Factors Associated with Diagnostic Delay of Pulmonary Tuberculosis in China*
XU Cai Hong ,ZHANG Xiao Meng ,LIU Yan ,HU Dong Mei ,XIA Yin Yin ,WANG Li ,and ZHANG Hui,#
Tuberculosis (TB) remains a major public health threat;approximately 10 million new TB cases are recorded worldwide,and more than 1.2 million deaths were caused by TB in 2019[1].The diagnostic delay presents a major obstacle to the control of the TB epidemic.This is a serious concern because each patient may infect 10–15 people each year,eventually creating a public health problem and even leading to economic difficulties[2].Ensuring universal access to quality-assured and early diagnosis of TB is critical to diminish transmission,avert deaths,and prevent TB infections,which can help countries move toward the elimination of the disease.
China is one of the countries with TB high burden,accounting for 8.4% of the global TB burden and 50% of the burden in the Western Pacific region[1-2].Considering the high TB burden and limited human resources,the passive case-finding(PCF) strategy has always been the main approach applied by the National Tuberculosis Programme(NTP) in China,which contributes > 95% of TB patients’ notification.Under the PCF principle,patients with symptomatic TB voluntarily visit healthcare facilities to seek medical care,and all patients with presumptive TB and confirmed TB should be referred to TB-designated medical facilities.Otherwise,cases undetected for a long time or late detection may worsen the disease,increase the mortality rate,and result in the sustained spread of TB in the community.
Identifying reasons for the diagnostic delay is important for the health system to discover methods of diagnosing and treating patients timely,thus reducing disease suffering and transmission.Information on diagnostic delay is also important for the evaluation and improvement of TB control programs.Some small-scale studies have reported that diagnostic delay varies significantly from around 30 days in Shanghai[3]to 71 days in Yunnan province[4].Factors attributed to diagnostic delay are also likely to vary because of different settings,poverty,non-residence,default health insurance,among others.However,nationally representative data are unavailable.We conducted a nationwide survey in 22 counties to evaluate the extent and risk factors of TB diagnostic delay within NTP in China.
This cross-sectional study used primary data collected from patients with drug-susceptible pulmonary TB.Individuals receiving treatment in facilities other than NTP were excluded.A multistage stratified cluster sampling was adopted.The stratifying factors were region (east/central/west)and residence (rural/urban).The sampling steps are summarized in Supplementary File 1 (available in www.besjourna.com).Assuming a diagnostic delay of 30%[5],relative precision of 0.2,and α error of 0.05,average cluster size of 50,between-cluster variation of 0.4,design effect of 4.36,and anticipating a nonresponse rate of 10%,the final sample size was 960,to be sampled from 22 clusters (Supplementary File 2,available in www.besjourna.com).
A structured questionnaire was developed,which addresses the health-seeking behaviors of patients with TB. The questionnaire collected the following information:1) demographic and socioeconomic variables,including sex,age,education level,area of residence,and economic activity;2) clinical profiles,TB category,sputum status at diagnosis,hospitalization,human immunodeficiency virus (HIV) infection status,and comorbidities,such as chronic nephrosis and chronic liver disease;and 3) insurance status and healthcareseeking experience,which means that patients with presumptive TB seek healthcare services in healthcare facilities.Written consent was obtained from each eligible patient with TB before enrollment.Informed consent and responses for children aged < 18 years were obtained from the accompanying relative.A face-to-face interview was performed by trained investigators.Diagnostic delay was defined as the time interval from symptom onset to confirmed TB diagnosis longer than 14 days[6].
Data were double entered and validated using EpiData (version 3.1 EpiData Association,Odense,Denmark).Analysis was conducted using STATA(version 12.1,copyright 1985–2011 StataCorp LP USA).Univariate and multivariate analyses were applied to analyze the risk factors associated with diagnostic delay.Variables withP< 0.20 in the univariate analysis were used in the stepwise (entry and removal probability of 0.05 and 0.10,respectively) multivariate logistic regression analysis.The association of predictor variables with dependent variables was assessed by using a 95%confidence interval (CI) and adjusted odds ratio(aOR).AP-value of < 0.05 was regarded as significant.
