The development of an evidence-informed Convergent Care Theory:Working together to achieve optimal health outcomes
Holly Wei
University of Louisville School of Nursing, Louisville, KY, USA
Keywords:Caring culture Collaborative care Convergent care Health personnel Organizational culture Precision care Self-care
ABSTRACT Background: Healthcare is a complex and divergent system with uncertainty,unpredictability,and multilayered stakeholders.The relationships among the stakeholders are multifaceted and dynamic,requiring continual interpersonal connections, networks, and co-evolution.It is pivotal to have an evidenceinformed theory to explain the phenomenon, uniting the multifaceted stakeholders’ efforts.Purpose: To describe the development of an evidence-informed theory, the Convergent Care Theory,assembling healthcare stakeholders to work together and achieve optimal health outcomes.Methods: The Convergent Care Theory was developed using a theory synthesis approach based on empirical research and literature reviews published by the theory-proposing author.The empirical evidence was categorized into: patients and families, healthcare providers, healthcare organizations, and patients’ and healthcare providers’ self-care.Results: The Convergent Care Theory includes four concepts: all-inclusive organizational care, healthcare professional collaborative care, person-centered precision care, and patients’ and healthcare providers’ selfcare.Achieving convergent care is a process requiring all stakeholders to work together.Six major facilitators emerged from the research evidence: competence, compassion, accountability, trusting,sharing, and engaging.Conclusion: This article introduced the development process of the evidence-informed Convergent Care Theory.Healthcare systems are complex, with multiple stakeholders’ needs to meet.The Convergent Care Theory strives to unite healthcare stakeholders, bond resources, and join forces to achieve optimal healthcare outcomes.The underpinning of the theory is a caring culture,which is an underlying code for organizational and team behaviors and the foundation of optimal health outcomes.
What is known?
· Healthcare is a complex and divergent system with unpredictability, uncertainty, and diversity and has multilayered stakeholders with divided roles and interests.
· The relationships among the stakeholders are multifaceted and dynamic, requiring continual interpersonal connections, networks, and co-evolution.
What is new?
· The Convergent Care Theory addresses four concepts:all-inclusive organizational care, interprofessional collaborative care,person-centered precision care, and self-care.
· Achieving convergent care is a process requiring all stakeholders to work together.Six major facilitators for the process emerged from the research evidence,including competence,compassion,accountability, trusting, sharing, and engaging.
· This theory signifies the importance of care convergence,emphasizing that human connections and a culture of caring are essential underpinnings of convergent care.
1.Introduction
Healthcare is a complex and divergent system with multilayered stakeholders and unpredictable situations.The relationships among the stakeholders are multifaceted and dynamic,requiring constant interpersonal connections, networks, and coevolution [1,2].Patients’ uncertain and unpredictable conditions add to the complications and complexity of the system.Healthcare is also humanistic, requiring professional collaboration and human being connections to meet multi-layered stakeholders’divergent needs [3-5].The healthcare complexity requires convergent care - all healthcare stakeholders - organization,providers, patients, and families - to work together to achieve optimal health outcomes.
The epistemological underpinning of the Convergent Care Theory is the belief that knowledge can be obtained through all ways of knowing.Carper suggested four patterns of knowing to guide practice and education: empirics, ethics, esthetics, and personal[6].The theory is also based on the belief that caring is a core value of nursing and healthcare[4,7,8],caring culture is the essence of interprofessional collaboration [9], and caring for patients requires professional competence, altruism, responsibility, and empathy[10].The assumption is that a caring culture can promote organizations’ healthy work environments, facilitate interprofessional collaboration, integrate patient care delivery, and improve healthcare outcomes [11-13].
Achieving optimal health outcomes requires the unity of the stakeholders, including healthcare organizations, providers, and patients.The complexity in healthcare and the demand for unified care among the key stakeholders require a theory that considers healthcare diversity and complexity and converges the stakeholders’ efforts to promote healthcare outcomes.This article describes the development of an evidence-informed theory, the Convergent Care Theory, guiding healthcare stakeholders to work together to achieve optimal health outcomes.
2.The nursing metaparadigm underlying the Convergent Care Theory
Nursing is a major healthcare workforce and plays an irreplicable role in leading change, maintaining healthcare function, and improving patient care.Healthcare is a people-centered system that aims to prevent, treat, maintain, and improve the public’s health.During the care process,caring interactions among various healthcare disciplines and professionals are essential in providing cohesive and high-quality patient care [4,5,14,15].The metaparadigm underlying convergent care is described based on the four major concepts noted by Fawcett - person, environment, health,and nursing [16].
2.1.Person
A person is a recipient or provider of care, who can be a patient, a family member, or a healthcare provider.These people can be categorized into caregivers and care receivers who are key stakeholders and play various roles in healthcare.The Convergent Care Theory sees a person from a humanistic and holistic view,meaning that each person is an individual who has specific biopsychosocial needs, can influence others, and can also be influenced by others and the surrounding environments [7,14,17].These beliefs of a person can facilitate the caring relationships among one another, treating patients and peers with humanity,interacting with respect and dignity, and making each other feel safe and belong.
