Ocular manifestation and visual outcomes in herpes zoster ophthalmicus: a prospective study from a tertiary hospital of Eastern lndia
Mayukh Goswami, Santanu Bhattacharya, Manas Bandyopadhyay
1Department of Ophthalmology, R G Kar Medical College and Hospital, Kolkata, West Bengal 700122, India
2Department of Anatomy, Maharaja Jitendra Narayan Medical College and Hospital, Coochbehar 736101, India
Abstract
● KEYWORDS: herpes zoster ophthalmicus; conjunctivitis;episcleritis; keratitis; uveitis; optic neuritis; Hutchinson sign
INTRODUCTION
Infection with varicella-zoster virus (VZV), a neurodermotropic virus causes varicella (chicken pox), a disease that manifests as a disseminated vesicular body rash after that the virus remains latent in sensory ganglia for decades which reactivated later under certain circumstance(s) and causes new symptoms herpes zoster (shingles). Herpes zoster ophthalmicus (HZO) is caused by activated double stranded VZV (type 3). The virus reactivated in dorsal root ganglion and retrograde migration to the sensory axon of the skin to form the painful vesicular eruption, crusting and heals within 2-6wk.It typically affects dermatome supplied by ophthalmic division of trigeminal nerve (5thcranial nerve) and unilateral in nature.It may be bilateral only in disseminated zoster seen in severely immune compromised patient. Deficient immune status of the host is a primary factor for virus reactivation.
Most of immune compromised patients including human immunodeficiency virus (HIV) positive patients are at risk develop HZO[1]. Risk of VZV is 15 times greater in men with HIV than men without HIV[2]. It usually develops in elderly patients due to depressed cellular immunity.
In HZO the reactivated virus descends from the trigeminal root ganglion (gasserian ganglion) though the ophthalmic nerve,whichviadifferent branches supplies the skin of forehead, the lids, the nose and the eyeball supra orbital and supra trochlear branches are nearly always involved, nasal branch are very frequently involved rarely infra orbital branch. Many cases of HZO exhibit a prodromal period of fever, malaise, headache,and eye pain prior to eruption of the skin rash. The patient may describe eye pressure, tearing, and eye redness, of decreasing vision. Pain in the trigeminal nerve distribution may be severe.Ocular manifestation is very common with HZO such as row of vesicular skin rash and scars in the forehead lids and lid adnexa, conjunctivitis, episcleritis and scleritis, keratitis,decreased corneal sensation, iridocyclitis, secondary glaucoma,retinal involvement, multiple ocular nerve involvement and marked visual impairment in various proportions. HZO associated uveitis is usually associated with high intraocular pressure (IOP). Hutchinson’s sign was a powerful predictor of ocular inflammation and corneal denervation in HZO. The manifestations of herpes zoster skin lesions at the dermatomes of both nasociliary branches were invariably associated with the development of ocular inflammation. Zoster comes from Greek word zester, meaning “belt” or “girdle”, after the characteristic belt-like dermatomal rash. The common name for the disease, shingles, derives from the Latin cingulus, a variant of Latin cingulum meaning “girdle”. VZV belongs to the same subfamily of the herpes virus group as HSV,the viruses are morphologically identical but antigenically distinct[3]. The HZO diagnosis is clinical. It is easy in patients presenting with a typical vesicular rash, challenging when mimicked by vesicles caused by herpes simplex virus (HSV),and may be missed when skin eruptions are lacking (zoster sine herpete).
Zoster sine herpete (ZSH) refers to a condition of HZO cases in which dermatomal distribution pain occurs in the absence of an antecedent rash.
Post herpetic neuralgia (PHN) is a most important and troublesome complication, which is very tiring to the patient as well as to the physician and till date there is no single effective drug to cure this distressing problem. Acyclovir has been the oral antiviral agent approved for the treatment of patients with acute herpes zoster, its effect on post herpetic neuralgia remains controversial. Diabetic status of the patient was not checked but diabetes is the important factor in development of HZO. Pain is not included in the inclusion criteria though it is ominous sign for clinical diagnosis of the cases[4-5].
The problem is that almost all HZO ocular manifestations are per se unspecific and often indistinguishable from those occurring for other causes in general and those caused by HSV infections in particular. Yet, there is one exception, VZV epithelial keratitis. Clinically, it is the least troublesome of VZV ocular manifestations, but it occupies an outstanding position because of its typical features. VZV epithelial keratitis may precede the rash, accompany it, develop later on, and recur; in some patients, it may be the only clue revealing the true cause of their disease.
