Epidemiology of Pemphigus: A Single Center Experience in Morocco
Farah El Hadadi∗, Line Mezni, Karima Senouci, Laila Benzekri, Nadia Ismaili, Mariame Meziane
Department of Dermatology-Venereology, Ibn Sina University Hospital, Mohammed V University, Rabat 10100, Morocco.
Abstract
Keywords: pemphigus, epidemiology, Rabat, Morocco, autoimmune bullous disease, desmoglein
Introduction
Pemphigus is a group of IgG-mediated autoimmune diseases of stratified squamous epithelia where acantholysis causes blisters and erosions. Many subtypes exist:pemphigus vulgaris (PV), pemphigus vegetans (P Veg),pemphigus erythematosus (PE), pemphigus foliaceous(PF), pemphigus herpetiformis (PH), pemphigus IgA,and paraneoplastic pemphigus (PP). They are classified according to the clinical phenotype, histological features and autoantibody profile (desmoglein 1 or 3). The incidence of the disease varies from 0.5 to 34cases/million inhabitants/year, with the highest incidence rates in Brazil.1In Tunisia, the incidence is 0.67/100,000 population,2in Saudi Arabia (0.16/100,000)3and 0.18/100,000 in France.4In North America,Europe,and Asia most cases of pemphigus are sporadic, but higher incidence were noticed in Jerusalem with an estimate of 1.6 per 100,000 populations per year.5In USA, the crude prevalence of PV is 6.1/100,000 inhabitants for a total population of 29,396,600.6Brazil presents the highest incidence of PF worldwide as 25–35cases/(million year)7followed by Tunisia of 6.7cases/(million·year).
In Rabat,which is the capital of Morocco,10 new cases of pemphigus are diagnosed every year for a population of 577,827 inhabitants.8While in Marrakech,the prevalence of 10.4 new cases per year has been noticed,9and approximately 20 new cases are recorded in Egypt per year(Cairo University hospital records),15 new cases in Jordan per year,and 10 new cases in Mauritania.10The aim of our study was to describe the epidemiological and clinical characteristics of the disease, which provides epidemiological reference to the disease prevention and control.
Methods and materials
Patients
All medical files of the cases with pemphigus at the Department of Dermatology in the Ibn Sina University Hospital of Rabat, Morocco, from January 1990 to December 2020 were collected, retrospectively analyzed,and the following epidemiological and clinical data were retrieved:age at diagnosis, gender, origin, mean duration of the disease,cutaneous and oral involvement,bedridden duration, mortality rate, treatment modalities, severity of the disease.The diagnosis of pemphigus was based on the clinical presentation, results of histopathology, indirect and direct immunofluorescence.
The ethical approval for the study was obtained from the local Research Health Committee of the Ibn Sina University Hospital–Mohammed V University of Rabat.
Statistical analyses
As for the statistical analysis, frequencies were calculated to describe the characteristics that were studied. Adjustment to the chi-square statistic was used for testing the equality of proportions of different qualitative variables.The P-values of 0.05 or less were considered to indicate statistical significance. The statistical analysis was conducted using SPSS version 20 (IBM Corp., Armonk, NY,USA). The incidence for pemphigus was calculated using the population projections for Morocco produced by the High Commissioner for Planning.
Results
Totally data of 302 pemphigus patients were included during the 30-years study period (1990–2020), and the Figure 1 resumes the incidence of new pemphigus cases through the years. An average of ten newly diagnosed cases occurred in the Rabat-Salé-Kénitra region, with 26 new cases in 2020. The average annual incidence was estimated to be 0.32/million populations. In 2020, the incidence increased from 0.04 in 1995 to 0.72 per 1 million populations, a peak that occurs simultaneously with the coronavirus disease 2019 pandemic.The prevalence of the disease for the general population at the end of the study period was 1.56/100,000.
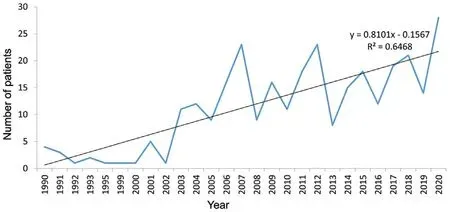
Figure 1. Temporal distribution of pemphigus cases through the years.