2.2.Environment
Environments refer to the external and internal surroundings impacting a person’s or an organization’s health and function.The Convergent Care Theory signifies that the environment can be internal and external and can affect individuals and organizations.The influence of the environment can be perceived as positive or negative.The internal environment can be one’s physical and mental health, which plays a significant role in individuals’ biopsychosocial health [10,18,19].The external environment can be physical surroundings, cultural atmospheres, or policies.The external and internal environments are intertwined and impact a person’s or an organization’s health and functioning capability[3,18].While external environments affect an individual’s or organization’s health and function, one’s internal conditions, such as ones’ health, values, goals, and beliefs, can influence the interactions with the surrounding environment and actions toward others.Healthcare organizations - settings where patient and community care are offered - are a vital environment for promoting or impeding patients’ and healthcare providers’ health[20,21].Establishing and maintaining positive or facilitating environments are vital for individuals’ and organizations’ growth and performance.
2.3.Health
Health refers to the state in which individuals achieve their best biopsychosocial wellness at the time and context.The Convergent Care Theory addresses health and health outcomes from four aspects of care - an all-inclusive organizational caring atmosphere(organizational care), healthcare professional collaborations(collaborative care), patients’ person-centered care delivery (precision care), and patients' and healthcare professionals' self-care(self-care).Healthcare systems are complex with uncertainty,unpredictability, and variability.It would not be possible for one person or discipline to complete the care patients require, especially when healthcare strives to provide individualized precision health.Besides patients’ health, clinicians’ health is also a significant focus in healthcare.
The Convergent Care Theory recognizes the importance of both patients’ and healthcare providers’ health outcomes.Healthcare professionals across specialties face great health-related challenges and experience psychological issues [22,23].While the external environments, including organizational environments, play a significant role in patients' and healthcare professionals’ health outcomes, self-care emerges to be essential.External environmental factors can only work through internal factors.Thus,it is crucial for healthcare providers and patients to perform self-care.
2.4.Nursing
Nursing signifies a discipline providing care with knowledge gained through all ways of knowing.The Convergent Care Theory combines knowledge gained through empirical, ethical, esthetical,and personal experiences [6].Nightingale, the founder of professional nursing, had a vision for nursing, caring for others with knowledge and passional and a whole person with biopsychosocial needs.Since the Florence Nightingale era, nurses have been responsible for creating an environment suitable for patient healing and have an ethical role in helping patients heal in their best possible conditions[24].Nurses play a significant role in creating a healthy and healing environment for patients, families, and colleagues[20,25,26].Nurses’caring actions determine organizational care, culture, and patient care quality [27-29].While nursing is a significant healthcare workforce, the Convergent Care Theory recognizes the limitation of one discipline and advocates teamwork and interprofessional collaborations.
3.Methods
The Convergent Care Theory was developed using a theory synthesis approach, synthesizing a phenomenon using available evidence.Walker and Avant[30]introduced three basic approaches to theory building: derivation, synthesis, and analysis.This theory was synthesized through integrating the evidence, including empirical research and literature reviews,published by the theoryproposing author from 2015 to 2021[3,9,10,13,18-22,25-29,31-52].A summary of the theoryproposing author’s studies is listed in Table 1.

Table 1Summary of the theory-proposing author’s publications supporting the Convergent Care Theory synthesis.
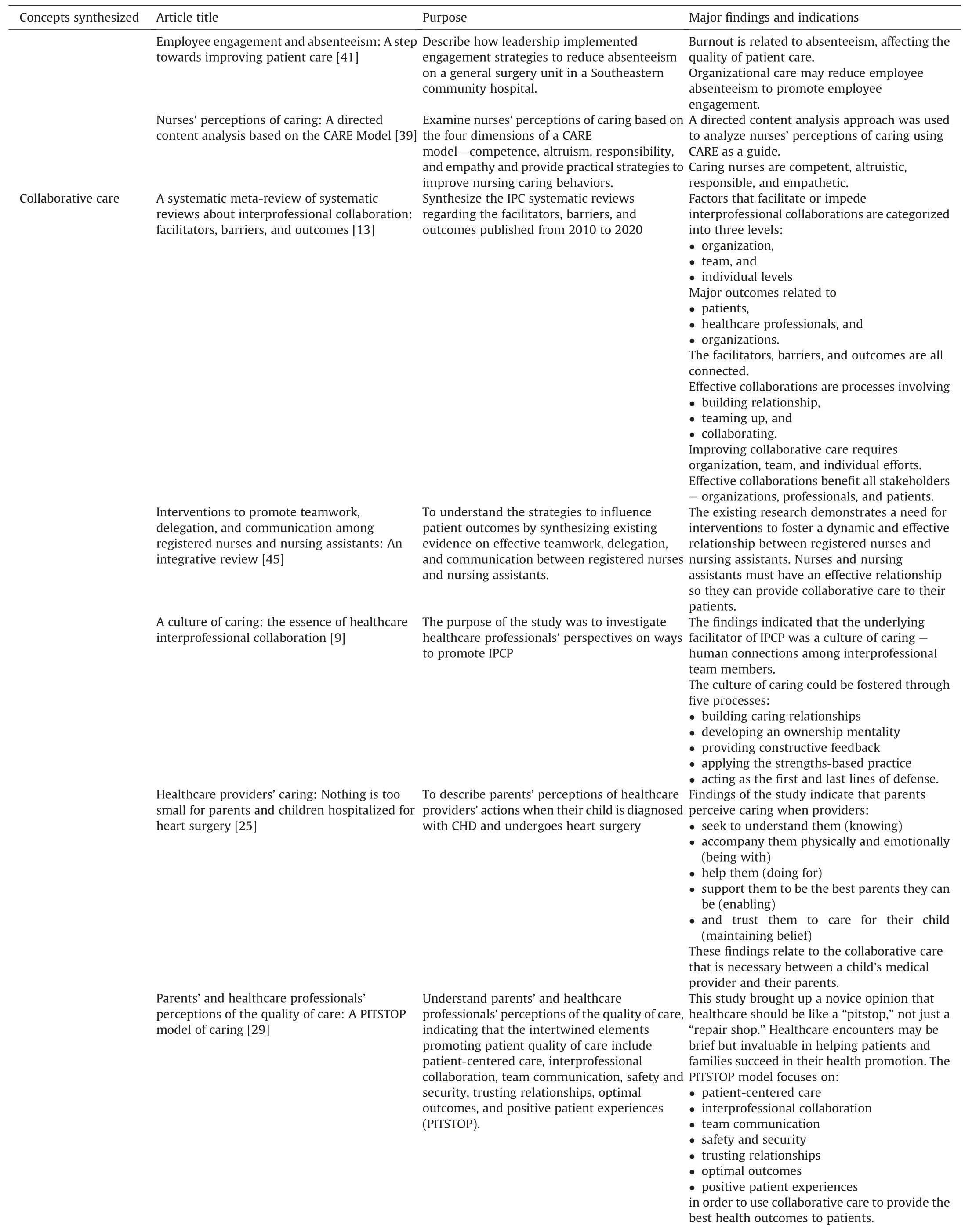
Table 1 (continued)

Table 1 (continued)

Table 1 (continued)

Table 1 (continued)
4.Theory development process
4.1.Empirical evidence underlying the theory development