A number of HZO patients come to Hospital Out Patient Department (OPD) with different symptoms but many of them have only cutaneous symptoms without any ocular manifestation. Few ocular manifestations may have serious vision threatening outcome. Many patients are referred from skin OPD to eye OPD for checking of ocular manifestations.So the main objective of the study was to find out magnitude of different ocular manifestations of HZO cases and to measure the visual outcome of the patients after two months and to find out the lacunae of different studies on the HZO cases and to determine the percentage of vision threatening ocular manifestation of HZO cases. But the biggest challenge of this study was to take consent from the patient for follow up on regular interval and to prevent drop out of patients from the study.
SUBJECTS AND METHODS
Ethical Approval A descriptive study with cross sectional design of data collection was conducted in the Departments of Ophthalmology and Dermatology, R.G. Kar Medical College and Hospital over a period of one year. Permission from Institutional Ethics Committee was obtained. Consent and detail history were taken in every patient.
Enrolment of patient was done for a period of 10mo as the visual outcome was assessed after 2mo. All clinically diagnosed cases of HZO from the OPD of ophthalmology and dermatology were included in the study. All HZO cases are Tzanck smear positive. Physical examination was included a thorough ophthalmologic exam including external inspection, visual acuity, visual fields, extra ocular movements,papillary response, fundoscopy, IOP, anterior chamber slit lamp examination, and corneal examination with and without staining amongst others.
All patients were planned for full ophthalmological examination. This was carried out using slit lamp bio microscopy details examination of eye lid lashes, eye lid margins and adnexal area, states of conjunctiva, cornea including its epithelial integrity by fluorescent straining,corneal ulceration, status of anterior chamber, iris, papillary shape size and reaction to light, lens condition. Non-contact tonometry (NCT), applanation tonometry (AT). AT were done, if corneal epithelium is intact or there is no significant corneal oedema or blepharospasm. NCT was used where AT was not possible. Following that dilatation of pupil bilaterally with tropicamide eye drop and fundus examination were done primarily by direct ophthalmoscope then 78/90 D Volk lens in slit lamp biomicroscope for examination of central fundus which includes optic disc macula including fovea and finally the peripheral fundus up to ora serreta check-up were done by indirect ophthalmoscopy. After initial visit (‘0’ date) every patient was examined after 3d, and at the end of 1stweek from the first date of visit. Subsequent visits were conducted at the end of 2nd, 4th, 6th, and 8thweek respectively.
After collection and compilation of data, it was subsequently analysed by using Graph Pad Software Inc., San Diego, CA,USA; 2007, Microsoft Word and Excel software.
RESULTS
Among the 42 cases of HZO, 28 (66.67%) were males and 14(33.33%) were females. Among the total cases, majority of the patients belonged to the age group of 56 to 60y (21.42%). The younger age group (21-25y) was minimum (2.38%). As the age of the male patients was 24-65y and female patient was 37-70y, 45y was selected for “cut of age” between younger and older. It was also observed that the ocular manifestation became eminent with a class interval of 5y. Figure 1 nose the Hutchingson sign in an HZO case.
Out of 42 cases of HZO, only 11 cases were 45y or less(26.19%) and 31 cases were above 45y (73.81%). Out of total 11 cases of 45y or less, males were 10 (90.91%) and females were only 1 (9.09%). But among the cases of above the age group of 45y, males were 18 (58.06%) and females were 13(41.94%). So, in lower age group gender distribution of HZO cases were male predominant in this study. The distribution of study population according to gender and age is depicted in Table 1.
Out of 42 cases of HZO, 33 (78.57%) cases were found to have ocular manifestation (Table 2). Among the total 33 HZO cases 24 cases were male (72.73%) and rest 9 (27.27%) were female.The female cases had higher cutaneous involvementi.e.5 out of 9 cases (55.56%). Among the 11 cases of 45y or below, 6(54.55%) cases had distinct ocular manifestation and among the 31 cases of above 45y 27 (87.10%) cases of higher age group had distinct ocular manifestation. It was observed that ocular manifestation was predominant in older age. Among the 6 cases of HZO with ocular manifestation in 45y or below age group male were 100% (6 cases out of 6) and female was 0 case. Among the 27 cases of HZO with ocular manifestation in higher age group males were 18 (66.67%) and females were 9(33.33%).
