Efficacy and safety of non-penetrating glaucoma surgery with phacoemulsification versus non-penetrating glaucoma surgery: a Meta-analysis
Jun-Yan Xiao, An-Yi Liang, Yue-Lin Wang, Gang-Wei Cheng, Mei-Fen Zhang
Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
Abstract
● KEYWORDS: cataract; glaucoma; non-penetrating glaucoma surgery; phacoemulsification; Meta-analysis
INTRODUCTION
Glaucoma and cataract are the most common causes for visual loss and commonly coexist[1-4]. Visual field loss in glaucoma cases is associated with elevated intraocular pressure(IOP) and the control of IOP is the only factor to decrease glaucoma progression. Surgery may be indicated if IOP could not be controlled despite maximal medical therapy.
The most widely performed surgery to reduce IOP worldwide is trabeculectomy, which establishes a passage between subconjunctival space and anterior chamber[5]. Surgical treatment of this condition has limitations including the need to destroy healthy structures and it is also limited by adverse outcomes like shallow anterior chamber, ocular inflammation,and hypotony[6-7]. And the estimated 5-year cumulative failure rate of trabeculectomy was 47%[8]. Therefore, novel surgical approaches are required. Non-penetrating glaucoma surgery(NPGS), namely, viscocanalostomy (VC), canaloplasty(CP), CO2laser-assisted sclerectomy surgery (CLASS), deep sclerectomy (DS), gradually developed as an alternative to traditional filtering procedures[9-11]. By strengthening natural aqueous outflow channels, those surgeries achieved reducing IOP with fewer complications[11-12].
With the aging of the world society, more patients with glaucoma accompanied by cataracts need surgical treatment[13].One way to solve this problem is to combine surgery.However, there were controversies about the optimal time to perform phacoemulsification (Phaco) and the best way to manage these patients[14-15], since phaco is known to adversely affect IOP control after trabeculectomy[16]. And trabeculectomy combined with phaco usually has poor surgical outcomes.Cataract surgery is well tolerated and the success rates have been improved with reduced complication rates in recent years.These benefit make phaco an attractive strategy in patients with comorbid glaucoma and cataract. Whether modern small incision phaco surgery allows a less hazardous profile of combined surgery remains a debated issue[17-18].
There are no previous studies that have assessed surgical outcomes between Phaco-NPGS, including phaco plus canaloplasty (PCP), phaco plus viscocanalostomy (PVC),phaco plus deep sclerectomy (PDS), and NPGS-alone. Hence,to help address these areas of contention, this study aimed to examine the efficacy and safety of Phaco-NPGS versus NPGSalone by systematically analyzed. Efficacy was examined from two aspects: IOPs and medication decrease. Postoperative procedures, complications of the surgery, and surgical success were utilized to determine safety.
MATERIALS AND METHODS
The Meta-analysis was performed strictly and followed the guideline named the Preferred Reporting Items for Systematic Reviews and Meta-analysis Statement[19].
Evidence Acquisition Two independent researchers (Xiao JY and Liang AY) searched the PubMed, EMBASE, and Cochrane Library databases. Data were last updated in March 2021. The following key terms and Medical Subject Headings(Mesh) were used: “non-penetrating surgery”, “non-penetrating procedures”, “viscocanalostomy”, “deep sclerectomy”,“canalostomy”, “CO2 laser-assisted sclerectomy surgery”,“CLASS”, “cataract surgery”, “phacoemulsification”, “ocular hypertension”, “open-angle glaucoma”, and “Pigmentary Glaucoma”. Data obtained were entered into EndNote X8 (Thomson Reuters, New York, NY, USA). Additional publications were identified from the reference list of articles obtained. All publications were included regardless of language.
Selection Criteria Eligible studies included: 1) patients diagnosed with pseudoexfoliation glaucoma (PEG), primary openangle glaucoma (POAG), pigmentary glaucoma (PG),exfoliation glaucoma (XFS), chronic narrow-angle glaucoma(CACG), or normal-tension glaucoma (NTG); 2) The indication for combined Phaco-NPGS was the presence of a visually disabling cataract and above the diagnosis of 1 with uncontrolled IOP eyes; 3) Phaco-NPGS was compared with NPGS-alone; 4) Six months or longer follow-up period;5) Researches reported quantitative data with one or more of these outcomes: IOP values, number of antiglaucoma medications, surgical success rate, the incidence of needling or goniopuncture and the prevalence of complications; 6)The methodology needed to be a comparative clinical study,regardless of retrospective, prospective, or randomization.
Studies were excluded if: 1) They comprised patients with uveitic glaucoma, juvenile, congenital or pediatric glaucoma,neovascular glaucoma, or post-penetrating keratoplasty glaucoma; 2) The study involved the use of antimetabolites and any type of implant during surgery; 3) Letters to the editor,comments, reviews, or other documents lacking original data; 4) Articles that were considered not relevant by the investigators.
