An unusual case of malignant glaucoma with ciliary detachment
Qian-Qian Xu, Wei-Wei Wang, Juan Zhu, Jian-Rong Liu
Dear Editor,
I am writing this letter to present an unusual case of malignant glaucoma with ciliary detachment.
Malignant glaucoma has an incidence of 0.6%-4% and mostly occurs after filtering surgery for primary angle-closure glaucoma. After surgery, the intraocular pressure (IOP)does not decrease but increases, and the anterior chamber(AC) becomes shallower or disappears. There is an obvious ophthalmodynia, and the disease rapidly worsens, thus seriously threatening the visual function of patients[1-3]. So far, no cases of malignant glaucoma combined with ciliary detachment have been reported. Complete comprehension of the symptoms of malignant glaucoma with ciliary detachment is crucial for preserving the patients’ visual function, diagnosing the disease at the early stage, and conducting correct and effective treatment.
This study was approved by the Institutional Review Board of Xi’an People’s Hospital (Xi’an Fourth Hospital). Written informed consent to participate and publication was obtained from the patient.
A 76-year-old male patient was referred to our hospital for ocular pain and blurred vision of 4 days duration after trabeculectomy of the right eye in another hospital. After the operation, the IOP did not decrease. However, the ophthalmodynia aggravated, and the vision was failing. Then,the patient visited the ophthalmic outclinic of our hospital on April 15, 2020. He had a five-year history of hypertension that was put under control after taking nifedipine extended-release tablets. The best corrected visual acuity (BCVA) was hand motion (HM)/30 cm, and the IOP was 35.0 mm Hg after taking two eye drops (carteolol twice a day and brinzolamide amine twice a day). Slit lamp revealed severe conjunctival hyperemia,flat filtering bleb (Figure 1A), and nearly clear cornea with approximately 0.5 corneal thickness (CT) central AC depth and disappeared peripheral AC (Figure 1B). The pupil was irregular and about 8 mm in diameter (Figure 1C), and there was no pupillary response. Iris partial posterior synechia and lens opacity (C2N2P1) were observed with asteroid hyalosis in the vitreous (Figure 2). The cup-disc ratio was about 0.5(Figure 3) and epiretinal membrane was seen in the macular area (Figure 4). In the left eye, the BCVA was 2/20 with the IOP of 17.8 mm Hg. Slit lamp revealed mild conjunctival hyperemia and clear cornea with a shallow AC. The pupil was circular and about 3 mm in diameter with normal pupillary response and lens opacity (C2N2P1). There was nothing wrong with the vitreous and retina.
In the ophthalmic outclinic, for his right eye, besides carteolol and brinzolamide amine, two more eye drops (both brimonidine tartrate and atropine three times a day) were given with subconjunctival injection of mydriasis mixture (atropine 0.1 mL + adrealine 0.1 mL + lidocaine 0.1 mL). After a routine blood test, COVID-19 and chest computer tomography examination, the patient was admitted to the hospital on April 16, 2020, suspected of malignant glaucoma in the right eye.
Then, the BCVA was slightly improved to counting fingers(CF)/40 cm and the IOP dropped to normal of 17.5 mm Hg in the right eye after taking IOP-lowering drugs and cycloplegic agents. Slit lamp revealed slightly deeper central AC depth than before. There were no other changes compared with the examinations on April 15. Ultrasound biomicroscopy (UBM)showed that the central AC depth was extremely shallow, the peripheral AC disappeared, and the anterior angles in four quadrants were closed with ciliary detachment (Figure 5A,5B) in the right eye. In the left eye, the AC was shallow; the anterior angle in the lower quadrant was closed while those in the other quadrants were narrow (Figure 5C, 5D). The axial length/lens thickness measured by IOL Master 700 was 21.74/5.19 mm in the right eye, and 22.23/5.15 mm in the left eye. Specular microscopy revealed corneal endothelium cell densities of 1454 cells/mm2in the right eye and 2957 cells/mm2in the left eye; hexagonal cell ratio of 24% in the right eye and 73% in the left eye. A diagnosis of malignant glaucoma with ciliary detachment, asteroid hyalosis, macular membrane and cataract in the right eye was made.