This section described the empirical evidence underlying the theory development.The theory-proposing author has led multiple research teams and interdisciplinary team members to conduct research and literature reviews to explore the convergent care phenomenon.The studies involved healthcare stakeholders - patients, families, and healthcare professionals from various disciplines,including nurses,physicians,allied health professionals,and healthcare administrators.The empirical evidence was categorized into patients and families,healthcare professionals,and healthcare organizations.The theory-development process is displayed in Fig.1.The Convergent Care theoretical model is shown in Fig.2.

Fig.1. Convergent Care Theory development process.

Fig.2. The Convergent Care theoretical model.
4.1.1.Studies on patients and families
Studies on patients and families provide knowledge about parents’ and family members’ hospital experiences[10,25,27,28,31-36].The research quest for the theory started with families of children hospitalized with acute conditions, such as critical congenital heart disease, undergoing heart surgery[10,35,37].Studies of parents provided knowledge about parents’hospital experiences, expectations for care, perspectives on care quality, and perceptions of healthcare providers’ caring characteristics[10,25].Parents specified that they experienced high levels of stress in healthcare, and what helped them the most during the hospitalization was healthcare providers’ caring characteristics,including professional knowledge, empathy, compassion, teamwork, and daily caring actions.
The studies on patients and families and the literature reviews on patients’perceptions of quality of care led to the exploration of healthcare professionals.When analyzing over a thousand patients'complaints in a major healthcare system, our team found that patients complained the most about healthcare professionals'lack of caring attitudes, team collaboration, and communication [27,28].From patients’ perspectives, healthcare providers’ caring characteristics were professional competence, altruism, responsibility,and empathy[3,10,26].Patient-provider relationships are essential to cultivating patients’ trust and can be developed through nonhierarchical human connections and relationships.
4.1.2.Studies on healthcare professionals
The studies on healthcare professionals offer valuable information about healthcare professionals’ perspectives on building caring relations with patients and promoting organizational culture and performance [19,38-44].The participants in the studies were nurses, physicians, allied health professionals, administrators, and other healthcare supportive personnel [3,19,22,39,41].These studies identified the underlying mechanism of the Convergent Care Theory,which is a culture of caring.Healthcare professionals’daily actions at work directly affect care quality and patients’ and families’ experiences, indicating the significance of human relations between and among co-workers and patients.
These studies explored the “what” and “why” of healthcare professionals’ optimal performance.The findings indicate that nothing that healthcare professionals do is too small in patients’care [10,25], and healthcare professionals’ daily actions at work affect team members’ engagement and patients’ care quality[20,21,26,29].The findings brought up topics like developing an ownership mentality (sharing missions, visions, goals, leadership,and responsibility between organizations and team members),creating a collaborative care environment, and building a patient safety culture, such as “Just Culture” - a culture of shared accountability between employees and organizations, in which organizations take accountability for system changes and employee behavior improvements [9,21].The studies on healthcare professionals suggested the importance of interprofessional collaboration.An optimal outcome of collaborative care is that healthcare professionals work together with patients and families, share decision-making, and provide safe and high-quality patient care.
4.1.3.Studies on organizations
Studies on organizations indicate that health outcomes are directly associated with organizations’ support, commitment, and culture [9,18,20,21,26,38,41,45].An underlying principle of organizations’ performance outcome is a culture of caring that affects human relationships and work environments [3,18,20,21].These studies focused on promoting healthcare professionals’ performance, well-being, and high-quality patient care.Organizations’caring culture, patients’ care, and healthcare professionals’ daily care actions are significantly correlated.Research evidence indicated significant impacts of nurses’ work environments on nurses’interpersonal relationships, psychological well-being, and job performance [18,45].Organizational leadership is significantly correlated with nurses’ engagement and well-being [19,38,40,43]and organizations’ culture [9,13,20,26,29,43].These research studies confirm that patients’ care quality, healthcare professionals’collaborative care, and organizational caring culture are all connected.
