Cutaneous Manifestations of HIV/AIDS in the Era of Highly Active Antiretroviral Therapy:Evidence from Bangladesh
Mohammad Rafiqul Mowla∗, Mohammed Abul Manchur, A Q M Serajul Islam Toby Maurer
1Department of Dermatology and Venereology, Chittagong Medical College, Chittagong 4203, Bangladesh; 2Department of Microbiology, University of Chittagong, Chittagong 4331, Bangladesh; 3Department of Dermatology, Indiana University,Bloomington, IN 47405, USA; 4Institute for Global Health, University of California, San Francisco, CA 94110, USA.
Abstract
Keywords:Bangladesh,Chittagong,cutaneous,highly active antiretroviral therapy(HAART),human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)
Introduction
The year 2021 marks the 40th anniversary of the discovery of human immunodeficiency virus/acquired immunodeficiency syndrome(HIV/AIDS).Since American researchers identified the first case of AIDS in 1981,AIDS has rapidly spread worldwide and become a global public health problem.1Cutaneous manifestations are very common in HIV-infected individuals and are associated with significant morbidity. More than 90% of patients develop at least one skin or mucous membrane manifestation during the course of their infection.2Several studies have revealed a correlation between skin disease and the patient’s underlying immune status,3–9thus making diagnosis of certain skin conditions a valuable clinical tool in staging and predicting the progression of disease.The introduction of highly active antiretroviral therapy (HAART) has significantly decreased the prevalence of opportunistic infections, Kaposi’s sarcoma, and most inflammatory conditions.10Since the introduction of HAART,there has been a dramatic decrease in the incidence and severity of HIV-associated dermatoses that were commonly seen in the pre-HAART era.11However, HAART itself has bought about a series of additional skin problems, such as drug-related adverse reactions and immune reconstitution inflammatory syndrome-related skin disease.12-13Variations exist in the incidence, clinical heterogeneity,and severity of disease among different ethnic and racial groups. Environmental, cultural, or genetic backgrounds may explain these variations. Cutaneous manifestations may differ both qualitatively and quantitatively between tropical and temperate countries depending on the availability of HAART and the genetic backgrounds or prevailing microorganisms in different geographic regions;however,few studies have been performed to classify these diseases with consideration of ethnic and geographic variations.14There is a scarcity of published data in Bangladesh regarding the cutaneous manifestations in patients with HIV/AIDS. The main purpose of this study was to analyze the prevalence and clinical importance of cutaneous lesions in patients with HIV/AIDS to facilitate early diagnosis and prompt intervention and thus prevent complications.
Materials and methods
This descriptive cross-sectional study was carried out in the Antiretroviral Therapy Clinic at the Department of Dermatology and Venereology, Chittagong Medical College Hospital from 2017 to 2020. This study was approved by the ethics committee of institution(Approval number: CMC/PG/ 2016/346) from Chittagong Medical College Hospital,which is the oldest tertiary care teaching hospital in Bangladesh.
Patient selection
The inclusion criteria for this study were a positive result on two separate HIV tests by enzyme-linked immunosorbent assay [reactive tests were supplemented by a rapid test in two different methods as per the World Health Organization(WHO)guidelines],diagnosis of HIV/AIDS,and current treatment with HAART.
The exclusion criteria were mucocutaneous lesions other than those associated with HIV/AIDS; concomitant diabetes mellitus, asthma, or other immunosuppressive conditions or prolonged treatment with steroids/cytotoxic therapy.
Data collection procedure
Clinical work-up
A structured questionnaire was administered to all participants to ascertain their demographic characteristics and history of HIV testing.A standardized clinical history was recorded, and all participants underwent a full dermatologic examination, including WHO staging, as part of a comprehensive clinical evaluation.The dermatological examination was performed in daylight. Chronic mucocutaneous disorders were diagnosed according to their clinical manifestations.The oral cavity was carefully inspected. The intraoral examination was performed under supervision of an oral medicine specialist in a dental unit.Most dermatoses were diagnosed according to WHO case definitions.True years were considered for age determination because no fraction was taken. The following additional data were extracted from the patients’records:sexual orientation,intravenous drug abuse,blood transfusions,addictions,other diseases,and opportunistic infections.