A total of 974 patients with TB were included in this study (Table 1).Among them,387 (39.7%) and 380 (39.0%) patients came from the Eastern and Western regions,respectively. Moreover,396(40.7%) patients were 45–64 years old,and 682(70.0%) patients were male.In addition,573 (58.5%)patients had primary and middle school education,641 (65.81%) were rural residents,and 810 (87.4%)were symptomatic.In total,728 patients were under the new rural cooperative medical scheme,accounting for 74.7%.
The median diagnostic time for all cases was 23(IQR 5–53) days.The mean diagnostic time was 37.1 ± 43.3 days,which was similar to results of previous studies in Shanghai and Yunnan provinces in China[4-5]. Compared with other developing counties such as India[7]and South Africa[8],in which the average diagnostic delay was 44–151 days,a shorter delay was recorded in China. The comparatively good results could be attributed to the determination and corresponding measures taken by the Chinese government to control TB,such as training of professionals,scaling up of laboratory equipment,and capacity building.However,594(61.0%) patients still experienced a diagnostic delay,and this was still a challenge of controlling TB.

Table 1. Socio-demographic characteristics of pulmonary tuberculosis patients in diagnostic delay survey in China,2017 (n=974)

Continued
Tables 2 and 3 showed the results of the univariate and multivariate logistic regression analyses.The odds of having a diagnostic delay were higher in patients from central (aOR=3.03,95%CI1.96–4.69) and eastern (aOR=1.69,95%CI1.24–2.31) regions than in those from the western region.Given the relatively good economic situation of patients with presumptive TB in eastern and central regions,they usually choose senior general hospitals as the first treatment facilities;however,recent studies have found that the ability of these hospitals to identify TB is not as sensitive as expected[9]because some general hospitals do not routinely perform TB-related laboratory tests.Therefore,presumptive TB cases are referred to TBdesignated hospitals for further TB-specific examination.The tortuous medical-seeking path increases the risk of diagnostic delay.
The odds of having a diagnostic delay were higher in rural residents than in urban residents(aOR=1.45,95%CI1.07–1.96).The Fifth National TB Epidemiology Survey showed that the rates of public awareness of TB in rural and urban areas were 51.7%and 63.4%,respectively[10];the lower awareness of TB in rural areas might lead to a longer diagnostic delay.By contrast,rural residents faced various barriers to access to timely TB diagnoses,such as the lack of diagnostic facilities,lack of quality services and trained staff,and poor economic situation.
The odds of having diagnostic delay were higher for patients with TB experiencing coughs or expectoration (aOR=2.20,95%CI1.48–3.28) than for patients with hemoptysis.This finding was mainly due to the current PCF strategy adopted in China,i.e.,once patients with presumptive TB present with TB-related symptoms,he/she will go to the healthcare institutions initiatively for medical consultation.However,this behavior depends on the patient’s awareness of TB and the seriousness of the symptoms.Previous studies have also shown that mild initial symptoms such as cough could prolongthe diagnostic time[3],whereas severe initial symptoms such as hemoptysis and bloody sputum could shorten the diagnostic time.As asymptomatic TB cases were mostly found through active case finding (ACF),such as health examination,patients were diagnosed at the early stage,which might shorten the diagnostic delay.
