Clinical study on Tuina plus umbilical therapy for senile functional constipation
Gong Xu-fang (龚旭芳)
Zhejiang Rongjun Hospital, Jiaxing 314000, China
Abstract
Keywords: Tuina; Massage; Point, Shenque (CV 8); Administration on Umbilicus; Acupoint Sticking Therapy; Constipation;Qi Deficiency of Spleen and Lung; Aged
Functional constipation (FC) is a common digestive tract disease in the elderly. The main manifestations include dry stool, difficult defecation, reduced defecation times or prolonged interval, abdominal distension, etc.Long-term constipation may cause feces to stay in the intestine, which may induce malignant lesions in the intestine. The incidence of colorectal cancer is closely related to this condition. In addition, forced defecation in patients with constipation can increase patients’ intraabdominal pressure, and subsequently increase their heart burden and oxygen consumption, inducing or aggravating cardiovascular and cerebrovascular diseases.Long-term constipation can also lead to negative emotions, such as anxiety in patients and seriously impair their quality of life (QOL)[1-3]. Modern medicine holds that improper diet, long-term bed rest, lack of exercise and gastrointestinal dysfunctions are the main factors for senile FC[4]. At present, Western medicine mainly adopts laxatives, motility-promoting drugs,secretion-promoting drugs, enemas and suppositories to treat FC. Although the symptoms can be relieved in the short term, the patients can become highly dependent on drugs and the symptoms often relapse after drug withdrawal. Consequently, the long-term effect of Western medicine is not satisfactory. Traditional Chinese medicine (TCM) has rich experience in treating constipation. In particular, the external treatment of TCM is effective, simple, convenient, and inexpensive. In recent years, we have employed Tuina (Chinese therapeutic massage) plus umbilical therapy to treat senile FC. The details are as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Western medicine
Referred to the diagnostic criteria for constipation described in theGuidelines on Diagnosis and Treatment of Chronic Constipation in China(Wuhan, 2013)[5],excluding constipation caused by organic diseases or drugs, and meeting the diagnostic criteria for FC described in the reference[6].
1.1.2 TCM
Referred to the diagnostic criteria for the syndrome of Qi deficiency of lung and spleen described in theCommon Views on Diagnosis and Treatment of Chronic Constipation with Chinese Medicine[7].
Main symptoms: patients may have trouble in defecation though they have defecation intention and the stools are not hard or dry; sweating and shortness of breath after forced defecation; and prolonged defecation time. Secondary symptoms: mental fatigue,reluctant speech, abdominal distention, shortness of breath, lassitude, poor appetite, puffy and lusterless face,pale complexion, a pale tongue with thin white coating,and weak pulse beats.
One could be diagnosed with FC if he presented all the main symptoms and two or more secondary symptoms.
1.2 Inclusion criteria
Met the above diagnostic criteria; aged between 60 and 80 years old, male or female; with normal results of routine examinations for liver and kidney functions,blood, urine, and feces; did not respond well to the change of diet or increase of exercises; stopped taking relevant drugs or did not take drugs for at least three months; voluntarily participated in the trial and signed informed consent.
1.3 Exclusion criteria
Those who suffered from organic diseases involving the intestinal tract including colorectal tumor, rectal prolapse, intestinal obstruction or stenosis; suffered from hemorrhagic diseases, high fever, suppurative inflammation or tuberculosis; suffered from liver and kidney dysfunctions or severe cardiovascular and cerebrovascular diseases; had a history of gastrointestinal operation; were unable to receive Tuina treatment due to skin injury or serious skin diseases;those who suffered from serious mental diseases,unconsciousness, communication disorders or cognitive impairment; were participating in other clinical trials.
1.4 Dropout criteria
Dropped out naturally or could not be followed up; did not provide complete clinical data; had to drop out due to accidents.
1.5 Statistical methods
The SPSS version 20.0 statistical software was adopted for data analysis. The measurement data which met normal distribution were expressed as mean ± standard deviation (±s). The independent samplet-test was used for inter-group comparisons, and the pairedt-test was used for intra-group comparisons. Rank-sum test was used for ranked data. Chi-square test was used for the counting data. Two-tailed test was adopted withα=0.05.P<0.05 indicated statistical significance.