Drug rashes were diagnosed when eruptions occurred within 1month of commencing a new drug,after exclusion of intercurrent sepsis. The diagnostic criteria for drug eruptions were as follows:the suspected drug was used in temporal relation to the symptoms, the mucocutaneous manifestations were typical for the suspected drug,and the eruptions improved after withdrawal of the suspected drug.
First-line antiretroviral treatment consisted of one nonnucleoside reverse transcriptase inhibitor plus two nucleoside reverse transcriptase inhibitors. All HIV-positive patients were given free access to HAART in Bangladesh.The patients’viral load was not determined for economic reasons.
Laboratory methods
When necessary,appropriate laboratory tests such as skin scrapings,pus swabs,and skin biopsies were performed to confirm the diagnoses. The clinical diagnosis was supplemented with laboratory procedures such as microscopic examination (potassium hydroxide preparation),the Venereal Disease Research Laboratory test, and the Treponema pallidum hemagglutination assay whenever applicable.Skin scrapings for mycology were performed to confirm diagnoses of tinea and pityrosporum folliculitis.Diagnosis of folliculitis and furuncles was only indicated for bacterial folliculitis,which was confirmed by bacterial culture. A complete blood count, urinalysis, chest X-ray examination,and peripheral blood lymphocyte count were also performed. Hepatitis serology and viral marker measurements were done accordingly. Diffuse non-Hodgkin lymphoma was diagnosed by histopathological examinations of lymph nodes.
The HIV antibody status was determined using enzymelinked immunosorbent assay kits, and reactive samples were confirmed using western blot. CD4 cell counts were determined using a flow cytometer within 4hours of blood collection. All assays were performed using the methods recommended by the manufacturers. Each patient’s level of immunosuppression was classified according to the Centers for Disease Control and Prevention classification of the CD4 count and based on the WHO immunologic staging system as absent (>800 cells/mL), moderate(>500 cells/mL), or severe (<200 cells/mL).
Statistical analysis
The data were processed and analyzed using SPSS Version 21(IBM Corp.,Armonk,NY,USA).Descriptive statistical analysis was carried out by using frequencies and percentages.
Results
Of 40 patients with HIV/AIDS,22(55.0%)were male and 18(45.0%)were female.The patients ranged in age from 8 to 60years with a mean age of 38±0.966years.Among all age groups, the number of age-specific cumulative HIV/AIDS cases was highest at 19(47.5%)in the 31-to 40-year age group (Fig. 1). Most of the patients were migrant workers[22(55.0%)]with a low socioeconomic status[32(80.0%)], and the most common transmission mode was heterosexual activity[36(90.0%)].Eight patients(20.0%)had a sexually acquired coinfection, 12 (30.0%) had significant weight loss, 11 (27.5%) had a fever, and 10(25.0%) had persistent diarrhea (Table 1). Most of the patients [32 (80.0%)] had mucocutaneous disorders, 30(75.0%) had infective dermatoses, and 21 (52.5%) had non-infective inflammatory dermatoses. Eight (20.0%)patients presented with three or more skin disorders.The most common infective dermatoses were fungal infections[15 (37.5%)], followed by viral infections [8 (20.0%)],bacterial infections [4 (10.0%)], and scabies [3 (7.5%)].The most common non-infective dermatosis was generalized pruritus[6(15.0%)],followed by prurigo simplex[4(10.0%)], psoriasis [4 (10.0%)], eczema [3 (7.5%)],pruritic papular eruption (PPE) [1 (2.5%)], seborrheic dermatitis[1(2.5%)],urticaria[1(2.5%)],and xerosis[1(2.5%)]. The most common mucosal lesions were vulval lesions[5(12.5%)], followed by oral thrush [4(10.0%)],periodontal disease [2 (5.0%)], penile lesions [2 (5.0%)],and angular cheilitis[1(2.5%)](Table 2).Patients treated with HAART had decreased rates of oral candidiasis and herpes simplex but increased rates of drug reactions [19(47.5%)]. The most common drug eruption following HAART was a morbilliform rash [11 (27.5%)], and the most common offending agent was nevirapine (Fig. 2).