Out of total 42 cases, 7 HIV positive cases were found. Out of total cases of 11 among 45y or below, 5 (45.45%) cases were HIV positive and out of total cases of 31 above 45y, only 2 cases (6.45%) were HIV positive. Out of 6 ocular manifested HZO cases of 45y or less, 4 cases (66.67%) were HIV positive and out of 27 ocular manifested HZO cases over 45y, only 2 cases (7.41%) were HIV positive. It was clearly observed that HIV status remained high in ocular manifested HZO cases at 45y or below age group. It was seen among the total 7 HIV positive HZO cases 6 cases have ocular manifestation(85.71%).

Figure 1 Hutchingson’s sign.

Figure 2 Skin of eye brow and adnexa involvement with conjunctivitis.
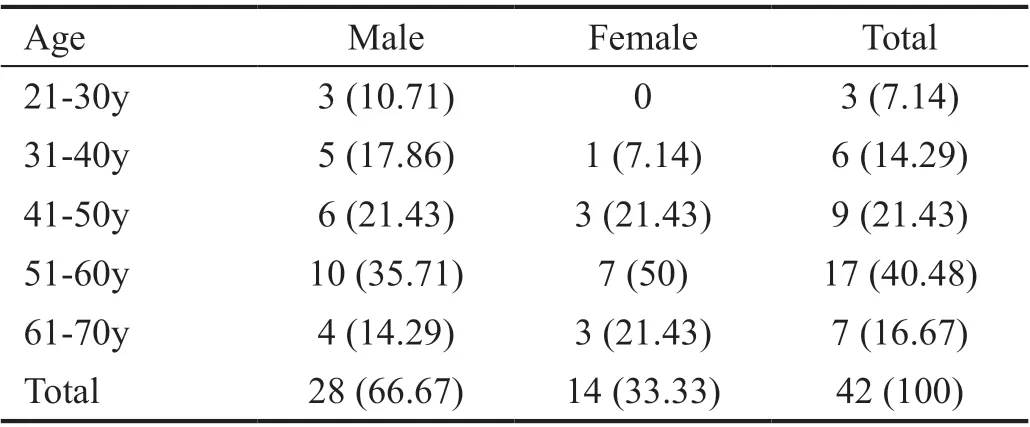
Table 1 Age and gender distribution of HZO cases n=42 (%)
Out of total 42 cases HZO, conjunctivitis was noted among most of the patient (69.05%). It was followed by keratitis overall(59.52%), epithelial keratitis (45.24%), stromal keratitis(38.10%), nummular keratitis (33.33%), anterior uveitis(30.95%). Among the patients with lid involvement, 22(52.38%) cases were male, and 9 (21.43%) cases were female(Figure 2, Table 3).
Ocular hypertension is associated with 18 cases of HZO with ocular manifestation among the total 33 cases (54.55%).IOP raised in 14 cases among total of 31 HZO cases over 45y (45.16%). Distribution of various ocular manifestations according to the age group and IOP were showed in Tables 4-5.In the present study it was seen that under 45y group vision 6/6 after 8wk was lower (7.14%) in comparison to over 45y(9.52%). Vision 6/9 was almost same (7.14%) as over 45y(7.14%). Visual outcome of affected and non-affected eyes at the end of 8wk were showed in Table 6.
DISCUSSION
Goh and Khoo[6]found the mean age of herpes zoster in theirstudy to be 48.8y. Herpes zoster usually occurs in advancing of age due to lowering of the immunity power reactivating the long-term harbouring the varicella virus in the sensory ganglion. Brănişteanuet al[7]found that 35% of patients were in the 70-80 years age. According to the study conducted by Abdul Latheef and Pavithran[8]the incidence of herpes zoster was mainly in the fourth and third decades of life. A definite history of chicken pox was present in only 63.4% cases. In the majority (70%) herpes zoster occurred spontaneously.Another study was conducted by Ghaznawiet al[9]where equal numbers of patients were affected with HZO in the younger and older age group. The most common decade of HZO onset was between 50 and 59y. Younger patients were more likely to be healthy compared with older patients. In our study it has also been shown that males are more affected than females. So herpes zoster is the male predominant disease. This is to some extent similar with different hospital-based clinical study of herpes zoster conducted by Adhicari and Agarwal[10]where the herpes zoster cases included 71 males and 42 females and the male:female ratio was 1.69:1. In another study of Chandrakala and Tharini[11], it was seen that out of 100 cases, 72 were males and 28 were females and the sex ratio was 2.5:1. Age wise distribution showed that 73 cases were below the age of 50 and 27 were above the age of 50y. Ten males were there out of 11 cases of HZO. The cause of high male dominance of HZO patients in younger age may be due associated HIV positive status. This finding is close to study conducted by Opsteltenet al[12]. He showed that the incidence was greater in females in the middle-aged and youngest group. Gender effect was inverse in young adults. In our study only one person under 25y affected among the total 42 patients. In our study it is revealed that ocular manifestation of HZO is more with advancing age and female involvement also more with advancement of age, but male have more ocular manifestation irrespective of age group. Out of 6 oculars manifested HZO cases under and equal to 45y, 4 cases (66.67%) were HIV positive and out of 27 ocular manifested HZO cases over 45y only 2 cases (7.40%) were HIV positive. According to the study of Sandoret al[13]HZO occurred with frequent ocular complications in a subgroup of adults distinguishable by their young age. Over the study duration, 21% (three of 14) of the AIDS-risk subgroup patients have developed AIDS with a 14% (two of 14) mortality.