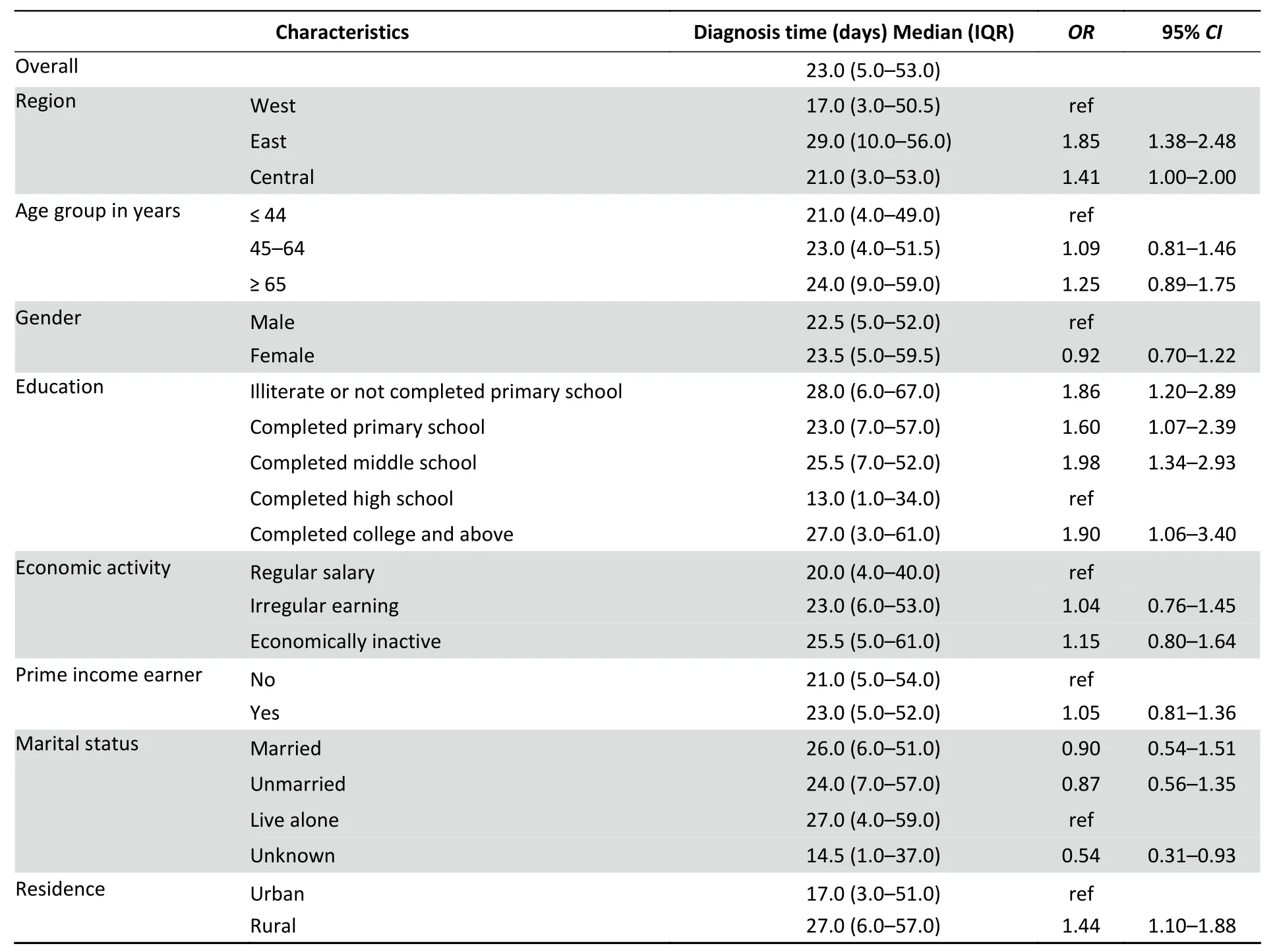
Table 2. Univariate logistic regression for factors associated with diagnostic delay among patients in China,2017 (n=974)

Continued
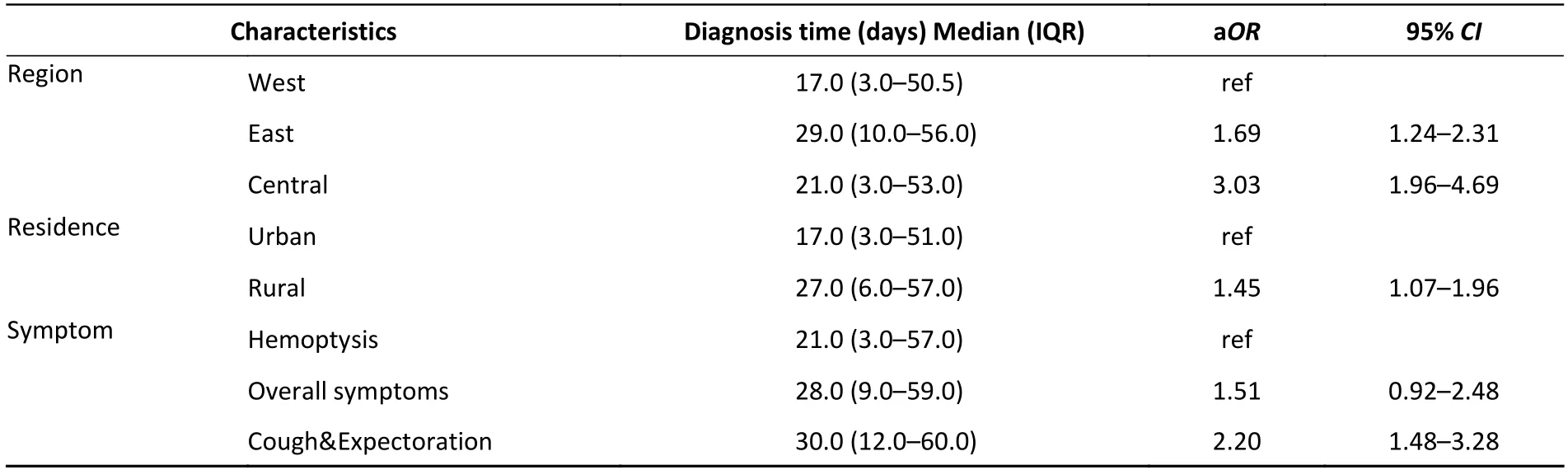
Table 3. Multivariate logistic regression for factors associated with diagnostic delay among patients in China,2017 (n=974)
The result of the univariate logistic regression analysis also suggested that patients without education or who have not completed primary school (OR=1.86,95%CI1.20– 2.89) or have completed middle school (OR=1.98,95%CI1.34–2.93) have higher odds of having diagnostic delay than patients who have completed high school.Among rural residents with TB,those with hospitalization history have higher odds of experiencing diagnostic delay than patients without hospitalization history (OR=1.35,95%CI1.03–1.77).The odds of having a diagnostic delay in patients registered in TB dispensary were higher than the value in those registered in TB-designated hospitals(OR=2.16,95%CI1.50–3.10).Sociodemographic factors such as age,sex,marital status,and type of medical insurance were not significantly associated with diagnostic delay.
The results of this study may have some important policy implications for TB control in China.To our knowledge,patients with TB are still predominantly passively identified in China,which relies heavily on the patient’s medical treatment behavior,so various approaches should be adopted to improve public awareness of TB and thereby reduce the patient delay.Besides the patient delay,the diagnostic delay includes health system delay,which is affected by the TB-recognizing ability of the doctors and the diagnostic capacity of the facility.Thus,improving the recognizing ability of TB symptoms by all healthcare workers,scaling up of rapid diagnostic tests,and optimizing the diagnostic algorithm are important to reduce the health system delay.In addition,China should gradually scale up ACF among high-risk groups,including close contacts of smear-positive TB cases,presence of HIV/AIDS,and those aged > 65 years.
In brief,this study presents a significant delay in TB diagnosis in China.Major factors associated with diagnostic delay are localization in central and eastern regions,rural residence,and being symptomatic.Multiple measures should be taken to shorten the diagnostic delay in view of the patient and health system and thus improve TB awareness of the public,scale up ACF in high-risk groups,and improve diagnostic capacity in economically lessdeveloped regions in the near future.