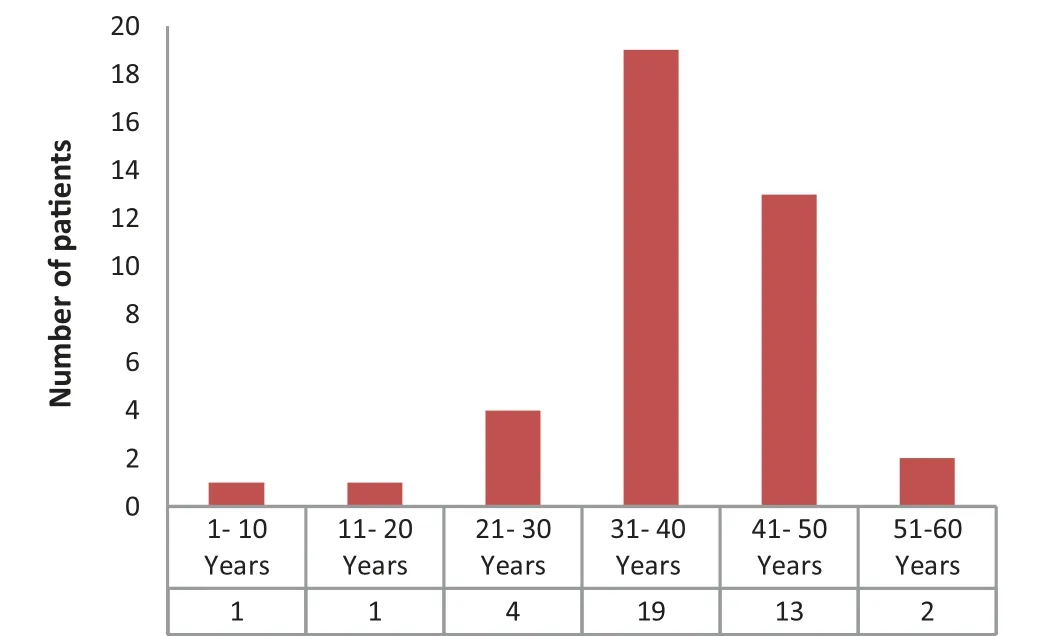
Figure 1. Age distribution of the HIV/AIDS patients (n=40). HIV/AIDS: Human immunodeficiency virus/acquired immunodeficiency syndrome.
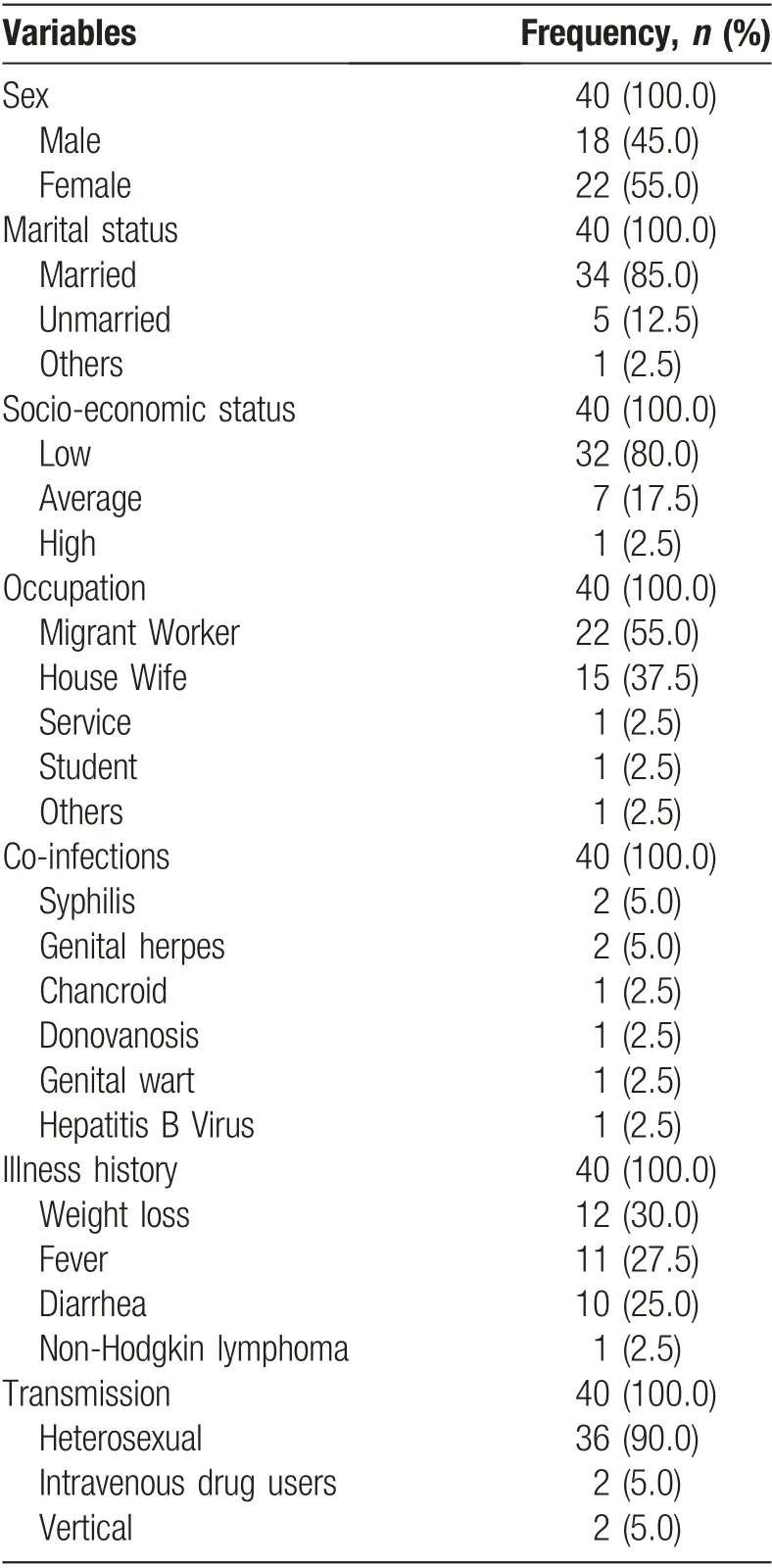
Table 1 Characteristics of patients included.
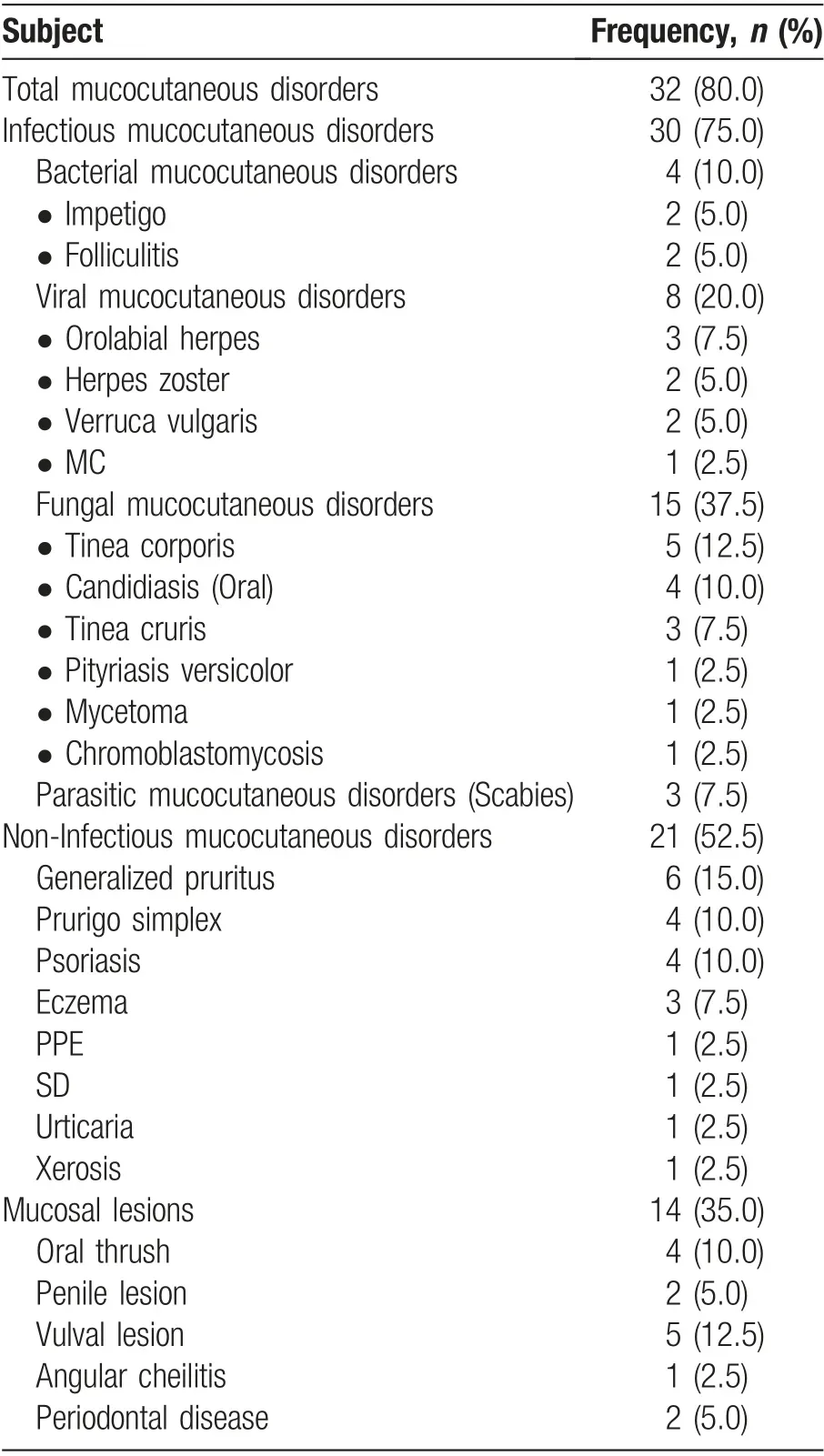
Table 2 Distribution of mucocutaneous disorders in HIV/AIDS patients.
Discussion
This descriptive cross-sectional study was performed to identify the pattern and prevalence of cutaneous manifestations in patients with HIV/AIDS in the HAART era because there are insufficient published data in this field in Bangladesh.

Figure 2. Distribution of drug reactions of HAART among HIV/AIDS patients. HAART: highly active antiretroviral therapy; HIV/AIDS:human immunodeficiency virus/acquired immunodeficiency syndrome.
The patients in this study ranged in age from 8 to 60 years,with a mean age of 38±0.966years.Among all age groups, the number of age-specific cumulative HIV/AIDS cases was highest at 19(47.5%)in the 31-to 40-year age group.This result is consistent with that reported by Han et al.1from China, who showed that the mean age was 39.64±11.79years. However, Brodt et al.15from Germany found that the median age varied from 37 to 38years.
Of the 40 patients with HIV/AIDS in this study, 22(55.0%) were male and 18 (45.0%) were female. Similar proportions of HIV/AIDS have been previously reported between the two sexes; Han et al.1from China reported that 225(64.66%)patients were male and 123(35.34%)were female, and Nnoruka et al.7from Nigeria reported that 320 (67.1%) patients were male and 157 (32.9%)were female. However, Chopra and Arora16from India reported a male:female ratio of 1.00:1.05, and Josephine et al.9from Cameroon reported that 236(61.5%)patients were male and 148 (38.5%) were female. This lower proportion of female patients could be due to stigma or shame and a reluctance to mention problems regarding sexually transmitted infections (STIs). Compared with men, women have symptoms for longer periods of time and seek treatment less often.Additionally,when women are economically dependent on men, they often have problems informing their partner of the disease and less often visit a health center without a male relative.