For the sex distribution, the female-to-male ratio was 0.75(173 females,129 males;P<0.001).The average age at diagnosis was (53±14.9) years old, the oldest and youngest patient was 95 and 18years old,respectively.The median age for men was 53years and was not different from the age of onset in females.
For the geographic distribution, since all cases of pemphigus were seen at the Department of Dermatology of Ibn Sina University Hospital and,due to the distribution and decentralization of health care in Morocco, most of our cases were from Rabat, 53 patients with PV were originally from Rabat followed by 47 cases with PE.Figure 2 shows the different distribution of pemphigus cases according to their origin.Most of our patients were referred by dermatologists practicing in the private or public sector (42%), followed by general practitioners(31%). Twenty-four percent of patients consulted in the emergency room and 3%were referred by dentists mainly PV with oral mucosal involvement.
The mean duration of the disease before diagnosis was 13.36months. Clinical forms were distributed as follows:50.3% with deep pemphigus (152 patients among 302 subjects,including 125 vulgaris and 27 vegetans)(Fig.3A and 3B); superficial pemphigus 45.7% (139 patients including 40 PF and 99 PE) (Fig. 3C); 3% of PH (nine patients) and two cases of PP. The Figure 4 resumes the number cases of pemphigus according to the clinical form.There was no significant difference between the ages of patients with PH,PV,and PE(50.0±5.0years).However,patients with PP were older(63.5years)while patients with P Veg were the youngest(42.4years).Both of two PP had hematologic malignancy (chronic lymphoid leukemia).Five percent (15 patients)had mucosal involvement only,while 45% of our patients had mucocutaneous involvement and 50%of our cases(148 patients)had a cutaneous disease. The assessment of the disease severity using the pemphigus disease area index score was as follows: 76%severe, 20% moderate, 4% mild. As for the bedridden duration it was 2.5months, the longest hospitalization period was noticed in a patient with PH(8.3months).The average hospitalization time per pemphigus subtypes was as follows: PP (3.0months) followed by PF and PH (2.6 months),PV(2.4 months),P Veg,and PE(2.2months each).
Fifty-five percent of our patients were treated with high doses of corticosteroids(1.5–2.0mg per kg of body weight per day) with a progressive tapering while 45% of the patients were treated with corticosteroids associated to other treatments: 37% with immunosuppressive therapy(Azathioprine is the main sparing-agent used in 99 patients, nine patients received Rituximab), the combination of steroids and dapsone were used in 7% of patients mainly those with PE.
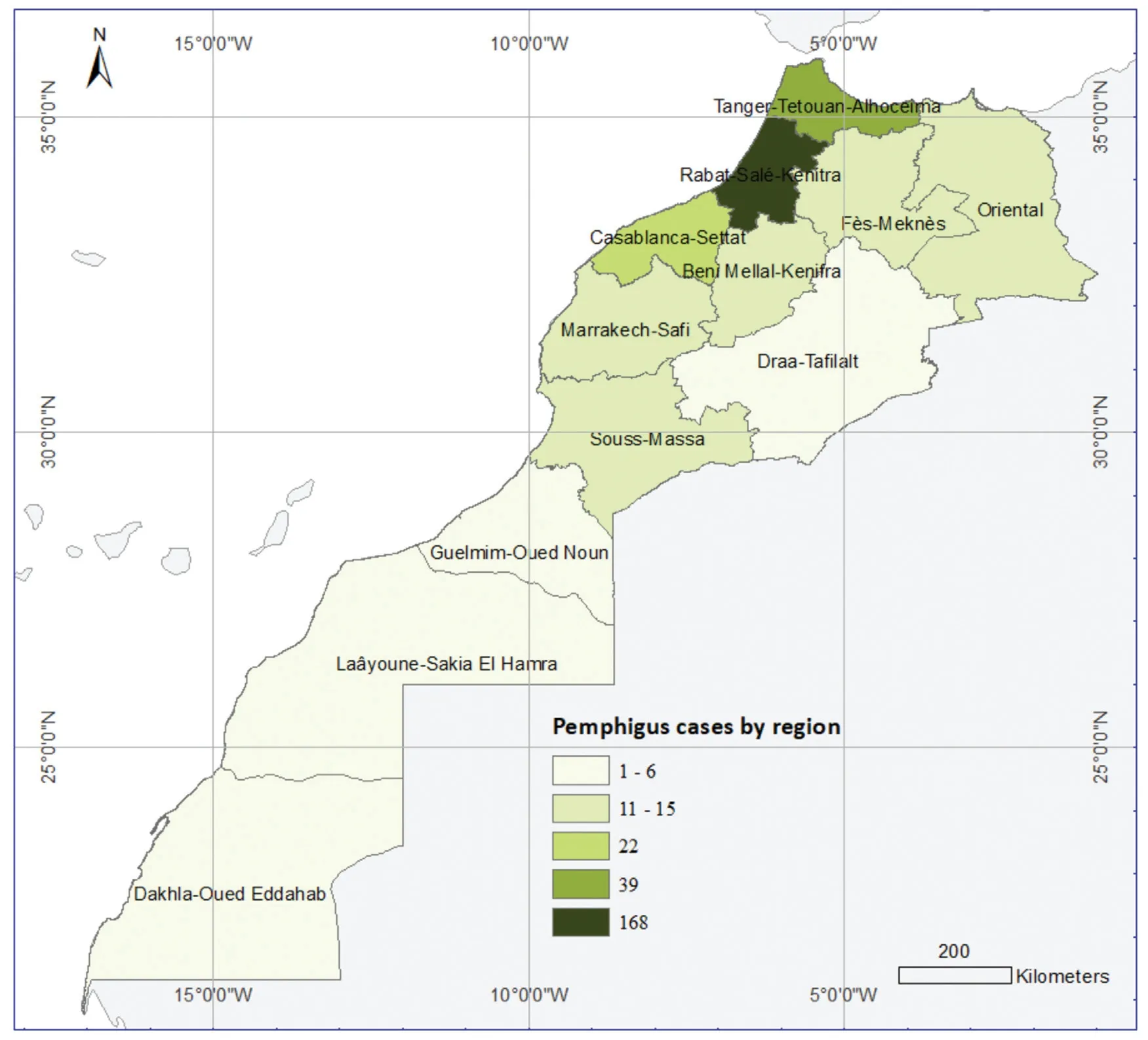
Figure 2. Spatial distribution of pemphigus cases from dermatology department of Ibn University Hospital of Rabat.