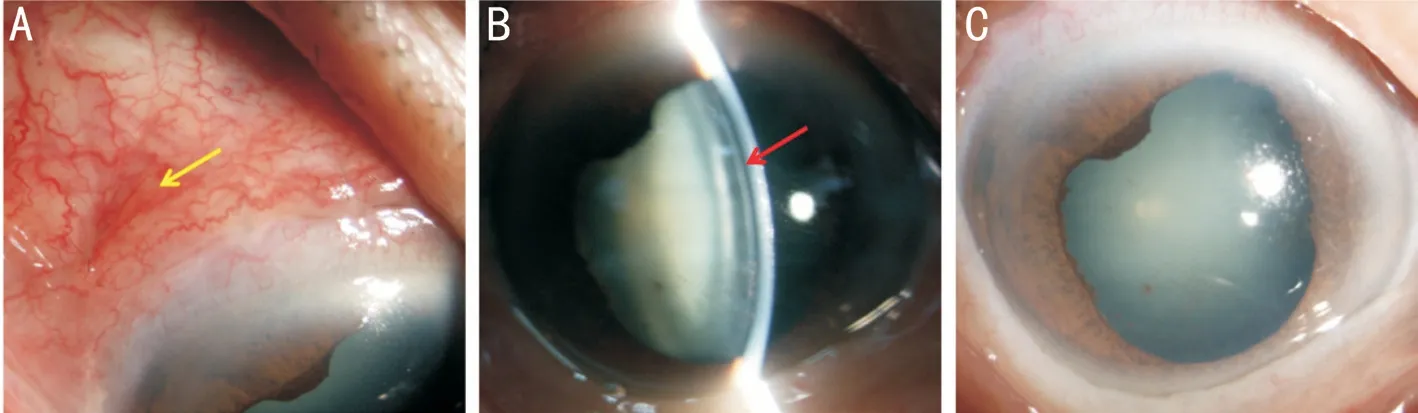
Figure 1 Biomicroscopic images of the right eye from the first visit A: Severe conjunctival hyperemia, flat conjunctival bubble (yellow arrow) after trabeculectomy; B: Nearly clear cornea with approximately 0.5 CT central AC depth (red arrow) and lens opacity (C2N2P1); C:Irregular pupil with 8 mm in diameter and posterior synechia, and iris hole couldn’t be seen because of arcus senilis.

Figure 2 B-scan ultrasound A: Asteroid hyalosis (arrow) in the vitreous of the right eye; B: No abnormalities in the left eye.

Figure 3 Fundus photo with an ultrawide view A: The cup-disk ratio was about 0.5 with asteroid hyalosis (black arrow) in the vitreous in the right eye; B: The cup-disk ratio was about 0.3 in the left eye.
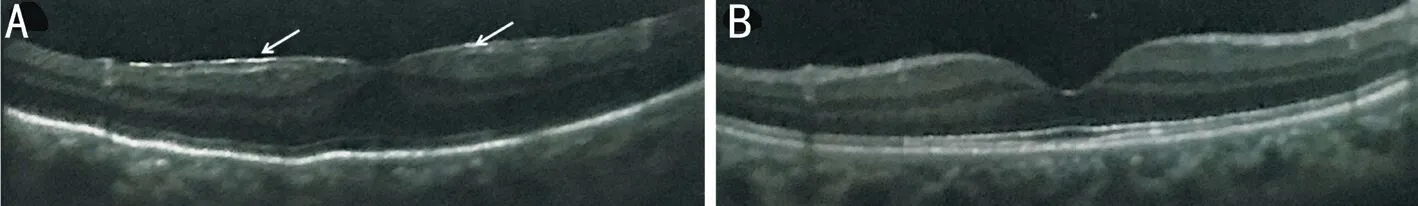
Figure 4 Optical coherence tomography images A: Epiretinal macular membrane (arrows) in the right eye; B: No abnormalities in the left eye.