1.6 General data
Senile FC inpatients and outpatients in our hospital between June 2017 and June 2019 were recruited in the study. They were randomly divided into an observation group and a control group by the random number table method. There were no significant differences between the two groups in the general data (P>0.05), indicating that the two groups were comparable (Table 1).
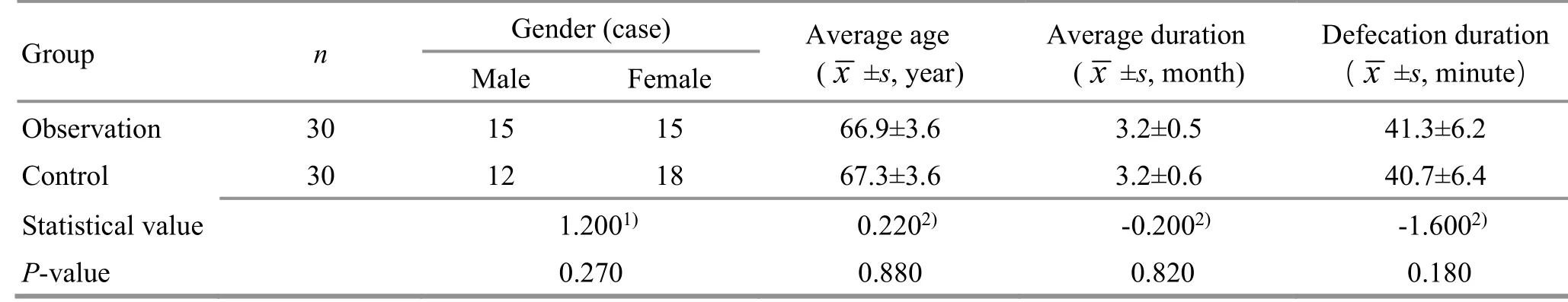
Table 1. Comparison of the general data between the two groups
2 Therapeutic Methods
During treatment, the patients in both groups were educated to develop healthy defecation habits, keep proper exercise and diet, and not eat uncooked, cold,spicy or greasy food, as well as fish and shrimp.
2.1 Observation group
The patients in the observation group received Tuina and umbilical therapy.
2.1.1 Tuina
The patient took a supine position and relaxed the abdomen. The operator stood by the right side of the patient with the right palm putting on the patient's abdomen, and the left palm on the right hand. From the patient's right lower abdomen, the operator An-Pressed and Rou-Kneaded the patient's abdomen clockwise along the anatomical routes of the ascending, transverse,and descending colon. The treatment was operated for 5 min with moderate strength (Figure 1). Then he performed one-thumb Tui-Pushing manipulation at Zhongwan (CV 12), Tianshu (ST 25), Daheng (SP 15),Qihai (CV 6), and Guanyuan (CV 4). Each acupoint was manipulated for 1 min with the strength making the patient feel soreness and heaviness (Figure 2). Finally,the patient took a prone position and exposed the lumbosacral region. The operator used vaseline as the medium to Ca-Rub the lumbosacral part of the patient by the palm until the patient felt gently hot (Figure 3).
2.1.2 Umbilical therapy
We groundDa Huang(Radix et Rhizoma Rhei) 9 g,Huang Lian(Rhizoma Coptidis) 15 g andHuang Qin(Radix Scutellariae) 12 g into powder, mixed it into a paste with sterile distilled water, and then made a herbal cake with a diameter of about 3 cm, a height of about 0.5 cm and a mass of about 15 g. Then the herbal cake was heated and placed on Shenque (CV 8) for 6 h/time(Figure 4).
Tuina and umbilical therapy were given once a day.The efficacy was evaluated after two weeks of treatment.
2.2 Control group
The patients in the control group took lactulose oral solution [specification: 15 mL/piece, State Food and Drug Administration Approval No. H20065730, Beijing Hanmi Pharm. Co., Ltd., China] at breakfast, with the initial dose of 30 mL/time, once a day. After one week of treatment,the dose was adjusted according to their individual conditions, and the reference maintenance dose was 10-25 mL/d. The efficacy was evaluated after two weeks of treatment.