During the follow-up period,10.9%of our patients died(33 patients), the mean age of death was 53.3years,and there was no difference between genders (17 males,16 females). The causes of death were: an important extension of the disease (severe pemphigus disease area index) in 16 patients, local or systemic infections(23 bacterial infections, seven viral infections, one case of pulmonary infection by Strongyloidiasis), vascular complications in 4 cases,a molar pregnancy in one patient,one case of PV with leukemia and unknown causes in five cases. No proven case of drug-related pemphigus was found. Patients with PV were the most concerned (28 patients)followed by two patients with PE,P Veg and PP(one case each).
Discussion
PV affects persons of all races but increases incidence in patients of Ashkenazi Jewish descent and those of Mediterranean origin.This can be due to different genetic susceptibilities and/or exposure to different environmental risk factors.In Morocco,pemphigus is associated with two HLA haplotypes (DR4–DQ3 and DR14–DQ5), this genetic predisposition was well demonstrated in Brick et al study,11where a significant increase was found in DRB1∗04, DRB1∗14, and DQB1∗03 allele frequencies and a significant decrease in DRB1∗15 and DQB1∗06 allele frequencies. The authors concluded that HLADRB1∗15–DQB1∗06 haplotype seems to confer a protective effect in the Moroccan population while DRB1∗04–DQB1∗03 and DRB1∗14–DQB1∗05 haplotypes induced susceptibility to the disease. Higher frequencies of HLADR4-HLA-DQw8 were noticed in the Ashkenazy Jewish patients with PV.12As for the risk haplotype, results of case-control association studies of European,Western and Southern Asian, and North and South American populations of European and Western Asian ancestry showed thatDRB1∗04:02-DQA1∗03:01-DQB1∗03:02andDRB1∗14:54(14:01)-DQA1∗01:04-DQB1∗05:03(or DQB1∗05:02 in Iran and Japan)are commonly associated with increased PV.13Besides the genetic susceptibility, other welldocumented events may trigger the disease such as physical agents (ultraviolet or ionizing radiation, thermal or electrical burns,surgery and cosmetic procedures),contact allergens(eg,organophosphate pesticides),dietary factors(eg,garlic,leek,onion,black pepper,red chili pepper,red wine, tea), and emotional stress.14In Morocco, chronic sun exposure can trigger the disease,indeed we notice that most of our patients live in a rural environment and work as farmers and artisans.Another trigger is our Moroccan diet which is known to be rich in products of the allium group (garlic and onion, tea), in addition to our “scrub habits in the Hammam” using a traditional exfoliative glove.These cultural facts could explain the frequency of this pathology in the country. In Brazil, epidemiological features of FS indicate continued exposure to certain hematophagous insect bites as a possible precipitating factor of the disease.15

Figure 3. Clinical presentation of various type of pemphigus.(A and B):Pemphigus vulgaris with mucosal(A)and cutaneous involvement(B).(C) Pemphigus erythematosus: erosions and blisters are mainly located in the seborrheic regions.