4.1.4.Studies on patients’and healthcare providers’self care
Studies on healthcare providers’ self-care yielded noteworthy knowledge about healthcare professionals’ self-care and resilience and patients’ self-care [19,22,40,42,43,46-48].A significant phenomenon surfaced, which is self-care, including self-care for patients and healthcare professionals.These studies suggest that although organizations and work environments are essential for quality care and patients’experiences in healthcare,self-care is the foundation for individuals’ health [36,49-52].
The concept of self-care has two facets,healthcare professionals and patients.Optimal self-care of patients and healthcare providers is essential for improving health system performance.The findings of these studies show that healthcare professionals’ well-being is fundamental to ensure patient care quality and reduce healthcare costs [38,40,41,49-51].The self-care studies led to some practical strategies to promote healthcare professionals’ resiliency building[19,22,43,44,47,48].These findings are consistent with the healthcare Quadruple Aim model in which the fourth aim (promoting clinicians’ health) was added to promote the previously designed Triple Aim (improving patient experience and population health and reducing healthcare costs)[53].Thus,patients'and healthcare providers’self-care is an important concept in the Convergent Care Theory.
4.2.Empirical evidence-informed practice models leading to the theory development
Based on the empirical evidence stated above, five practice models have been developed: the Interprofessional Caring Model[9],CARE Model[10],PITSTOP Model[29],Self-Care ENERGY Model[47],and Resiliency-Building Model[48].These models provided the theoretical foundations for the Convergent Care Theory synthesis.
4.2.1.The Interprofessional Caring Model [9]
The theory-proposing author led a research study exploring healthcare professionals’perceptions of interprofessional collaboration and developed the Interprofessional Caring Model [9].A qualitative study was conducted to interview 36 healthcare professionals in a United States university-affiliated hospital in 2017-2018.The healthcare professionals included hospital administrators, nurses,physicians,nurse practitioners,physician assistants,nurse assistants,and support personnel,such as chaplains and therapists.The model illustrated the professionals’perceptions of healthcare professionals’teamwork and collaboration.The Interprofessional Caring Model identified five processes promoting interprofessional care: Building caring relationships; Fostering an ownership mentality; Providing constructive feedback; Applying strengths-based practice; Taking accountability as the first and last lines of defense [9, p.324].This model proposed the underlying mechanism of the Convergent Care Theory,which is a culture of caring.
4.2.2.The CARE model [10]
The CARE Model recognizes four significant caring characteristics of healthcare providers:Competence,Altruism, Responsibility,and Empathy (CARE).The model was established based on the research findings of patients’ perceptions of healthcare providers’caring behaviors [10].This model was affirmed and expanded by nurses’ perceptions of caring actions through a cross-sectional descriptive study surveying 157 nurses of a university-affiliated hospital across specialties [39].The CARE Model indicated the qualities required for healthcare professionals to create a competent and caring atmosphere in healthcare organizations,laying the foundation for organizational care.
4.2.3.The PITSTOP model [29]
The PITSTOP Model illustrated the importance of personcentered precision care, including patient-centered interprofessional collaboration,team communication,safety,security,trusting relationships, optimal outcomes, and positive patient experiences(PITSTOP)[29].The model was synthesized based on the studies on healthcare professionals and parents of children with critical illnesses.The studies were United States-based, including 27 healthcare professionals and 13 parents of children with critical conditions,which focused on parents’and healthcare professionals’perceptions of quality of care.This model provided evidence underlying patients’ individualized high-quality precision care.
4.2.4.Self Care and Resiliency Building Models [47,48]
Self-care has been recognized as a vital essence for patients and healthcare professionals.The Quadruple Aim is a healthcare practice model, which emphasizes four important aspects of healthcare: promoting patient experience, advancing population health,decreasing costs, and enhancing healthcare professionals’ health[53].The Self-Care ENERGY Model[47]and the Resiliency Building Model [48]delineated ways to promote clinicians’ self-care and well-being, supporting the Quadruple Aim and improving the work-life and well-being of healthcare professionals[53].The Self-Care ENERGY Model acknowledges six strategies to refuel energy:Energy source, Nurturing kindness,Emotional hygiene, Refocusing purpose, Germinating positivity, and Your uniqueness (ENERGY)[47,p.28].The Resiliency-building Model outlines six strategies to foster resilience: Embracing loving-kindness for self and others;Nurturing interpersonal and intersubjective connections and relations; Deepening a creative use of self and sense of belonging;Balancing self-learning, self-awareness, and an evolved selfconsciousness; Valuing forgiveness and releasing negativity;Inspiring and maintaining faith-hope [48, p.130].The goal of promoting self-care is to optimize healthcare performance and outcomes for all stakeholders.
5.Results
5.1.The concepts of the Convergent Care Theory
The results section explained the Convergent Care Theory concepts synthesized.Based on the empirical evidence and practice models, four Convergent Care Theory concepts were synthesized:organizational care,collaborative care,precision care,and self-care.