Figure 1. An-Pressing and Rou-Kneading manipulation

Figure 2. One-thumb Tui-Pushing manipulation

Figure 3. Ca-Rubbing manipulation

Figure 4. Umbilical therapy
3 Observation of Clinical Efficacy
3.1 Observed items
3.1.1 Wexner continence grading scale (WCGS)
Before and after treatment, the WCGS was adopted to score eight items related to constipation including fecal property, defecation time, defecation frequency and difficulty in defecation. The total score was between 0 and 30 points. The lower the score, the milder the degree of constipation.
3.1.2 Patient assessment of constipation-quality of life questionnaire (PAC-QOL)[8]
PAC-QOL was adopted to evaluate the quality of life of the patients, including the following four dimensions:worry and anxiety, psycho-society, physical discomfort,and satisfaction. These four dimensions were divided into 28 items. Items 18 and from 25 to 28 were reverse items. All kinds of discomfort were given 1 to 5 points respectively according to the degree from ‘absence’ to‘severe’. The score of each dimension was the sum of the scores of all items in this dimension, and the sum of the scores of all dimensions was the total score. The lower the score, the higher the QOL.
3.2 Efficacy evaluation criteria
Referred to the efficacy evaluation criteria for constipation described in theGuidelines for Diagnosis and Treatment of Common Internal Diseases in Chinese Medicine[9].
Cured: Defecation discomfort and incompleteness disappeared, the fecal property was normal, and the defecation frequency was 5-7 times a week.
Markedly effective: Pain, discomfort and incompleteness were almost absent from defecation,the fecal property was significantly improved, the defecation interval was less than 72 h, and the defecation frequency was between 3 and 5 times a week.
Effective: The fecal property improved, the symptoms were relieved and the defecation interval was shortened by 1 d compared with that before treatment.
Invalid: The improvement of symptoms did not reach the above three standards.
3.3 Results
3.3.1 Comparison of the effective rate
The total effective rate in the observation group was 90.0%, which was higher than that in the control group(76.7%), and the difference between the two groups was statistically significant (P<0.05). Check Table 2 for details.
3.3.2 Comparison of the WCGS score
After treatment, the WCGS scores in both groups decreased compared with those before treatment, and the differences within the groups were statistically significant (P<0.05). The WCGS score in the observation group was lower than that in the control group, and the difference between the two groups was statistically significant (P<0.05). Check Table 3 for details.
3.3.3 Comparison of the PAC-QOL score