Figure 4. Distribution of patients according to the clinical forms of pemphigus.PV:pemphigus vulgaris;PVeg:pemphigus vegetans;PE:pemphigus erythematosus; PF:pemphigus foliaceous; PH:pemphigus herpetiformis: PP: paraneoplastic pemphigus.
Because of its cutaneous and oral involvement, PV is a potentially life-threatening autoimmune mucocutaneous disease with a mortality rate of approximately 5%-15%.16In fact, mortality among pemphigus patients is 2.4-times greater than for the general population mainly due to infections.17Morbidity and mortality are closely related to the disease activity score,high dose of corticosteroids,age of the patients (elderly), and infections. In our study,mortality was associated to the type of pemphigus(vulgaris, PP), vascular complications, infections (pneumonia, sepsis), high dose of corticosteroids, the delayed consultation time (13.43 months), and the history of the patients (cardiac disease in five patients). In the study of Belgnaoui et al.18the high mortality rates were mainly linked to infections, the presence of pre-existent diabetes,and the combination of oral steroids with immunosuppressive therapy. In France, the high mortality rate was mainly related to the old age of patients (median age at death of PF 87.4 years and PV patients 82.4years).4In the study of Baum et al19in Israel,out of 290 patients with PV;20 died.The causes of death were pulmonary disease(chronic obstructive pulmonary disease and pneumonia)in four cases, malignancy in three cases, cardiac disease in two cases,cerebrovascular accident in one case,and other or unknown causes in six cases.19None of the mortalities were found to be directly related to pemphigus disease with no statistically significant difference in the severity score was found between males and females,age at presentation(<40 vs.≥40years),or between Ashkenazi and Sephardic Jews.However,men and Sephardic Jews tended to have a more severe level of disease at presentation.
In Morocco,the average age of onset is 48±3years,with some variability between Universities (Rabat: 53years,Casablanca: 47years and 53.8 in another study,20-21Fès:47.8 years,22Marrakech:44.4years).Table 1 resumes the different Moroccan studies published by now. In the Maghreb, the disease affects the fifth decade(eg, Tunisia,Egypt). A younger age at onset was reported in Kuwait(36.5years),Iran (mean age of 38years in one study, and 43years in another), Saudi Arabia (43.1years), in Brazil(41.5years). In European countries, such as France, the average age is almost the same to our study,ie,50years)as well as in USA (50years). Surprisingly, in other countries the PV usually develops at an older age, as shown by studies from Sicily,Italy(56years),23the UK(median age of 71years).24In Japan,the disease affects elderly patients(60–69years old).25In general,age at onset appears to be higher in northern European countries compared to Middle Eastern, Asian, and African countries. Several theories have been put forward to explain this observation,some authors suggested that it was related to demographic variability (fertility rates, life expectancy, birth rates),some to migration, while others to geo-epidemiological changes in PV characteristics.
For the gender and the sex specific prevalence;even if we didn’t find any specific difference between gender, it has been demonstrated that–as many auto immune diseases–pemphigus has a female predominance, the difference of pemphigus in gender is not well understood and the correlation between disease severity activity and gender is unknown. In Morocco, the female to male is 1.8:1, this was evidenced by the different studies published in the country:1.8 in Casablanca;3.6 in Marrakech,and 1.12 in Fès.These data join the epidemiological studies conducted in Iran,Turkey,26South Africa,27Kuwait,28China,29and most European countries.30The gender specific auto immunity can be explained by hormonal,immunological,microbiomial,and genetic theories(specific genes encodedon the X chromosome). Sex hormones (oestrogens,progresterons) are reported to affect the susceptibility to autoimmune disease with a severe activity disease during pregnancy and relapses in the postpartum period while testosterone has a protective effect on the immune system.