Most of the patients in this study were migrant workers[22 (55.0%)] with a low socioeconomic status [32(80.0%)], and the most common transmission mode was heterosexual activity [36 (90.0%)]. Two (5.0%)patients were intravenous drug users, and one (2.5%)patient was a commercial sex worker. The pattern of transmission of HIV in Bangladesh is mostly heterosexual;that is,sexual activity involving sex with female and male sex workers and between married couples.Homosexuality is rather rare in Bangladesh.Migration for work abroad is very common in Bangladesh. Men who stay away from their homes for prolonged periods may practice risky behaviors that make them more vulnerable to HIV/STIs.In this study,most of the female patients had become infected by their husbands.Return from working in a high-prevalence country is one of the ways HIV is introduced into lowprevalence countries. Available data show that the HIV epidemic is still at a relatively low level and concentrated mainly among intravenous drug users in Dhaka city.17

Figure 3. Cutaneous disorders in patients with HIV/AIDS in the era of HAART. (A): Morbiliform rash in a HIV/AIDS following HAART;(B): Molluscum contagiosum in a HIV/AIDS patient. HAART: highly active antiretroviral therapy; HIV/AIDS: human immunodeficiency virus/acquired immunodeficiency syndrome.
Eight (20.0%) patients with HIV/AIDS in this study were co-infected with other STIs. These co-infections included syphilis in two patients(5.0%),genital herpes in two(5.0%),chancroid in one(2.5%),donovanosis in one(2.5%),genital warts in one(2.5%),and hepatitis B virus in one (2.5%). Co-infections with STIs are prevalent among people living with HIV/AIDS.18Such co-infections pose considerable health threats to people living with HIV.Multiple co-infections with STIs are common because the pathogens share the same transmission routes and can have a multiplicative impact on the health of patients with HIV infection. Co-infections with STIs can compromise the health of HIV-positive individuals in various ways.
In the current study, 34 (85.0%) patients were treated with the Lamivudine+Zidovudine+Nevirapine regimen,four (10.0%) were treated with the Lamivudine +Zidovudine + Efavirenz (EFV) regimen, and one (2.5%)was treated with the EFV + Emtricitabine + Tenofovir regimen.Only one(2.5%)patient did not receive HAART.The advent of HAART has enhanced long-term viral suppression, has decreased opportunistic infections, and has increased the quality of life of infected individuals.19However,long-term treatment with HAART is associated with substantial toxicity and adherence difficulties,which can lead to drug resistance.20There was a relatively high incidence of drug eruptions in this study, especially in patients receiving HAART. We observed 19 (47.5%)patients with drug reactions, the most common of which were a morbilliform rash[11(27.5%)](Fig.3A)followed by anemia with a morbilliform rash [3 (7.5%)], only anemia [2 (5.0%)], headache [1 (2.5%)], deafness [1(2.5%)],and myelosuppression[1(2.5%)].The offending drugs were nevirapine, efavirenz, and cotrimoxazole,which were used to combat bacterial opportunistic infections. These findings are similar to those of Han et al.,1who reported 31 cases of drug eruptions in patients receiving HAART; of these, 25 cases were caused by nevirapine,4 were caused by efavirenz,and 2 were caused by sulfonamides.HIV-infected patients are predisposed to developing drug eruptions because of their defective drug metabolism and altered immune function.21Drug eruptions in patients with AIDS are much more frequent than in those without AIDS.22