5.1.1.Organizational care
In the Convergent Care Theory, organizational care refers to an organization’s mission, goals, culture, and commitment to value employees’ contributions, care for employees’ well-being, and ensure resources for employees’work and safety.The wellness of a healthcare organization includes characteristics of kindness,integrity, righteousness, blameless, all-inclusiveness atmosphere(diversity, equality, and inclusion), commitment to care (staff, patients, community, and society), a clearly defined purpose, and a culture of caring [9,13,20,21].The all-inclusive organizational care can support team members with different backgrounds, foster team members’engagement,and make them feel valued,included,and belong,which promotes patients’care atmosphere and quality.As Ray noted in her Bureaucratic Caring Theory, “caring is the convergent focus of professional nursing …, and is bureaucratic given the extent to which its meaning can be understood in relation to the rational-political,legal,social structure of a hospital and the extent to which the concept of bureaucratization is a part of the structure of complex organizations and social structures.”[5,p.163]The Convergent Care Theory emphasizes the importance of organizational resources, support, and culture to healthcare outcomes.
Optimal organizational care is the foundation of the internal code of an organization,determining organizational behaviors and affecting the organization’s internal function and external reputation and business [9,19,20,29].A positive organizational environment, culture, and support system empower team members,promote commitment and belonging, and reduce turnover[9,18,19,27,29,38-40,43,45].Work environments, culture, and power-sharing leadership play a significant role in team members’job experiences and well-being, which affect clinicians’ job performance, organizational resilience, and patient care quality[3,18,40,43].Team members with strong organizational commitment tend to stay longer,perform to their best potential,and foster high-quality patient care [18,20,21,38].
Healthcare administrators must build an all-inclusive organizational culture to embrace diversity, inclusion, and equity.Organizational culture determines the effectiveness and success of organizational strategies and lays the foundation for strategies to take effect[9,18,20,21,26].Healthcare is a complex adaptive system with multi-level stakeholders and professionals working together.The outcome of an all-inclusive atmosphere can help nurses and team members create caring-healing culture, communicate effectively without hierarchical privilege,value one another’s input,and share organization and team goals and missions,which leads to the second concept of the theory, which is Collaborative Care.
5.1.2.Collaborative care
From the Convergent Care Theory perspective,collaborative care is the unity of workforces,including intra-and inter-professionals,to work together and achieve the optimal outcomes at the patients’,nurses’, and health systems' levels.During the collaborative care process, healthcare professionals engage in complementary roles,work cooperatively, and share responsibility and resources to care for patients with the best team efforts [3,9,13].Interprofessional collaborative practice refers to healthcare professionals with various professional backgrounds from different disciplines working together along with patients,family members, and communities to provide the best optimal care [3].Interprofessional collaboration encompasses healthcare professionals’ values, ethics, roles, responsibilities,communication,and teamwork[54].
Healthcare is like a team sport requiring every team member’s effort to achieve a common goal.As indicated in the Synergy Model by the American Association of Critical-Care Nurses, it is vital to synergize nurses’ knowledge, teamwork, and collaboration to promote health outcomes at various levels, including patients,nurses,and systems’outcomes[55].An optimal desire is to have a stable team and practice with established players.A typical process of effective professional collaboration may experience three stages:theestablishing, functioning,andsynergizing stages.
The establishing stageis how healthcare professionals get to know one another and develop a team goal.This stage is like a running-in period, during which teams may experience uncertainty, hesitancy, and conflicts.Team members need to establish relationships and build trust, including knowing one another,building trust, working through conflicts, and sharing goals [9,13].Team members attempt to find effective ways to communicate,build interpersonal relationships, and balance power.
The functioning stageis when team members reach a consensus on goals and cooperate more cohesively.In this stage,interpersonal relationships grow, and team members become committed to one another.Members value individuals’ contributions, share responsibilities and pride, and work together to achieve team goals[3,9,13,25].
The synergizing stageis when team members use their expertise to contribute and produce more comprehensive outcomes than the sum of members’ individual effects.During this stage, team members are motivated to promote team goals and achievements.Individual members develop a sense of belonging [3,9,13,20,29],and team energy is synergized.
In healthcare,however,the teams may often comprise different team members in various situations, especially during emergency situations.Thus, teams may go through these stages at different speeds and forms.Some teams may be more stable than others with long-term team members, and other teams may need to quickly gather with less-familiar members during emergencies.Healthcare professionals must adjust, adapt, and work as a team effectively to provide the best optimal patient-centered care.
5.1.3.Precision care
In this theory, patient-centered precision care is defined as individualized, person-centered, and situation-specific care tailored to meet each patient’s care needs.The principle of precision care stems from precision health or medicine, defined as an approach for disease treatment and prevention that considers individuals’ variability in their specific genes, environment, and lifestyle to achieve optimal health outcomes individually [56,57].Patients’care needs are different and,thus,should be tailored based on individuals’situations.Healthcare professionals should care for patients depending on their specific physical (involving genetics/genomics), environmental (comprising epigenetics/epigenomics),mental, emotional, cultural, and spiritual needs [3,27,28,37,50,51].
Implementing this domain requires and allows healthcare professionals to design personalized,precision programs to predict and provide precise patient care.Healthcare professionals are at the front line and are largely responsible for patients’ health.Thus,caring for patients based on individualized, person-centered, and situation-specific care can help specify patients’care strategies and help them live their lives to the highest potential.
5.1.4.Self-care
In the Convergent Care Theory,self-care is the process in which individuals take care of themselves by actively engaging in healthy behaviors and activities to promote health, prevent illnesses, and manage illnesses when they occur.This concept comprises health promotion, disease prevention, self-administration of medication,care for dependents,rehabilitation,palliative care,and getting care from health providers as needed [58].From the Convergent Care Theory perspective, self-care has two facets - patients and healthcare providers.
