Takotsubo syndrome with underlying pheochromocytoma
Tooba Sahar✉, Asaad Akbar Khan, Raja Wajid Shabbir
Cardiology Department, Shifa International Hospital, Islamabad, Pakistan
Takotsubo cardiomyopathy (TTC), also referred as broken heart syndrome, is a type of non-ischemic cardiomyopathy usually preceded by exposure to significant physical or emotional stress.[1]Reported by Sato,et al.[2]in 1990 for the first time, the condition resembles acute coronary syndrome (ACS), characterised by chest pain and dyspnoea.[3]ST-segment elevation and/or T wave inversion and pathological Q waves are present in almost 40% of patients on electrocardiogram.[4]It is recently established that TTC causative factor is not only an acute emotional stress, but also sudden intracranial events, including haemorrhage, trauma and ischemic events; acute medical diseases such as sepsis and surgical interventions; increased secretion of endogenous catecholamines (pheochromocytoma); and administration of exogenous catecholaminergic agents can contribute to the disease pathology. TTC has been recognized by the American College of Cardiology/American Heart Association as a distinctive form of reversible cardiomyopathy.[5]
A 63-year-old man presented to the emergency department with central chest pain radiating to neck and 4−5 episodes of vomiting in the last 15 h. Pain scale was described as 3/10. He also complained of 1 episode of loose stools one day back. Patient was a known case of hypertension. His past medical history was notable for right-sided abdominal pain about two months back for which computed tomography(CT) scan was done. A contrast enhanced CT scan had revealed a large right adrenal mass 10 cm × 9.7 cm × 10 cm (Figure 1), having mass effect on the upper pole of the right kidney. Differentials included adrenal carcinoma, atypical pheochromocytoma or less likely metastasis. Surgery was planned later that month. No history of smoking, hyperlipidaemia,diabetes mellitus and family history. His home medications included doxazosin 1 mg twice a day and tenormin 25 mg once a day.

Figure 1 Contrast enhanced multi-slice computed tomography renal dynamic performed shows a supra-renal mass measuring 10 cm × 9.7 cm × 10 cm.
Initial emergency room examination revealed blood pressure (BP) of 134/70 mmHg, pulse of 98 beats/min and normal S1 S2 heart sounds. His electrocardiogram revealed normal sinus rhythm with ST-segment elevations in leads V2–V3 (Figure 2)and initial laboratory workup revealed elevated troponin I levels of 5,274 pg/mL (normal levels up to 34.3 pg/mL) and creatine kinase-MB levels of 18 ng/mL (normal levels up to 7.2 ng/mL), which suggested acute anterior wall myocardial infarction (MI).Patient was shifted directly to the cardiac catheterization laboratory for emergency primary percutaneous intervention for suspected acute MI. However,the procedure revealed normal coronary arteries(Figure 3A–3C). His echocardiography showed a reduced ejection fraction of 45% with severe apical hypokinesis (Figure 4A & 4B). He was diagnosed to have takotsubo syndrome and was treated with aspirin 75 mg, doxazosin 1 mg, and atorvastatin 10 mg and on and off glyceryl trinitrate infusion for fluctuating high BP. He was discharged on the third day from hospital in a stable condition with the advice to start low dose short acting beta blocker, i.e., metoprolol 12.5 mg once a day and then later switch to atenolol 25 mg once a day with instructions for strict BP monitoring.

Figure 2 ST-segment elevations in leads V2–V3.
Patient remained in stable condition at home. His follow-up echocardiography was performed after two weeks which revealed normal left ventricular systolic function with an ejection fraction of 60%with no wall motion abnormality (Figure 5A & 5B).
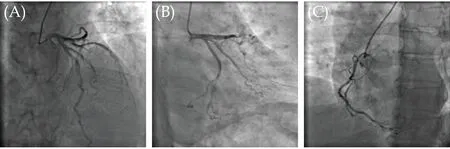
Figure 3 Coronary angiograms (A–C) showing no signs of coronary stenosis with mild luminal irregularities.
His adrenalectomy was performed in the next month. Right adrenal mass was sent for biopsy which confirmed pheochromocytoma of adrenal gland(Figure 6). BP was found to be stable off-medications and all the symptoms were resolved.
Our patient came with an unusual presentation of anterior wall MI with fluctuating BP, which was diagnosed to be a case of pheochromocytoma induced TTC.

Figure 4 Heart in systole, showing left ventricular apical hypokinesis with mid to basal hyperkinesis (apical ballooning) (A), and heart in diastole, showing dilated left ventricular (B).

Figure 5 Heart in diastole, showing preserved apical wall thickness with normal left ventricular dimentions (A), and heart in systole, showing normal endocardial thickening and wall motion in apex (B).

Figure 6 Encapsulated tumor comprising of nests of cells separated by fibrovascular septa.
The patient presented with typical chest pain, uncontrolled angina, increased levels of cardiac enzymes, decreased contraction of apical wall and nonobstructive coronary vessels. The initial diagnosis was TTC. The distinguishing feature of TTC is reversible decreased contraction of apical wall, heart failure, non-obstructive coronary arteries caused by emotional trauma. TTC is more frequent in elderly females.[5]Conversely, TTC in this particular patient had some variances with the usual TTC considering that this patient had no emotional trauma and was male. Not long ago, it has been established that TTC and hypertension can present due to underlying pheochromocytoma.[6]Catecholamines released by pheochromocytoma can lead to grave cardiovascular implications such as high BP, TTC, left ventricular hypertrophy, and heart failure.[7]
The diagnosis of pheochromocytoma is frequently delayed or missed. Cardiomyopathy caused by increased levels of catecholamines has been established with few cases of pheochromocytoma, and a small number of cases of pheochromocytoma present as ACS.[8]
In this particular case, the correct diagnosis was made due to the images available that showed an adrenal mass, presentation of ST-segment elevation MI and emergency angiography which showed normal coronaries. The case had a dubious clinical presentation: ST-segment elevations in anterior leads, raised cardiac enzymes, left ventricular dysfunction,and typical chest pain but normal coronaries. The features were consistent with TTC and ACS.
This patient presented with atypical TTC and ACS with fluctuating BP and was diagnosed with an adrenal mass. It is therefore, essential to think about pheochromocytoma-induced MI at an early stage to reduce the risk of further myocardial damage and prompt removal of the causative factor.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2021年12期
Journal of Geriatric Cardiology2021年12期
- Journal of Geriatric Cardiology的其它文章
- Echocardiography and impedance cardiography as determinants of successful slow levosimendan infusion in advanced older heart failure patients
- Association between serum cystatin C level and hemodynamically significant aortic stenosis: a prospective cohort study
- Lipoprotein(a) is associated with coronary atheroma progression:analysis from a serial coronary computed tomography angiography study
- A different cardiac resynchronization therapy technique might be needed in some patients with nonspecific intraventricular conduction disturbance pattern
- MiR-21-5p-expressing bone marrow mesenchymal stem cells alleviate myocardial ischemia/reperfusion injury by regulating the circRNA_0031672/miR-21-5p/programmed cell death protein 4 pathway
- Reversible heart failure in a patient with hypocalcemic cardiomyopathy