After treatment, the PAC-QOL scores in both groups decreased compared with those before treatment, and the differences within the groups were statistically significant (P<0.05). The PAC-QOL score in the observation group was lower than that in the control group, and the difference between the two groups was statistically significant (P<0.05). Check Table 4 for details.
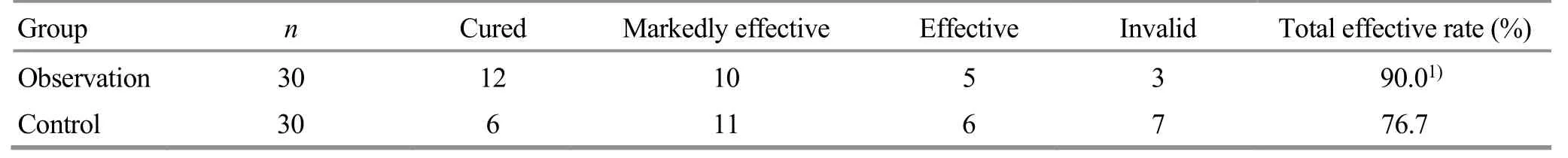
Table 2. Comparison of the efficacy between the two groups (case)
Table 3. Comparison of the WCGS score between the two groups ( ±s point)
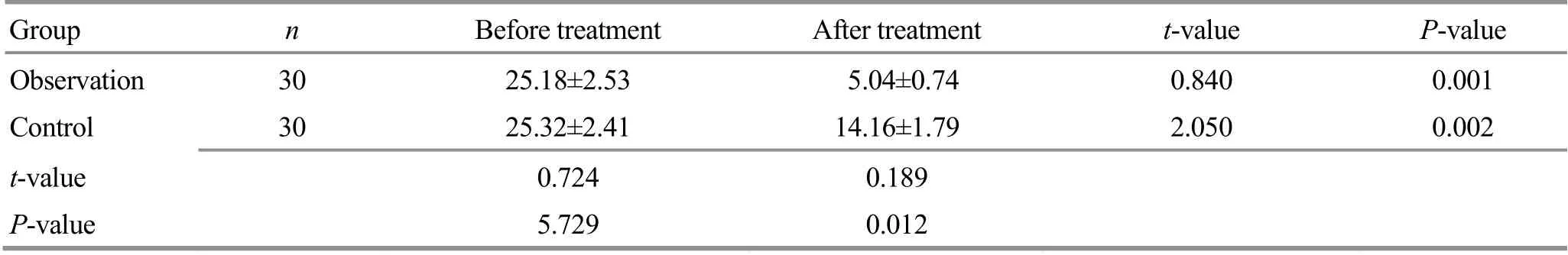
Table 3. Comparison of the WCGS score between the two groups ( ±s point)
Group n Before treatment After treatment t-value P-value Observation 30 25.18±2.53 5.04±0.74 0.840 0.001 Control 30 25.32±2.41 14.16±1.79 2.050 0.002 t-value 0.724 0.189 P-value 5.729 0.012
Table 4. Comparison of the PAC-QOL score between the two groups ( ±s, point)
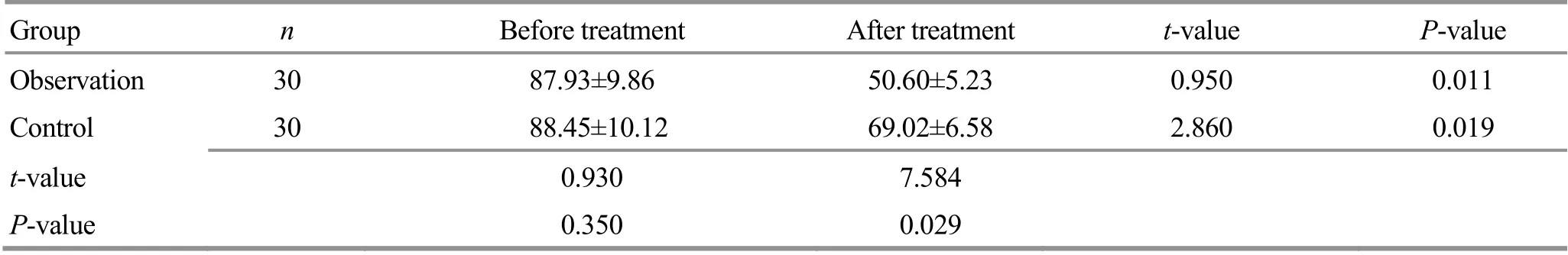
Table 4. Comparison of the PAC-QOL score between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 30 87.93±9.86 50.60±5.23 0.950 0.011 Control 30 88.45±10.12 69.02±6.58 2.860 0.019 t-value 0.930 7.584 P-value 0.350 0.029
4 Discussion
FC is a common digestive tract disorder. With a long duration, it often affects the elderly. It not only influences the intestinal nutrient absorption and living status of the patients, but also relapses easily. It can increase the risk of colon cancer, cardiovascular and cerebrovascular diseases, and even sudden deaths. The current treatment aims at alleviating symptoms and improving intestinal functions.
Lactulose is a synthetic nonabsorbable disaccharide. It is a hyperosmotic laxative, and not easy to be decomposed by digestive enzymes. After entering the colon, it will be transformed into low-molecular-weight organic acids to form an intestinal hypertonic state,absorb water through osmosis, increase intestinal volume, and stimulate intestinal peristalsis, thus restoring intestinal physiological rhythm and promoting the discharge of feces[10-12]. However, long-term use may cause serious dependence, and may damage the intestinal nerve endings and aggravate the condition.
In TCM, constipation falls under “difficulty in bowel movements”, “deficient constipation”, “Qi constipation”,“intestinal obstruction” or “splenic constipation” and locates in the large intestine. The basic is abnormal conduction of the large intestine. Improper diet,overexertion or emotional disturbance in elderly patients may cause Qi deficiency of lung and spleen, and failure in transportation and transformation. This condition may result in weak large intestine conduction,intestinal stagnation, and subsequent constipation[13].