Table 2 Distribution of study population according to gender and ocular manifestation of herpes zoster cases n=42 (%)

Table 3 Distribution of various ocular manifestations among the HZO cases n=42
In another study of by Adepoguet al[14]26 seropositive patients were in 20 to 49 years of age and half the patient had HZO manifestation. Maiya and Shenoy[15]demonstrated that advancing age was the most common predisposing factor.Acute neuralgia and skin lesions were the most common modes of presentation. Ocular involvement was seen in 16 (59.25%)of the patients with HZO. Cornea was the commonest ocular structure (62.5%). It was also observable that disciform keratitis (19.04%) was near most half of the nummular keratitis incidence. Liesegang[16]told that a nummular anterior stromal keratitis could develop, which usually resolved or became chronic. Puriet al[17]reported that ocular manifestations in HZO were present on 68 patients. Among them pain (77.9%)was the commonest ocular complaint. Visual status was good in the majority (73.5%) of patients at presentation. Lid and adnexal findings (45.8%) were most common ocular involvement followed by conjunctivitis (41.1%). Corneal complication was seen in 38.2% of cases, uveitis in 19.1% and post-herpetic neuralgia and secondary glaucoma each in 5.8%.Yawnet al[18]conducted a cohort study where 184 patients(9.0%) had eye involvement. Common eye complications were keratitis (76.2%), uveitis/iritis (46.6%) and conjunctivitis(35.4%). Recurrent keratitis and recurrent iritis/uveitis occurred in 6.9% and 7.4% respectively. Outcomes included six (3.3%) patients with new vision decrements to 20/200 or worse. Six (3.3%) individuals had lid ptosis. No one developed acute retinal necrosis (ARN). Significant visual outcome may not be expected from this study due to relatively small sample size, short time and other factors affective the visual outcome like cataract, macular pathologyetc. are not excluded. This finding can be correlate with other studies like Kahlounet al[19]where ocular manifestations included adnexal involvement(58.8%), keratitis (31.4%), keratouveitis (31.4%), isolatedanterior uveitis (29.4%), IOP elevation (23.5%), oculomotor nerve palsy (5.8%), and optic neuritis (1.9%). Isolated anterior uveitis, isolated keratitis (P=0.001), and IOP elevation were more likely to be concomitant to HZO active skin disease,while keratouveitis occurred more likely more than 1mo after HZO eruption. Anterior uveitis and keratouveitis were more likely to be associated with age ≥50y. Ocular complications included neurotrophic keratopathy (1.9%), corneal opacity(5.9%), secondary glaucoma (7.8%), optic atrophy (1.9%),and post herpetic neuralgia (13.3%). Mean follow-up was 12mo. Mean final best corrected visual acuity was 20/32; it was ≥20/40 in 78.4% of the eyes. Szetoet al[20]conducted a retrospective study where ocular manifestations were present in 170 (65.6%) patients. Conjunctivitis was the most common ocular manifestation, followed by anterior uveitis and keratitis.After resolution of HZO, 58.7% of patients had a visual acuity of 6/12 or worse. Epithelial keratitis and stromal keratitis were independent risk factors for visual loss after resolution of HZO. Another study conducted by Nithyanandamet al[21]where overall visual outcome was good, with 36/64 (56.3%).The mild, moderate, and severe visual loss occurred in 22/64(34.3%), 3/64 (4.7%), and 3/64 (4.7%) respectively. Moderate to severe visual loss was due to severe uveitis, neurotrophic keratitis, and cataract. Increasing age was significantly associated with visual loss. Uveitis was found to be the best predictor of visual loss in HZO on multivariate analysis. Viral retinitis was a rapidly progressive condition that may involve the entire retina and lead to severe loss of vision.