There is growing awareness for patients with chronic conditions to participate actively and be involved in their own self-care.The growing healthcare costs are considered a major driver for promoting patients’illness and disease self-care and management.As chronic disease escalates, there is a surging demand for people to have self-care knowledge and take more responsibility for their own care [59,60].Self-care means maintaining one’s health using health-promoting practices and managing disease symptoms upon occurring [61,62].Individuals with chronic illnesses only spend a small fraction of their time in healthcare, and most of the health maintenance, disease management, and illness prevention are taken care of by the individuals and caretakers as self-care undertakings [61,62].The principles of the self-care concept are efficient self-management,improved decision-making, and cooperation between patients, families, and healthcare professionals.
Caring for others is a core value for healthcare professionals, a natural drawing for many to the healthcare profession.However,even though the work is rewarding,healthcare professionals often face stressful work situations, traumatic events, high-intensity workloads, unpredictable work shifts, and long work hours,which places healthcare professionals at high risks for psychological issues, such as stress, depression, anxiety, and burnout.Thus,despite the intention of organizations'support,organizational care alone may not be sufficient to maintain employees’well-being,and self-care becomes critical for healthcare providers’ health[22,53,63].
Practical self-care strategies are critical for healthcare providers.Some effective strategies used by healthcare providers include finding meaning in work, connecting with an energy source,nurturing interpersonal connections, developing an attitude of positivity, performing emotional hygiene, and recognizing one's uniqueness and contribution at work [22, p.44].Other self-care strategies are described in the ENERGY Model - Energy source,Nurturing kindness, Emotional hygiene, Refocusing purpose,Germinating positivity, and Your uniqueness [47, p.28].The resiliency-building strategies comprise facilitating social connections, promoting positivity, capitalizing on nurses’ strengths,nurturing nurses’ growth, encouraging nurses’ self-care, fostering mindfulness practice, and conveying altruism [19, p.681].Other resiliency building strategies are illustrated in the Resiliencybuilding Model: Embracing loving-kindness for self and others;Nurturing interpersonal and intersubjective connections/relations;Deepening a creative use of self and sense of belonging;Balancing self-learning, self-awareness, and an evolved self-consciousness;Valuing forgiveness and releasing negativity; Inspiring and maintaining faith-hope [48, p.130].
5.2.The facilitators of the convergent care
Achieving convergent care is a process, which needs all stakeholders to work together.It calls for facilitators to promote the process.Six major facilitators emerged from the research evidence,including competence, compassion, accountability, trusting,sharing, and engaging.
5.2.1.Competence
Competence is a set of knowledge and skills enabling the adequate performance of a job and working efficiently as required by the job or task.In clinical practice, healthcare competence comprises intertwined components, such as professional knowledge, skills, behavior, and judgment [10,25].Professional competence lies at the heart of a profession’s ability and a cornerstone against which professionals are measured for success [3,10].Patients trust their lives with healthcare professionals.It is essential for healthcare professionals to update and maintain their competence to ensure optimal outcomes for patients and society.
Maintaining competence is a collective obligation and effort of both healthcare professionals and organizations.It is critical for healthcare organizations to engage nurses in fulfilling competence assessment and maintaining the most up-to-date nursing knowledge and skills.One way to motivate healthcare professionals’competence is through value sharing, aligning personal and organizational goals and missions.Organizational values are the moral and operational guidance for individuals and teams’ development and culture, inspiring team members to update their professional knowledge and work together to fulfill professional and organizational goals[3,9,10,20,29].Healthcare professionals’competence is essential for healthcare stakeholders, including patients, peers,organizations, and society.In addition to having the intertwined components, such as knowledge, skills, and judgment, healthcare professionals also require compassion in practice.
5.2.2.Compassion
Compassion is the moral, ethical, and humanistic aspect of nursing care and the philosophical foundation of the nursing profession.Research suggests a direct relationship among patients’perceptions of organizations’support,commitment,caring culture,care quality, and nurses’ caring compassion [9,20,21,26,27,29].Without caring and compassion,professional knowledge and skills may not be delivered effectively [26,28].Caring and compassion can add a human touch to interpersonal interactions and give meaning and purpose to daily actions.
Organizational leaders play a significant role in promoting healthcare professionals’caring and compassionate actions toward themselves and others [3,26].It is essential for healthcare organizations and leaders to help healthcare professionals to maintain competence, knowledge, skills, and caring behaviors.A caring and compassionate attitude can be fostered through cultivating positive leadership and building caring relationships at work [3,20,26,28].Some ways to promote compassion include performing lovekindness to others and self, cultivating healthy work environments,respecting one another and human dignity,and developing caring relationships and collaborations [3,20,25,26,29].Compassionate care can be promoted through supporting interpersonal connections,building positivity on the units,nurturing professional growth, and encouraging healthcare professionals’ self-care and well-being[3,19,48].To ensure patients’quality of care,healthcare professionals’ accountability is essential.
5.2.3.Accountability
Accountability is taking responsibility for one’s professional judgments and actions and upholding one’s professional knowledge,competency,professional standards,and patient care quality.Professional accountability underpins the safe professional practice, addressing the need for knowledge, skills, and attitudes required for professional accountability and reinforcing congruence and consistency between professional actions and standards to ensure quality and safe patient care [64-68].
