaining ligament(ORL)is then separated upward under the orbicularis muscle,which is the fibrous connective tissue over the lateral bony surface.The flap is fixed to the ORL using a nonabsorbable suture.Local adjustments are necessary to correct the lower eyelid margin to its normal position or to correct it by 1–2 mm.After firm suspension,the suture is threaded through the lateral upper eyelid skin(Fig.3).
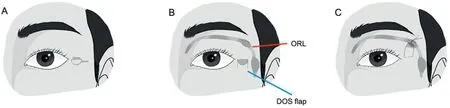
Fig.3.(A)Preoperative design.(B)The red line points to the ORL,and the blue line points to the DOS flap.(C)The DOS flap is suspended on the ORL.DOS,dermalorbicularis oculi suspension;ORL,orbicularis retaining ligament.
The DOS flap has two advantages.First,the incision is short.The surgery is performed using only a short incision;thus,the surgical area is small,giving a vertical lift to the lower eyelid margin to reduce the possibility of middle scarring.Second,the treatment mobilizes the midface skin simultaneously,eliminating the need for skin grafts.For patients with large tissue loss of the lower eyelid,even midface,the DOS flap could effectively reduce the amount of tissue replenishment(Fig.4).
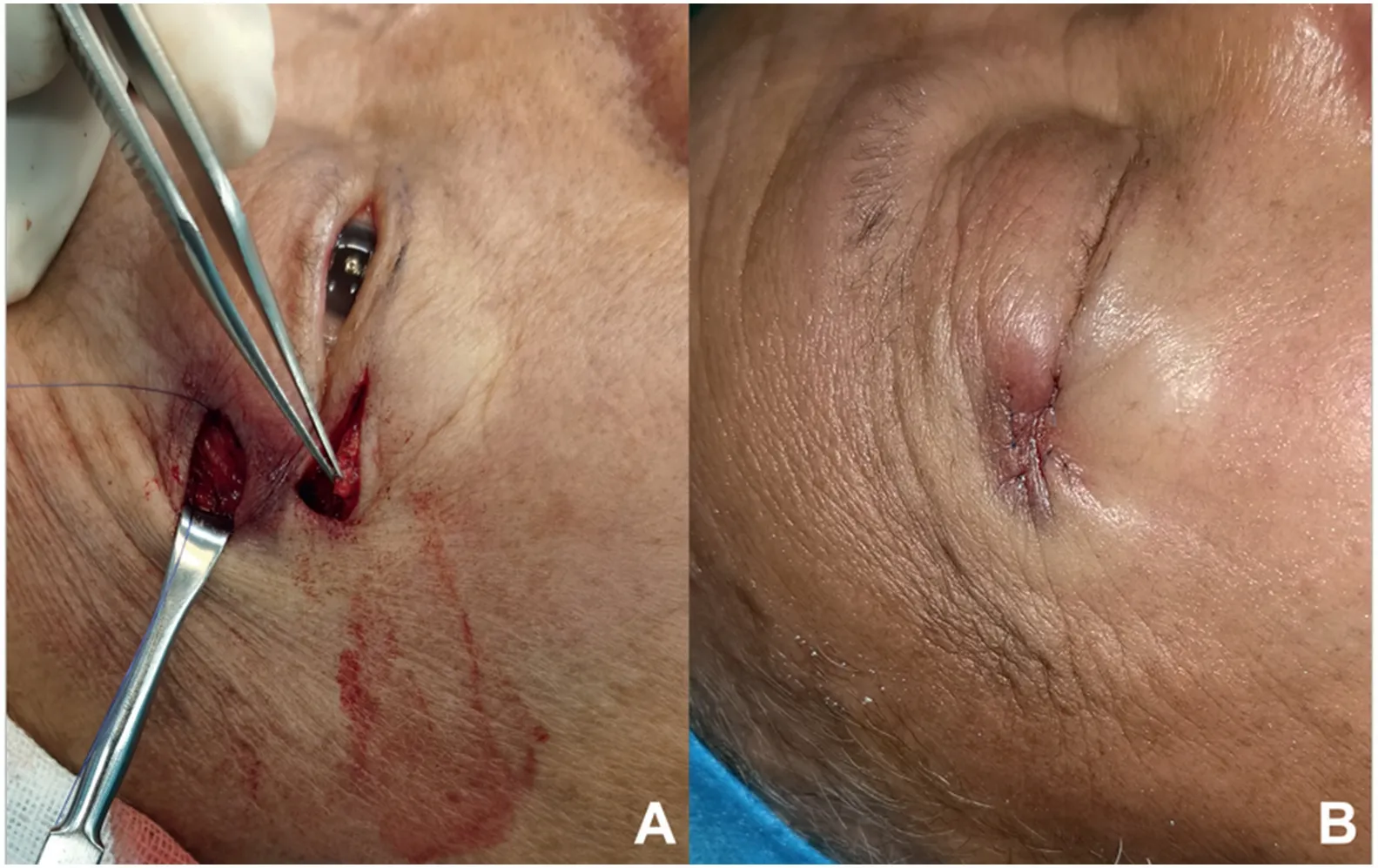
Fig.4.(A) The DOS flap.(B) The eyelid postoperatively.
As the flap is suspended from the superficial tissue to the deeper tissue,there may be an obvious depression at the skin incision area during the early postoperative period,which may cause a poor appearance;however,this will gradually recover later.We attempted this technique on 16 cases with a maximum follow-up of one year.All patients were satisfied with the results.No recurrence was observed after surgery (Fig.5).However,more cases need to be treated with this technique and longer follow-up times are needed to further understand this DOS flap.

Fig.5.Appearance of the eyelid at preoperation (A–C),postoperation (D,E),and 3 months after the operation (F).
8.Conclusion
Lower eyelid retraction is a complication of lower blepharoplasty that may cause tearing,dry eye,ocular irritation,corneal scarring,exposure keratitis,and even corneal ulcers.According to the causes of lower eyelid retraction,different suspensions,lateral canthal anchoring,midface lifting,injections of autologous fat and hyaluronic acid,spacer grafts,full-thickness skin grafts,local myocutaneous flaps,and correction of eye position are all effective methods to solve lower eyelid retraction.In clinical practice,single or multiple methods are often chosen for different causes of lower eyelid retraction.The DOS flap that we developed has enough upward traction,which can effectively correct lower eyelid retraction for different reasons.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained in this study.
Competing interests
The authors declare that they have no competing interests.
Authors’contributions
Ding Y:Writing-Original draft,Visualization.Huang X:Investigation.Lu L,Jin R,and Sun D:Validation.Yang J:Supervision,Project administration,Funding acquisition.Luo X:Conceptualization,Methodology,Writing-Review and Editing,Supervision,Project administration,Funding acquisition.
Acknowledgments
The study was sponsored by the Natural Science Foundation of Shanghai (grant no.19ZR1430100) and the National Natural Science Foundation of China(grant no.81871576).
 Chinese Journal of Plastic and Reconstructive Surgery2022年1期
Chinese Journal of Plastic and Reconstructive Surgery2022年1期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Androgen-related disorders and hormone therapy for patients with keloids
- Prospective application of poloxamer 188 in plastic surgery:A comprehensive review
- Using the parietal branch of superficial temporal vessels:A good approach to total ear replantation
- Misdiagnosis of malignant meningioma in subcutaneous soft tissue of the forehead:A case report
- Polyacrylamide gel migration after injection for breast augmentation:A case report
- External application of a Nocardia rubra cell wall skeleton in the treatment of diabetic foot ulcers