Table 4 Distribution of various ocular manifestations according to the age group n=42 (%)
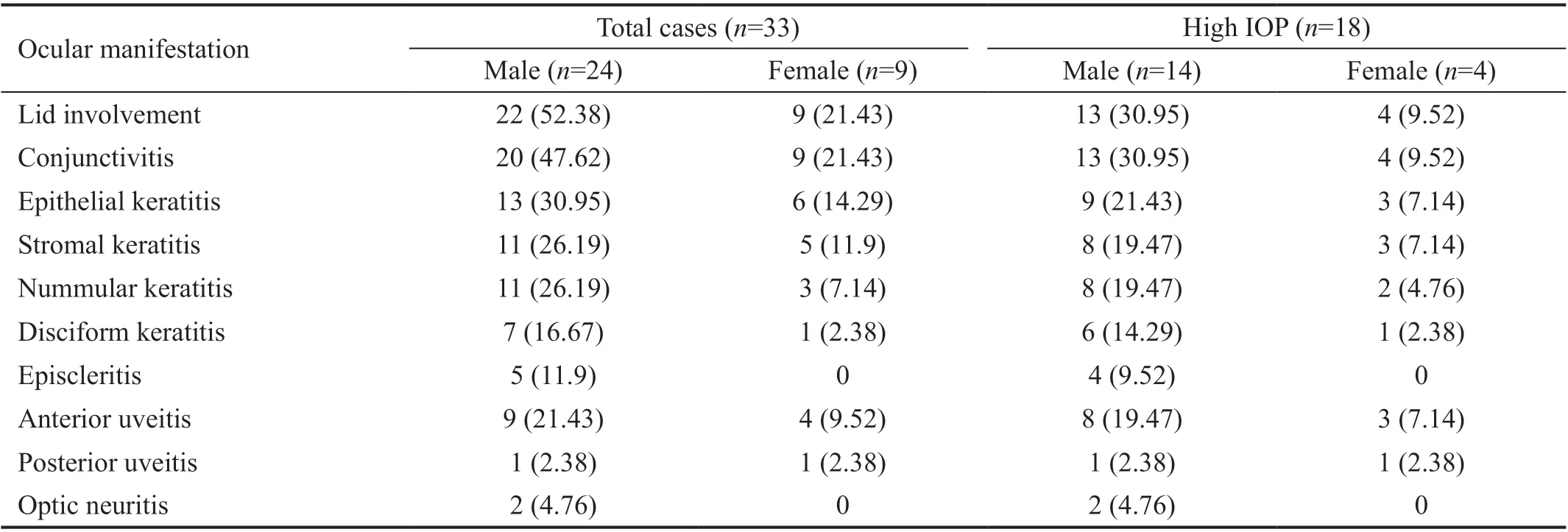
Table 5 Distribution of various ocular manifestations in HZO cases according to gender and IOP n=42 (%)
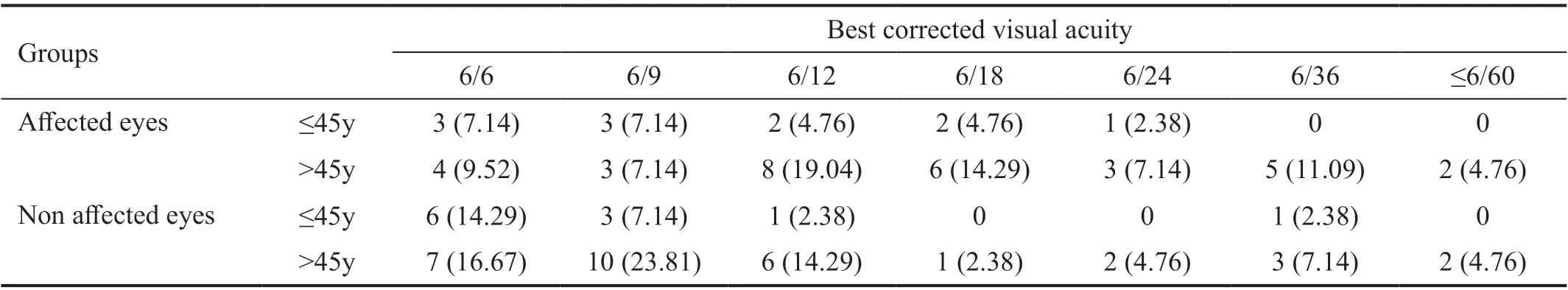
Table 6 Visual outcome of affected and non-affected eyes at the end of 8wk n=42 (%)
The aetiological agents include cytomegalovirus (CMV),VZV, HSV, and rarely Epstein-Barr virus (EBV). ARN may occur in immune-competent individuals and is characterised by confluent, peripheral, necrotising retinitis, peripheral occlusive arteritis and moderate-to-severe vitritis. Progressive outer retinal necrosis usually occurs in immune-compromised patients and can lead to the rapid involvement of the peripheral and central retina by full thickness necrosis with severe loss of vision from retinal detachment and optic neuropathy. In our study we did not found a single case of retinal involvement.Forsteret al[22]reported two patients, both seropositive for the HIV, developed rapidly progressive retinal necrosis associated with a systemic herpes zoster infection.