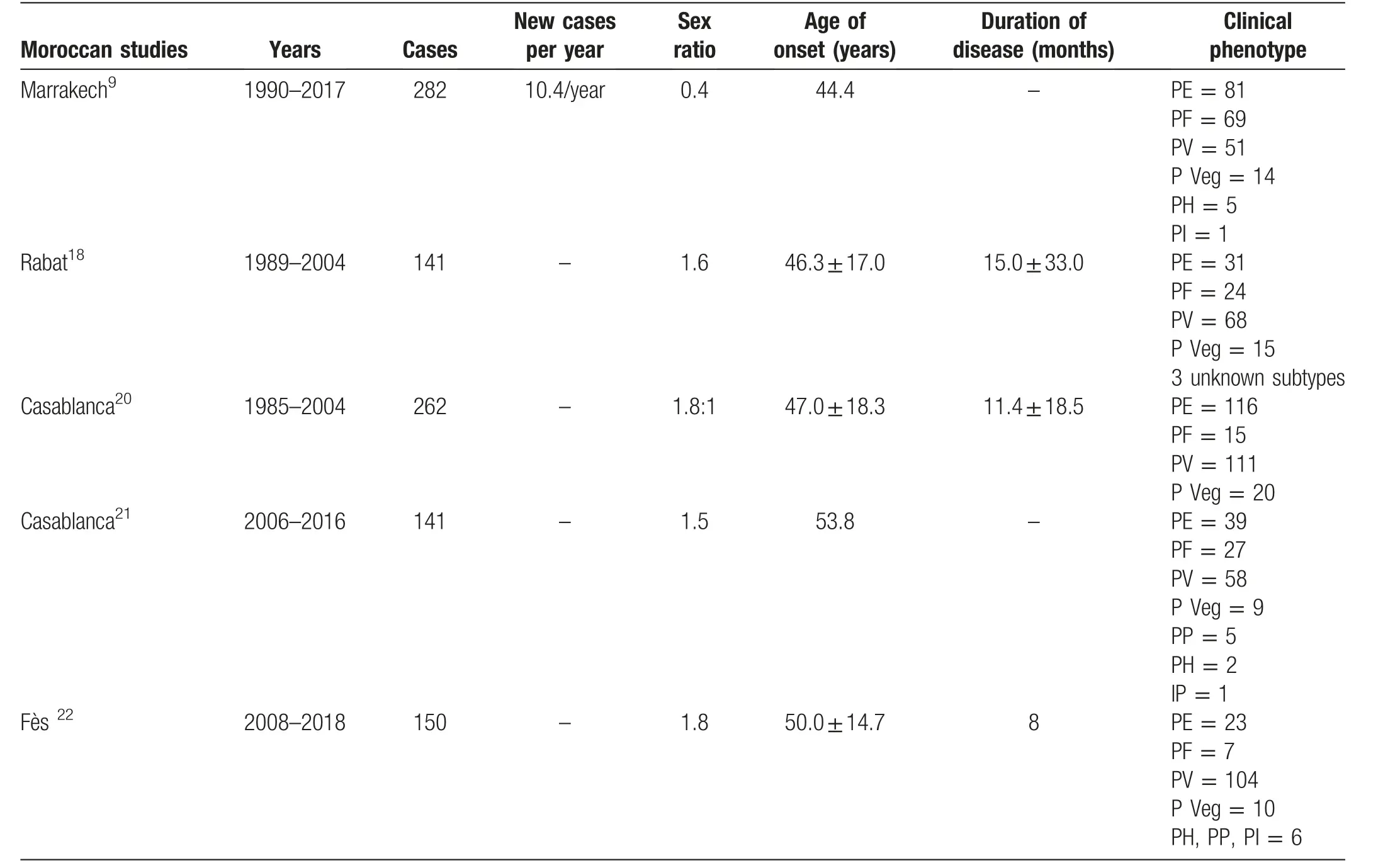
Table 1 Reported cases of pemphigus in Morocco representative studies.
As for the geographic distribution, since our center is based in Rabat(capital of Morocco),most of our patients were from the region of Rabat Sale Kenitra, 53 patients with PV were originally from Rabat followed by PE(47 cases).However,these data are inconclusive and may constitute a selection bias.Indeed,due the distribution and decentralization of health care in Morocco, our department recruits patients from the region of Rabat Sale Kenitra. Other studies raised from different hospital care centers of the kingdom are therefore necessary to determine if there is a link between the clinical phenotype,HLA haplotype, and ethnic susceptibility among Moroccan pemphigus patients.