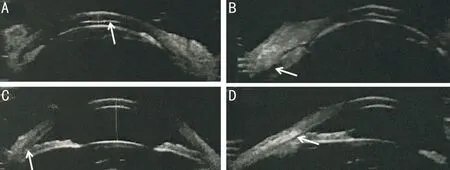
Figure 5 Ultrasound biomicroscopy images A: Extremely shallow of the central AC depth (arrow) with disappeared peripheral AC in the right eye; B: Closed anterior angle with ciliary detachment (arrow) in the right eye; C: Closed anterior angle (arrow) in the left eye; D: Narrow anterior angle (arrow) in the left eye.
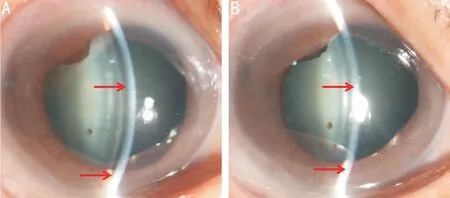
Figure 6 Biomicroscopic images of the right eye after pharmacotherapy A: Deeper central AC depth of about 1 CT (red arrow) on April 17; B:Disappeared AC (red arrow) on April 20.
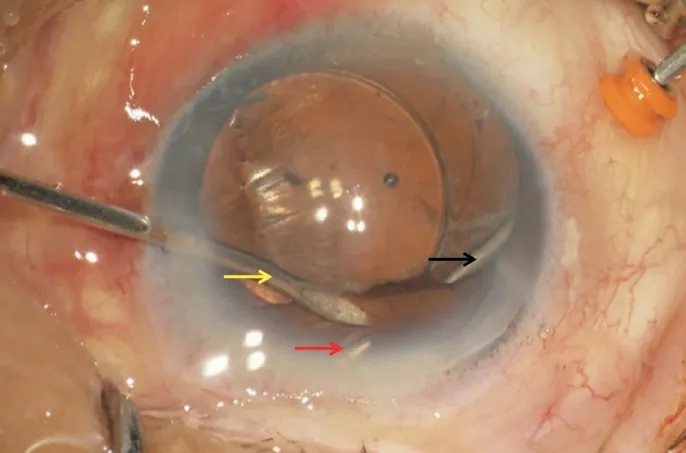
Figure 7 Biomicroscopic images during anterior vitrectomy of the right eye With anterior irrigation by a needle (yellow arrow), 23-gauge vitrectomy probe(black arrow) was inserted through a sclerotomy incision to do zonulo-hyaloido-vitrectomy through a peripheral iridectomy (red arrow).
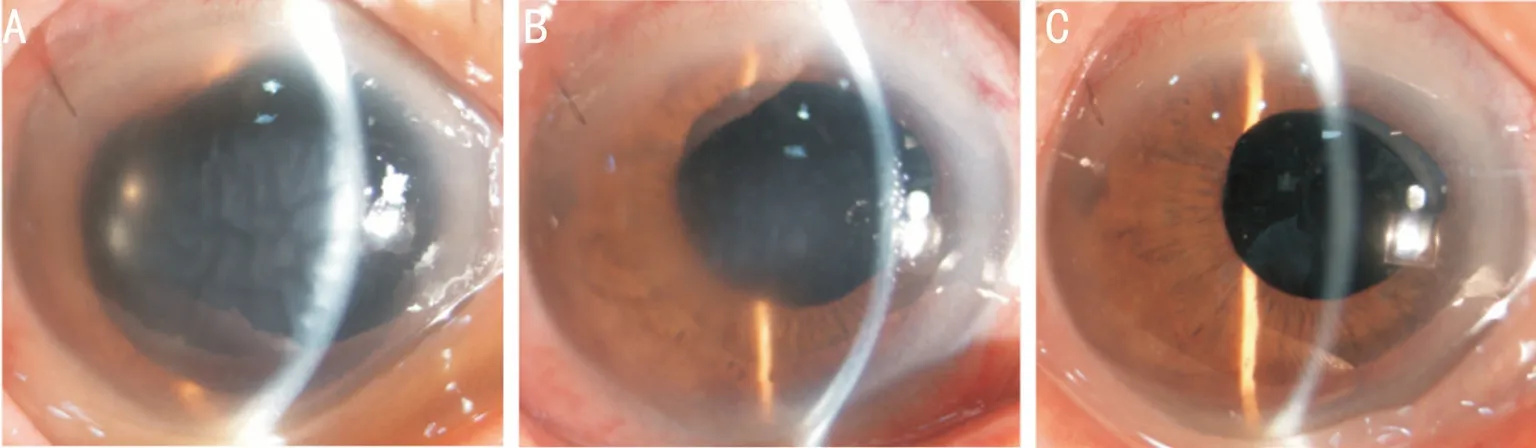
Figure 8 Biomicroscopic images of the right eye postoperatively A: Mild corneal edema and deep AC on the first day postoperatively; B:Significantly relieved corneal edema and deep AC on the fourth day postoperatively; C: Clear cornea and deep AC one month later.