The study was approved by the Ethics Committee of the Chinese Center for Disease Control and Prevention [No.201625,dated 22 November 2016].
No potential conflict of interest was disclosed.
The authors would like to thank all supporters of Liaoning CDC,Henan CDC,Xinjiang CDC,Yunnan CDC,Fujian CDC,and Hunan Chest Hospital.
XU Cai Hong and ZHANG Hui conceived the study,LIU Yan and WANG Li supervised the survey,HU Dong Mei and XIA Yin Yin analyzed the data,XU Cai Hong and ZHANG Xiao Meng wrote the manuscript.ZHANG Hui reviewed the manuscript.
&These authors contributed equally to this work.
#Correspondence should be addressed to ZHANG Hui,E-mail: zhanghui@chinacdc.cn or huizhang1974@126.com
Biographical notes of the first authors:XU Cai Hong,female,born in 1979,MD,majoring in tuberculosis prevention and control;ZHANG Xiao Meng,female,born in 1991,Msc,majoring in tuberculosis prevention and control.
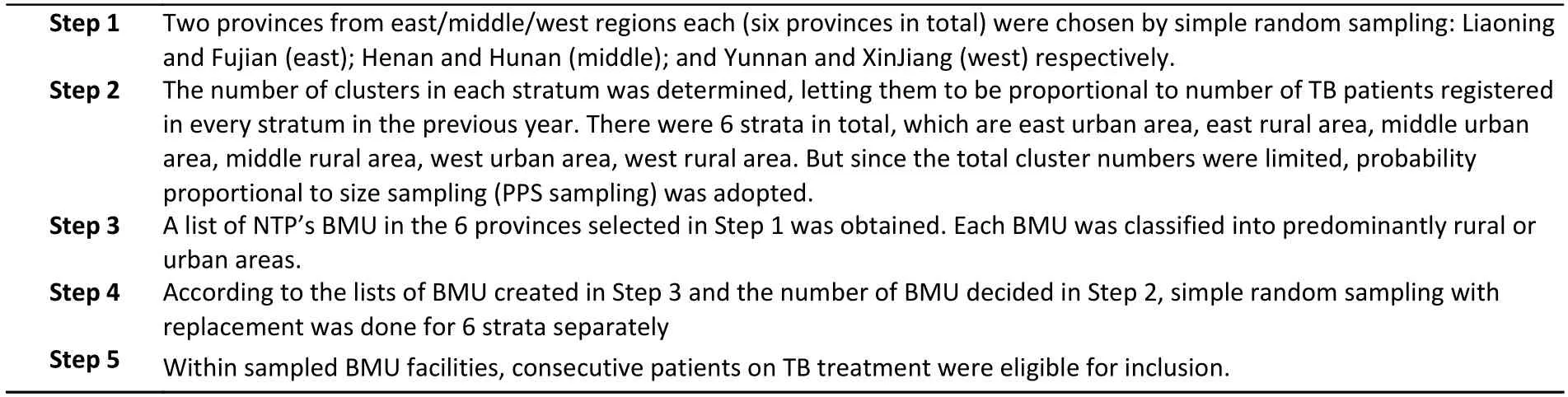
Supplementary File S1. Multi-stage stratified cluster sampling adopted in China’s TB* patient diagnosis survey (2017)