Healthcare professionals are held accountable for the care they provide to patients.They should fulfill their obligations stated in the professional code of ethics, which clarifies a profession’s roles and responsibilities and guides professionals to address questions related to ethical issues in practice.From patients’and co-workers’perspectives,great healthcare providers are not only competent in and responsible for their professional knowledge and skills but also caring, compassionate, empathetic, and altruistic [3,10].Being accountable is vital because their actions affect the outcomes of many, including patients, families, healthcare professionals themselves, organizations, and society.
5.2.4.Trusting
Trusting is the belief and confidence in a person’s reliability and ability to fulfill the commitment promised.In healthcare, trusting signifies healthcare professionals’caring characteristics,knowledge,and skills in promoting health outcomes and represents confidence,reliance, honesty, and sincerity.Trusting relationships among the healthcare stakeholders facilitate organizational commitment, support,culture,team collaborations,self-care,and high-quality personcentered patient care [9,29].Trust is an effective component in ensuring healthy work environments,teamwork,and organizational performance [10,25].It is vital for patients to trust healthcare professionals and for team members to trust one another.
On healthcare teams,trusting is a key concept and facilitator for creativity and team success.An important antecedent or foundation of collaboration is fostering trust and caring relationships among team members, which are essential in promoting a team’s caring culture and collaboration[64].Trust is the power that can bond a team together and create a sense of belonging[3,10,20,27,29].When trusting one another,team members tend to join forces and achieve goals [3,9,29].Trust can inspire team members and unite individual strengths to achieve optimal outcomes.The sense of belonging and caring working relationships are motivational factors for collaborative care.
5.2.5.Sharing
Sharing is team members’commitment to sharing values,goals,and leadership.Shared values and goals, such as delivering highquality patient care, can help team members unite and foster professionals’ stewardship [9,13].Shared leadership encourages team members’ ownership mentality and commitment to achieving common goals.An ownership mentality refers to having the autonomy and obligation to make decisions for group tasks,take responsibility for outcomes, and offer suggestions for improvement [9,13].The ownership mentality nurtures nurses’shared governance and leadership mindset and fosters nurses’commitment as the first and last line of defense for patients’safety[9,13].The sense of ownership can motivate team members to do their share, be accountable, and work together towards the common goals [3,9,13].
The level of healthcare professionals’ engagement and ownership mentality can motivate team members to not only “see” the problems but also take responsibility and bring solutions as decision-makers.Sharing can be achieved by sharing leadership,building trust,and communicating effectively between and among leaders and team members.Shared leadership is a process and a leadership style to delegate and distribute leadership responsibility to team members within a team and organization.Team members share decision-making, vision, goals, trust, values, and responsibilities [3,9,13,38,41].Because of the willingness to share,team members develop an accountable mindset for the entire team’s success.Trusting relationships and sharing may enable healthcare processionals’ engagement.
5.2.6.Engaging
Engaging is to create and sustain supportive team environments, encourage individual contribution and accountability, and enable team members to foster competence and compassion[3,9,13,19].Engagement is characterized by team members’showing high enthusiasm, motivation, dedication, vigor, and absorption at work [38].An engaging team has a healthy work environment that promotes trust, accountability, and compassion and increases team members’ commitment to participation [41,43].Team members’engagement significantly affects collaborative care accomplishments and patients’ outcomes [38,41,43].
Team members’ engagement can be promoted through empowerment.Empowerment supports team members with authority and power to help them contribute at their highest capability based on their experience and expertise.Empowerment fosters a shared leadership and accountability culture,where team members feel valued and committed to achieving a common goal.The organizations with empowered teams and members have a relatively collaborative hierarchical leadership structure and a high proportion of highly trusted members [9,29,43].
5.3.The theory assumption statements
Four theory statements are formed and expressed in the following assumptions.
· Assumption 1.Optimal healthcare outcomes depend on the convergence of all-inclusive organizational care, healthcare professional collaborative care, person-centered precision care,and patients’ and healthcare providers’ self-care.
· Assumption 2.Organizational care can support collaborative care, precision care, and self-care, which, in turn, enhance organizational health.
· Assumption 3.Collaborative care depends on the alliance and synergism of all stakeholders, including organizations, healthcare professionals, patients, and families.
· Assumption 4.The process of convergent care can be enabled by the following facilitators: competence, compassion, accountability, trusting, sharing, and engaging.
6.Discussion
This article introduced the development process of an evidenceinformed Convergent Care Theory.This theory signifies the importance of care convergence, emphasizing that high-quality patient care and optimal health outcomes require all-inclusive organizational care, interprofessional collaborative care, personcentered precision care, and effective patients’ and healthcare professionals’ self-care.Convergent Care Theory aims to unite healthcare stakeholders,bond resources,and join forces to achieve optimal healthcare outcomes.
The convergent care facilitators include competence, compassion, altruism, engaging, sharing, and belonging.These concepts align with the theoretical philosophy of the theory,the unity of all ways of knowing, including research evidence, experiences, and perceptions.The theory proposes that nursing practice requires professional knowledge and humanistic characteristics.Healthcare professionals’ collaborative care can lead to unity, efficiency, and quality under a caring culture.The caring atmosphere motivates individuals to develop professionally, work together, and perform at the highest professional capability.