On April 17, slit lamp revealed deeper central AC depth of about 1 CT in the right eye (Figure 6A). However, on April 20, the AC depth disappeared in the right eye (Figure 6B).Phacoemulsification and intraocular lens implantation combined with anterior vitrectomy were carried out in the right eye. A 23-gauge vitrectomyviapars plana was performed to push the lens iris diaphragm backward. After a continuous curvilinear capsulorrhexis of approximately 6.0 mm in diameter, phacoemulsification was performed with a 24.0 D intraocular lens (ZA9003) implanted into the capsular bag.Then, zonulo-hyaloido-vitrectomy through a peripheral iridectomy was carried out to disrupt the anterior hyaloid membrane ensuring aqueous outflow from the vitreous cavity into the AC in order to interrupt the ciliolenticular block(Figure 7). On the first day postoperatively, the visual acuity was CF/50 cm, and the IOP was 21.5 mm Hg (without any IOP-lowering drops) with mild corneal edema and deep AC in the right eye (Figure 8A). The patient’s right eye was treated with levofloxacin eye drops six times a day, tobramycin dexamethasone eye drops six times a day, and tropicamide eye drops three times a day. On the fourth day after surgery,the visual acuity was 20/100, and the IOP was 9.8 mm Hg with significantly relieved corneal edema (Figure 8B). Thus,levofloxacin eye drops and tobramycin dexamethasone eye drops were adjusted three times a day, and tropicamide eye drop was stopped. One month after discharge, the BCVA was 20/50, and the IOP was 10.3 mm Hg with clear cornea and deep AC in the right eye (Figure 8C). UBM showed that the ciliary body of the right eye was reset. At a one-year followup, the patient’s condition was stable.
DISCUSSION
The exact pathophysiological mechanism of malignant glaucoma remains unclear[1,4]; yet, it mainly involves the theory of the stray flow of the aqueous humor and choroidal expansion. Most scholars believe that the occurrence of malignant glaucoma is closely related to the special ophthalmic anatomy, such as small eyeball, short eye axis, narrow-angle,rotation of ciliary process, relatively large lens,etc[1-2,5-9]. The abnormal anatomical relationships among lens, ciliary body,and anterior vitreous lead to the ciliolenticular block and aqueous misdirection into the vitreous. The pressure in the vitreous increases and pushes the lens iris diaphragm forward,thus leading to malicious circulation and resulting in malignant glaucoma.
Once a patient is diagnosed with malignant glaucoma,immediate measures must be taken to resolve the ciliolenticular block, recover the AC and reduce IOP. The medical treatment, including cycloplegic agents, IOP-lowering drops, and glucocorticoid anti-inflammatory treatment, is the initial treatment that can alleviate the disease of 50% of patients. However, as the recurrence rate is high, maintenance treatment of atropine eye drop is needed[1-2,7-9]. Chandler and Grant[10]reported for the first time on the use of pars-plana fluid aspiration to treat malignant glaucoma. This kind of operation is relatively simple, but it cannot completely resolve the ciliolenticular block. Phacoemulsification combined with anterior vitrectomy can resolve ciliolenticular block,and recreate the normal pathway of aqueous humor. It can further push the misdirected aqueous humor that flows into the vitreous cavity to circulate to the AC and drain out of the eye through a functional angle or filtering channel so as to fundamentally cure malignant glaucoma[1-2,5,7-9,11].