Tuina is a commonly used external treatment. Studies have shown that abdominal Tuina can promote gastrointestinal peristalsis and the secretion of digestive juice, and improve the excitability of sympathetic nerves.Abdominal manipulations can change the abdominal pressure, enhance rectal compound movement, cause relaxation of the internal anal sphincter, and thus promote defecation[14-17]. In this study, one-thumb Tui-Pushing manipulation was performed at Zhongwan(CV 12), Tianshu (ST 25), Daheng (SP 15), Qihai (CV 6) and Guanyuan (CV 4). Tianshu (ST 25) is the Front-Mu point of the large intestine. It can regulate Qi, remove stagnation, ascend the clear and descend the turbidity.Daheng (SP 15) can remove stagnation, dredge the Fu organs, and regulate the stomach and spleen. Qihai(CV 6), governing the Qi movements, can reinforce Yuan-Primordial Qi and dredge the Conception Vessel.Zhongwan (CV 12) is the Influential Point of Fu organs and the Front-Mu point of the stomach. It can tonify Qi,regulate the middle Jiao, promote the circulation of Qi and blood, and remove stagnation. Guanyuan (CV 4) can benefit and consolidate the Yuan-Primordial Qi. Ca-Rubbing manipulation on the lumbosacral part can tonify the kidney, benefit the lung, promote Qi and bowel movements. These manipulations work together can benefit Qi, tonify the spleen and relax the bowel.
Umbilical therapy as one of the TCM external treatments can give full play of drugs and acupoints at the same time. The umbilicus is where Shenque (CV 8) is located. By umbilicus application, the effective components of the drugs can directly penetrate the skin around the point and be absorbed by the tissues to enhance the intestinal contraction function, stimulate the gastrointestinal nerves, and promote intestinal peristalsis, thus treating constipation. The formula Da Huang San adopted in this study, consisting ofDa Huang,
Huang LianandHuang Qin, was recorded in theWai Tai Mi Yao(Medical Secrets of an Official).Da Huangcan purge heat, remove stagnation, and especially drain the fire in the lower Jiao. Modern studies have shown that rhein inDa Huangis an effective component for purgation. Rhein can promote defecation by stimulating the peristalsis of large intestine, inhibiting the absorption of water by the intestine, and stimulating the duodenum[18-20];Huang Liancan consolidate Yin and especially drain the fire in the middle Jiao.Huang Qincan clear heat in the gallbladder and especially drain the fire in the upper Jiao. Thus, this formula functions by purging and flushing away heat to subsequently promote bowel movements.
This study showed that the total effective rate in the observation group was significantly higher than that in the control group, and the improvements of constipation and quality of life of the patients were better than those in the control group, indicating that the method of Tuina combined with umbilical therapy is better than taking lactulose oral solution in the treatment of FC. This method demonstrates the strengths of this method in alleviating constipation symptoms and improving the quality of life of the patients. In addition, it is easy to operate. With small dosage of drugs, this method will cause almost no damage to the body and thus achieve high compliance. Therefore, it is worthy of clinical promotion.
Conflict of Interest
The author declares that there is no potential conflict of interest in this article.
Acknowledgments
There was no project fund supporting this study.
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 14 September 2020/Accepted: 25 December 2020
 Journal of Acupuncture and Tuina Science2021年6期
Journal of Acupuncture and Tuina Science2021年6期
- Journal of Acupuncture and Tuina Science的其它文章
- Effects of sinew-regulating bone-setting manipulations on chondrocytes, IL-1β and NO in rabbits with knee osteoarthritis
- Efficacy observation of auricular point sticking in combination with a healthy diet for simple obesity in children
- Clinical efficacy of sticking-needle acupuncture plus tendon-regulating manipulation in the treatment of acute ankle sprain
- Therapeutic efficacy observation of warm needling moxibustion plus spine subtle adjusting manipulation for cervical radiculopathy
- Evaluation of the clinical efficacy of muscle regions of meridians needling method for refractory facial paralysis based on infrared thermal imaging technology
- Effect of acupuncture on serum PYY and nesfatin-1 in obese patients with insulin resistance