6.1.Strengths
Interprofessional collaboration and caring are fundamental elements in the Convergent Care Theory and clinical practice.Compared with theories, such as caring, self-care, and interprofessional collaboration-related theories [5,59,61,62], the Convergent Care Theory covers the organization, collaboration, precision care, and self-care from a more inclusive and holistic perspective.This theory not only shows the phenomenon of caring, collaboration, and the practical process of collaboration and teamwork but also the “why” behind the phenomena.The essence of caring and collaboration is the culture of caring.Team members care for one another to collaborate.The major facilitators for establishing a caring culture and effective collaborations are professional competence, compassion, accountability, trust, sharing, and engagement.This theory leads the way of considering multiple aspects of health services and multi-layered stakeholders to promote the effectiveness of care delivery and achieve the best optional outcomes.The increasing complexity in healthcare creates problems and challenges, yet it also provides opportunities for creativity in relationship building, interdependencies, and innovative care models.The Convergent Care Theory aims to address these issues and challenges.
The Convergent Care Theory was developed based on substantial empirical evidence through clinical research studies and relevant literature (systematic, integrative, and critical reviews) in recent years.The theory was originated from clinical practice with the potential to guide and support clinical practice.In addition,this theory embraces the healthcare systems’ multi-facet characteristics, addresses empowerment and power in teambuilding,and reflects organizational diversity,inclusion,and equity.Another strength of the theory is the convergence of science and art.It describes and explains a phenomenon that effective care requires a combination of science and art - scientific knowledge and caring humanity.
6.2.Limitations
The theory, however, currently lacks a systematic scale to measure the progress of the theory-based practice.Each concept needs to be measured using separate scales.A Convergent Care Scale is needed to measure the effectiveness of professional collaboration, patient care quality, and organizational culture,support, and commitment.Another weakness or limitation is that this theory was developed mainly based on the research evidence from hospital-based care and experiences.It needs to be validated in different healthcare settings, such as community and rehabilitation settings.
6.3.Clinical implications
Hospitals can design their practice models based on the Convergent Care Theory.For example,hospitals can establish their organizations’ mission, values, and goals based on the four concepts, organizational are, collaborative care, precision care, and self-care, with a clear picture of what they want to accomplish.They can develop specific strategies based on the facilitators,including ways to promote professional competence, compassion,accountability, trust, share, and engagement, based on their organizations’ exact situations and needs.
For example,three hospitals developed and implemented their nursing practice models based on the concepts and facilitators.One of the hospitals designed eight factors to promote care delivery,four factors for healthcare professionals and four for patient-related education and care.They developed a visual practice model,made flyers,and established outcome measures for the hospital.Another hospital used a similar process but developed different strategies and outcome measures based on the theory’s concepts and facilitators.The third hospital developed organizational strategies to promote the hospital’s caring culture, support, healthcare professionals’ self-care, well-being, employee engagement, and patients’ experience[21].
These hospitals defined the concepts based on their hospitals’needs and requirements and operationalized the concepts to guide nurses’ practice.For example, for the “Competence” concept, one hospital defined it as nurses’ability to provide care for patients and their families, including organizations’ proficiency of continuing education and nurses’ aptitude for collaboration.Competence comprised nurses’ proficiency in teamwork and collaboration between and among nurses and healthcare professionals of other disciplines.
7.Conclusions
This article introduced the development process of an evidenceinformed theory.The Convergent Care Theory was synthesized from clinical empirical evidence related to the key healthcare stakeholders, including healthcare organizations, professionals,patients, and families.It takes the unity of all-inclusive organizational care, effective interprofessional collaboration, patientcentered precision care, and patients' healthcare professionals’self-care to achieve optimal health outcomes.With the underlying principle of a culture of caring,this theory addresses collaboration,power- and resource-sharing, teamwork and engaging, diversity,inclusion,equity,and self-care in clinical settings.Convergent Care Theory strives to unite healthcare stakeholders, bond resources,and join forces to achieve optimal healthcare outcomes.The underpinning of the theory is a caring culture,which is an underlying code for organizational and team behaviors and the foundation of optimal health outcomes.
Funding or sources of support
This study is supported in part by the University of Louisville School of Nursing and CCI Research Foundation.
Ethical approval
Not Applicable.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
I want to acknowledge many who are involved in the theory development.The theory-development process has been a highly collaborative work.Many collaborators have made great contributions during the initial data collection, practice model development, and application stages.
I also would like to thank Professor and Dean Dr.Sonya R.Hardin,Professor and Associate Dean Dr.Lynne A Hall,and Ms.Lili Sun for their support.
I also want to acknowledge the research scholarship and funding support received during the initial research studies, including but not limited to Leininger Culture Care Scholarship Award from the International Association for Human Caring;Jane Winningham Smith Scholarship from the School of Nursing at the University of North Carolina at Chapel Hill, North Carolina; Dr.Lester Sauvage Research Fund from the Hope Heart Institute,Seattle,Washington;East Carolina University College of Nursing graduate department seed grant; the NINR T32NR007091 grant from the School of Nursing at the University of North Carolina at Chapel Hill; Nursing Research Award from the North Carolina Nurses Association; University of Louisville School of Nursing; CCI Research Foundation.
 International Journal of Nursing Sciences2022年1期
International Journal of Nursing Sciences2022年1期
- International Journal of Nursing Sciences的其它文章
- 新型冠状病毒疫情期间护理本科生职业认同及相关因素的调查研究
- 医疗卫生人员循证实践知识与培训需求的调查研究
- 约旦冠心病患者心理韧性的调查研究
- 国际学术网站集萃
- 一种多功能警报及决策支持系统的设计
- 手术室跨专业团队合作的障碍和促进因素