The mean duration of the disease before diagnosis varies according to studies:13.36months in our study vs.(11.4±18.5) months in the Benchikhi et al in Casablanca.20The delayed time consultation in our country may reflect the difficulties to access medical services and health care centers, a low socio-economic level and can be related to some cultural and mystical-religious beliefs such as consultation of herborists, diviners, but also the non/mis-diagnosis by some general practitioners or other medical specialists;thus,resulting in diagnosis of moderate and severe forms.
From a clinical point of view,deep forms of pemphigus were as frequent as superficial forms in our study.PV was the most frequent form 50.3%, these data are similar to another Moroccan study in Casablanca, also in Algeria(unpublished data), reflecting a similar distribution as in our series.While in Tunisia PV was the most frequent form(61.0%),also in Kuwait(48.0%),France(62.2%),Korea(62.7%),higher rates have been observed in Iran(91.2%)and Saudi Arabia(94.7%).In our study,in the superficial subtypes of pemphigus:PE was predominant 71.2%with less cases of PF (28, 8%). When the clinical subtypes of pemphigus were compared according to gender,there was not a significant higher prevalence in women vs. men.However, we noticed that the superficial forms affected elderly patients then the deep forms (54.74years vs.48.79years), same statistics were found in France,where the mean age of PF was (61.3±20.4) years, while that of PV was (57.5±17.3) years.
In Brazil, two forms of PF have been described: a sporadic one, known as Cazenave’s PF, with worldwide distribution, and an endemic one related to certain geographic areas,known as Fogo Selvagem.The difference between both presentation forms of PF is its epidemiology.FS is endemic in Brazil, affecting young adults living in rural areas, neighbors, and family members. Colombia,Venezuela, and Tunisia are also countries where PF is endemic.However,the incidence of PV has been exceeding PF since 1998.
As for the bedridden duration, 3.0months was the longest hospitalization period in patients with PP, the average time was 2.5months, compared to 2.9months in Iran and 6.4months and 4.8months in other studies.The differences in treatment (local skin nursing care, use of immunosuppressive therapies)but also the access to social health insurance in various countries may be the main cause of different bedridden durations. In our study, the total cost for a period of hospitalization of 2.5months(time necessary for a complete remission) corresponds to 22,000-50,000 Moroccan Dirham depending on the social security, for an average salary in Morocco in 2019 of 2,368 Moroccan Dirham(222.38 €)which is;therefore,a significant non-negligible investment.
The main limitations of our study are: the one center study,the retrospective design,and the absence of dosage of the anti-desmoglein antibodies in our country. A multicenter study based on the demographic profile and genetic analysis is, therefore, necessary to understand the epidemiology of pemphigus in our country.
In conclusion,pemphigus is the most common blistering disease and the main cause of hospitalization in our department. The lack of epidemiological studies in our country prompted us to contribute in this field knowing the limitedimpactofitduetoouronecenterresearch.However,this epidemiological analysis can be seen as a baseline one to be deepened by further studies. On the other hand, this researchmaybeused forcomparativeonesatdifferentlevels(methodology, results). It also represents a solid database for further multicenter studies and can therefore be used to establish a national protocol for the management of pemphigus.The outcome in fine is to contribute to a better knowledge of the disease for a suitable care.
Acknowledgment
The authors thank El Hatimmy Faiçal for the statistical analysis.
- 国际皮肤性病学杂志的其它文章
- Prevalence of Acne Inversa (Hidradenitis Suppurativa) in China: A Nationwide Cross-Sectional Epidemiological Study
- Cutaneous Manifestations of HIV/AIDS in the Era of Highly Active Antiretroviral Therapy:Evidence from Bangladesh
- Evaluation of Depression and Quality of Life in Patients With Psoriasis
- Nail Psoriasis: Treatment Options and Management Strategies in Special Patient Populations
- Concurrence of Merkel Cell Carcinoma and Squamous Cell Carcinoma in A Patient with Generalized Actinic Keratosis: A Case Report
- Bowen’s Disease on the Left Fifth Finger Successfully Treated with Photodynamic Therapy: A Case Report