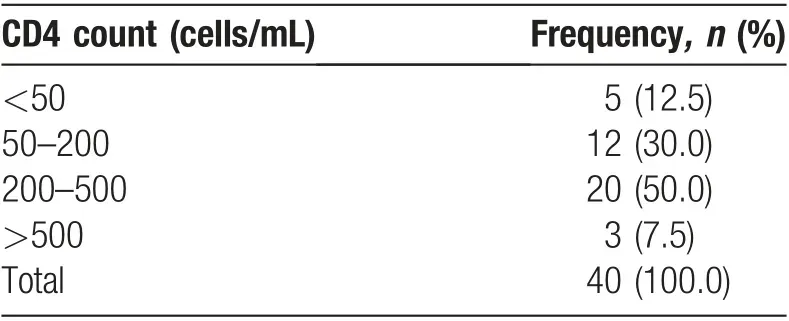
Table 3 Distribution of CD4 counts among HIV/AIDS patients
Most of the patients in the present study (80.0%) had mucocutaneous disorders. Infective dermatoses [30(75.0%)] outnumbered non-infective inflammatory dermatoses [21 (52.5%)]. There were 25 different types of mucocutaneous disorders associated with HIV/AIDS in the present study. Fifteen (37.5%) patients had one skin disorder, nine (22.5%) had two skin disorders, and eight(20.0%)had three or more skin disorders.Eight(20.0%)patients presented with no skin disorders. Patients with multiple and widespread cutaneous and mucocutaneous lesions had increased immunosuppression as noted by their CD4 counts (Table 3). Patients with less immunosuppression had more localized lesions and fewer diagnoses.16
The most common infective dermatoses were fungal infections [15 (37.5%)], followed by viral infections [8(20.0%)], bacterial infections [4 (10.0%)], and scabies [3(7.5%)]. Tinea corporis was the most common fungal infection[5(12.5%)],followed by candidiasis[4(10.0%)],tinea cruris [3 (7.5%)], pityriasis versicolor [1 (2.5%)],eumycetoma [1 (2.5%)], and chromoblastomycosis [1(2.5%)].With respect to viral infections, orolabial herpes occurred in three (7.5%) patients, herpes zoster in two(5.0%), verruca vulgaris in two (5.0%), and molluscum contagiosum in one (2.5%). Among bacterial infections,impetigo occurred in two(5.0%)patients and folliculitis in two (5.0%). Scabies was the only parasitic infection [3(7.5%)]. In a study from Nigeria by Nnoruka et al.,7dermatophytosis occurred in 24.3% of patients, whereas Chopra and Arora16from India reported a 3.33%incidence of dermatophytosis in their series. Although Chopra and Arora16reported a high prevalence of oral candidiasis (32.22%), the incidence of oral candidiasis in their study was only 10.0% (four patients). These differences might have been due to variations in the study design, recruitment of patients, environment, lifestyles of patients, and effects of HAART. Thrush is recognized as an early clinical marker of immunosuppression and an initial manifestation of symptomatic HIV infection.23In the present study, other oral lesions included periodontal disease [2 (5.0%)] and angular cheilitis [1 (2.5%)].Gingival and periodontal disease have recently been recognized as possible early presentations of HIV infection.24In general,oral manifestations are early indicators of HIV infection.
Among the fungal infections in the present study, one(2.5%) patient had eumycetoma and another(2.5%) had chromoblastomycosis. These were subcutaneous fungal infections, challenging clinical entities that become even more complex against a background of HIV infection.Therefore, it is not surprising that subcutaneous fungal and HIV co-infection manifest as different clinical presentations.This variation could be due to the profound immunosuppression of patients with HIV/AIDS.
In the current study, three (7.5%) patients presented with orolabial herpes and two(5.0%)with herpes zoster.These findings are consistent with other studies from different parts of the world. Han et al.1from China reported that 4.6%of patients had herpes zoster,whereas Chopra and Arora16from India reported that 13.33%of patients had herpes zoster. Herpes zoster and herpes simplex virus mucocutaneous infections are more frequent, chronic, and progressive in HIV-infected than immunocompetent persons.25The cutaneous lesions of zoster in HIV-positive adults can be dermatomal, multidermatomal,or disseminated.26The patients in this study had only localized dermatomal disease at all stages during the course of HIV infection.