Kumaret al[23]conducted a study on 35 patients where 28.57%cases were in age group 41-50y and the male cases were 54.28%. The patients were followed on 7, 14, 30d and 3mo after first visit. So, the frequency of the visit was less than the present study. According to them conjunctivitis (77.1%)and corneal involvement (60%), episcleritis (8.6%), uveitis(57.1%), and secondary glaucoma (5.7%) were common manifestations of HZO. Hutchinson’s signs was positive in 18 cases. Corneal involvement and uveitis with Hutchinson’s signs were observed in 48.57% and 14.28% cases respectively.The 57.14% patients had no visual loss at 3mo follow up, and 85.71% had vision 6/18 or better. But they did not report any association with HIV[23].
Niedereret al[24]reported ocular involvement of HZO in 84.8% cases. In his study corneal involvement, uveitis, and vision loss (<20/50) were found in 51.2%, 47.6%, and 9.6%cases respectively. But this retrospective cohort study had certain limitations like subjective or recall bias. Another study was conducted by Tuli[25]where follicular conjunctivitis was reported as the commonest manifestation of HZO. Zhenget al[26]conducted a retrospective cohort study including 87 673 patients above 50y (from 2010 to 2018). They compared the characteristics HZO and non HZO among herpes zoster patients and factors associated with ocular manifestations by an automated natural processing algorithm. They found 9% ocular herpes zoster cases among all HZO cases. But the study design was devoid of direct patient contacts or follow up. Li[27]conducted a study on HZO includes acute keratitis as an ocular manifestation and permanent vision loss due to it.Early diagnosis and management by oral and topical antiviral medication may help to reduce the potentially devastating complication.
The present study reported that the HZO cases occurred more in advanced of age group (73.80% patients were above 45 years of age). The 78.57% patients of HZO had ocular manifestations. Ocular manifestations of HZO cases were also common above 45y (87.09% cases). Young patients were affected more with associated HIV infection (45.45%) and at the same time the HIV positive HZO cases also suffered more with ocular manifestations (85.71%). HZO cases were twice common among males (66.67%). Ocular manifestations were observed more in males (72.72%). All female patients were over 45 years of age. Ocular hypertension was associated with almost every type of ocular manifestations and IOP raised in 54.54% patients with ocular manifestations. IOP was also more in elderly patients (45.16%). Ocular manifestations were lid involvement (73.80%), conjunctivitis (69.04%), episcleritis(11.90%), keratitis (59.52%), anterior uveitis (30.95%),posterior uveitis (4.76%). Four types of keratitis were found in the study: keratitis (45.23%), stromal keratitis (38.09%),nummular keratitis (33.33%), and disciform keratitis (19.04%).Retinal involvements were not found in this study. Visual outcome was poor in the affected eye of elderly patient (>45y)and was associated with keratitis, anterior uveitis, posterior uveitis and optic neuritis primarily.
The present study depicts the scenario of HZO cases and its ocular manifestation in a tertiary hospital in Eastern India. It also helps to generate a clear conception regarding the type of ocular manifestations and magnitude of ocular manifestations in HZO patients of Eastern India. The causes of vision threatening consequences of HZO patients, type and magnitude of keratitis associated with HZO, relation between raised IOP and HZO,relation with HIV positive cases are also revealed. This study can help the clinician and ophthalmologist in their judgement and presumptive assessment of the HZO cases in OPD.
ACKNOWLEDGEMENTS
Conflicts of Interest:Goswami M, None; Bhattacharya S,None; Bondopadhyay M, None.
 International Journal of Ophthalmology2021年12期
International Journal of Ophthalmology2021年12期
- International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