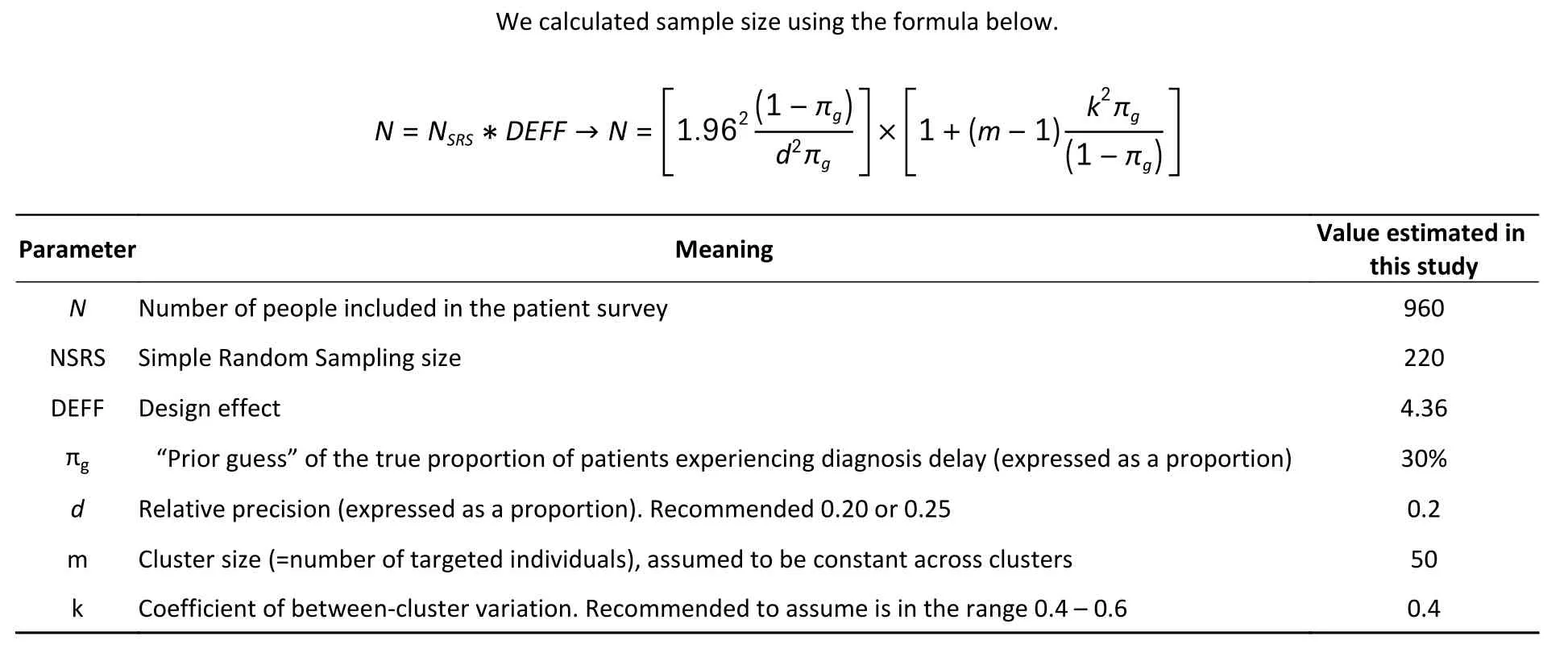
Supplementary File S2.The parameters used for sample size calculation under the nationally representative TB survey, China (Jan–June 2017)
Received:June 9,2021;
Accepted:August 24,2021
 Biomedical and Environmental Sciences2022年1期
Biomedical and Environmental Sciences2022年1期
- Biomedical and Environmental Sciences的其它文章
- Physical Activity Guidelines for Chinese (2021)
- Association of Residential Greenness with the Prevalence of Metabolic Syndrome in a Rural Chinese Population:the Henan Rural Cohort Study*
- SlRT1 Mediates Sestrin1-lnduced lmprovement in Hepatic lnsulin Resistance*
- An Analysis on Failure Reasons of Quit Smoking among Smokers in Beijing Communities
——Based on a Cross-Sectional Study* - Application of Oral Fluid in Measles lgG Antibody Detection for Medical Staff *
- Master Quorum Sensing Regulator HapR Acts as A Repressor of the Mannitol Phosphotransferase System Operon in Vibrio cholerae*