One patient (2.5%) in this study had molluscum contagiosum (Fig. 3B); this patient was critically ill and was admitted to the inpatient department.Umoru et al.27from Nigeria also reported three (2.5%) patients with molluscum contagiosum in their study group. Although the typical lesions are pearly papules with central umbilication, atypical lesion such as giant molluscum contagiosum have been reported in patients with advanced HIV infection.28
In the current study, non-infective mucocutaneous disorders were present in 21 (52.5%) patients. Among non-infectious mucocutaneous disorders,generalized pruritus was the most common [6 (15.0%)] followed by prurigo simplex [4 (10.0%)], psoriasis [4 (10.0%)],eczema [3 (7.5%)], PPE [1 (2.5%)], seborrheic dermatitis[1 (2.5%)], urticaria [1 (2.5%)], and xerosis [1 (2.5%)].In a study from Thailand by Sivayathorn et al.,29the incidence of PPE was 32.7%,that of seborrheic dermatitis was 21.0%,and that of psoriasis was 6.5%.The incidence of PPE was also found in Indian and Chinese studies to be 7.77% and 5.75%, respectively. PPE is a unique dermatosis associated with advanced HIV infection and is characterized by sterile papules, nodules, or pustules with a hyperpigmented, urticarial appearance and pruritus.30The underlying etiology probably reflects a hypersensitivity reaction to insect bites in susceptible patients.31The prevalence rate of seborrheic dermatitis in patients with HIV ranges from 8% to 21% in India as reported by Chopra and Arora16and is only 1.15% in China as reported by Han et al.1
In the present study,two(5.0%)patients presented with paronychia, one (2.5%) with melanonychia, and one(2.5%) with nail dystrophy. Paronychia and nail dystrophy are associated with candidal onychomycosis in people living with HIV/AIDS due to immunosuppression and also lifestyle factors (eg, frequent hand washing by housewives).Melanonychia may be due to the use of ZDV.This is also supported by other studies.12,32
We also found that mucocutaneous abnormalities are more frequent and more severe as the immune status worsens. A significant proportion of patients with immunosuppression presented with more than one mucocutaneous lesion concurrently. Notably, however,the study population had a high prevalence of infective dermatoses,a high prevalence of generalized pruritus,and an absence of Kaposi’s sarcoma.
The major limitation of this study is that it was a crosssectional hospital-based study without a non-HIV-infected comparison group. The sample size was also relatively small.Because of their low educational level,some patients were unable to recall their history of skin diseases prior to HAART. Thus, the patients with HIV/AIDS who were included in this study may not reflect the true national scenario of Bangladesh. We recommend a further multicenter study of cutaneous manifestations in patients with HIV/AIDS.
In conclusion, a different clinical pattern was noted in this study than reported previously. A wide range of cutaneous disorders is observed in Bangladeshi patients with HIV/AIDS, and HAART has an impact on the spectrum of HIV/AIDS-associated mucocutaneous disorders. Such disorders are seen at every stage of HIV/AIDS and are often the initial presentation in most instances within our environment.Early detection of HIV optimizes the chemoprophylaxis for many opportunistic mucocutaneous infections. The presence of recurrent, chronic, and recalcitrant skin diseases should be regarded as a strong indication for HIV testing.Our findings stress the necessity to incorporate geographic aspects in future guidelines for classification of HIV/AIDS-related mucocutaneous diseases. There is a need for increased attention to the diagnosis and treatment of skin diseases affecting the quality of life of patients with HIV/AIDS.
- 国际皮肤性病学杂志的其它文章
- Prevalence of Acne Inversa (Hidradenitis Suppurativa) in China: A Nationwide Cross-Sectional Epidemiological Study
- Epidemiology of Pemphigus: A Single Center Experience in Morocco
- Evaluation of Depression and Quality of Life in Patients With Psoriasis
- Nail Psoriasis: Treatment Options and Management Strategies in Special Patient Populations
- Concurrence of Merkel Cell Carcinoma and Squamous Cell Carcinoma in A Patient with Generalized Actinic Keratosis: A Case Report
- Bowen’s Disease on the Left Fifth Finger Successfully Treated with Photodynamic Therapy: A Case Report