Our patient underwent a trabeculectomy of the right eye in another hospital. Four days postoperatively, the ophthalmodynia aggravated, the AC depth became shallower, and the IOP remained high. Then, the patient was referred to our hospital.UBM showed that the anterior angle of each quadrant was closed, the central AC was very shallow with disappeared peripheral AC, and the lens iris diaphragm moved forward.Combined with the medical history and ocular examinations,the patient was suspected of malignant glaucoma. After immediate anti-inflammatory and cycloplegic treatment,the patient’s IOP dropped to normal but ciliary detachment occured. The AC depth was deeper than that at initial when it was 0.5 CT and then disappeared onoperation day. This indicated that the dropping of IOP was caused by ciliary detachment, while the ciliolenticular block had not been disrupted. The possible reasons of ciliary detachment were analyzed as follows[12]: first, high IOP caused blood circulation disorder in the anterior part of the eye, leading to ciliary edema and inflammatory reaction; second, due to the timely treatment,the IOP rapidly dropped, and choroidal vascular leakage increased, leading to the increase of supraciliary effusion. As a result, ciliary detachment appeared. If the IOP of the patients with malignant glaucoma decreases after medical treatment while the AC does not deepen, the possibility of ciliary choroidal detachment should be ruled out. Ocular B-ultrasound and UBM examination can help for the diagnosis.
In order to completely resolve the ciliolenticular block, the patient underwent phacoemulsification and intraocular lens implantation combined with zonulo-hyaloido-vitrectomy through a peripheral iridectomy. Considering the patient has 360° ciliary detachment, the puncture which was performed in the pars plana should be accurately placed to avoid puncture into the upper cavity of the ciliary. After operation, AC depth of the patients recovered to normal, the BCVA increased to 20/50, and the IOP decreased to the normal range. At the oneyear follow-up, the patient’s condition was stable.
In conclusion, the exact pathogenesis of malignant glaucoma can be defined as complex, being closely related to the abnormal anatomical relationship among lens, anterior vitreous,and ciliary body. Various blocking factors may simultaneously exist or appear one after another with the progress of the disease. The key to successful treatment is to remove the existing blocking factors. High IOP can cause blood circulation disorder in the anterior segment, leading to ciliary edema and inflammatory reaction, inducing ciliary detachment and reducing IOP to normal. After ciliary detachment, the AC is shallower or even disappears, and the condition deteriorates,which requires immediate surgery to restore the AC, resolve the ciliolenticular block and promote the resetting of the ciliary.Cataract phacoemulsification combined with zonulo-hyaloidovitrectomy through a peripheral iridectomy in the treatment of malignant glaucoma has the following benefits: the AC is deeper, the IOP is stable, and the ciliary detachment is reset; it can result in improved vision in most patients. Therefore, it is an effective method for the treatment of malignant glaucoma.
ACKNOWLEDGEMENTS
Authors’ contributions: Xu QQ and Wang WW contributed to patient care, literature search, and writing of the report. Zhu J and Liu JR contributed to data analysis. All authors have read and approved the final manuscript.
Foundations: Supported by the National Natural Science Foundation of China (No.81500719); Shaanxi Province Innovation Talents Promotion Plan (No.2018KJXX-091);Research Incubaiton of Xi’an People’s Hospital (Xi’an Fourth Hospital) (No.BS-2).
Conflicts of Interest:Xu QQ, None; Wang WW, None; Zhu J, None; Liu JR, None.
 International Journal of Ophthalmology2021年12期
International Journal of Ophthalmology2021年12期
- International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