Data Extraction Initial analysis involved reading abstracts and titles, and the full-text screening to determine the eligibility of studies. Liang AY and Xiao JY obtained and examined retrieved data, such as publication year, design, first author’s name, study location, type of glaucoma, average age,details of the surgical procedure, and follow-up periods. The primary outcomes were postoperative IOP and the number of antiglaucoma medications. Secondary outcomes were efficacy in terms of the surgical success rate, complication levels,and incidence of goniopuncture or needling. Disagreements between the authors would lead to the involvement of the corresponding author (Zhang MF) until consensus was achieved.
Quality Assessment Newcastle-Ottawa Scale (NOS) was used to explore the quality of included cohort studies. Eight domains concerned were observed: 1) level of follow-up of cohorts; 2) ascertainment of exposure; 3) selection of the non-exposed cohort; 4) illustration that the outcomes of interest do not exist at the initial stage of the study; 5) based on the comparability of queues designed or analyzed; 6)examination of the outcome; 7) whether the follow-up time is long enough to ensure the occurrence of the results, and 8)representativeness of the exposed cohort. The domains were graded as “low risk of bias”, “high risk of bias” or “unclear risk of bias”.
Statistical Analysis The Meta-analysis was performed with RevMan software (version 5.4; Cochrane Collaboration,Oxford, UK). Continuous scale variables were presented as mean±standard deviation (SD). Weighted mean difference(WMD) and the 95% confidence interval (CI) were determined for continuous variables. The statistical heterogeneity was determined with a Chi-squared test andI2, withP<0.05 andI2>50% showing significant heterogeneity[17]. Data with low heterogeneity low (I2≤50%) were analyzed with a fixed-effects model, whereas those withI2>50% were analyzed with a random-effects model[18]. Begg’s funnel plot and Egger’s linear regression tests were used to determining publication bias by Stata/SE version 12 (StataCorp, College Station, TX, USA).P<0.05 was considered statistically significant.
RESULTS
Study SelectionOne hundred and forty-six articles were initially retrieved in this study. A total of 27 duplicate studies were removed, titles and abstracts were screened, and 91 unrelated articles were excluded. A total of 8 studies met the inclusion criteria[20-27]. The study selection process is presented in Figure 1. One study had 2 eligible groups and therefore,provided 2 comparisons for this Meta-analysis.
Features of Included Studies We identified studies comparing PVC (n=313 eyes) with VC (n=177 eyes), PDS(n=61 eyes) with DS (n=78 eyes), and PCP (n=50 eyes)with CP (n=125 eyes). We did not use other combinations of PVC, PDS, PCP, VC, DS, and CP for research. We included 1 randomized, 3 retrospective, and 4 prospective studies. A mixed group of glaucoma subtypes was included in all studies.One study was a multicenter, international prospective clinical trial conducted in the United States and Germany. Six studies were performed in Europe (the UK,n=3; Germany,n=1;Spain,n=1; Turkey,n=2). Two groups were excluded from a study with 4 groups during this Meta-analysis as it reported data of eyes that were duplicated in another study[20]. The main features of included studies are presented in Table 1. All studies with scores ranging from 7 to 9, were considered highquality studies (NOS score>7).Primary Outcomes Analyzed
Postoperative IOP values The postoperative IOP values at the 12-month follow-up were compared across 7 studies between the Phaco-NPGS and NPGS-alone groups. In total,230 eyes underwent Phaco-NPGS and 281 received NPGSalone. IOP was significantly lower in the Phaco-NPGS group compared with that in the NPDS-alone group (WMD=-1.12,95%CI: -2.11 to -0.12,P=0.03; Figure 2). Egger’s regression intercepts were 2.10 (95%CI: -5.68 to 9.89,P>|t|=0.52), which indicated no publication bias.
Postoperative numbers of medications At the 12-month follow-up, the postoperative number of medications was reported by four of the enrolled studies. The Phaco-NPGS group showed a significantly lower number of medications compared with that in the NPGS-alone group (WMD=-0.31,95%CI: -0.53 to -0.09,P=0.006; Figure 3). Analysis showed Egger’s regression intercepts at -0.54 (95%CI: -7.79 to 6.71,P>|t|=0.78), which revealed no publication bias.
Secondary Outcomes of the Meta-Analysis
Prevalence of complications The findings showed that the Phaco-NPGS group had a significantly lower prevalence of complications compared with that in the NPGS-alone group(WMD=0.52, 95%CI: 0.31 to 0.88,P=0.01; Figure 4). These studies reported a wide range of complications ranging including hyphema, bleb fibrosis, hypotony, iris prolapse, and choroidal detachment. Among these, only the prevalence of bleb fibrosis was statistically significantly higher in NPGSalone than in Phaco-NPGS (RR=0.12, 95%CI: 0.02 to 0.66,P=0.01; Figure 4). Analysis showed Egger’s regression intercepts at -0.34 (95%CI: -0.98 to 0.29,P>|t|=0.26). No publication bias was observed.
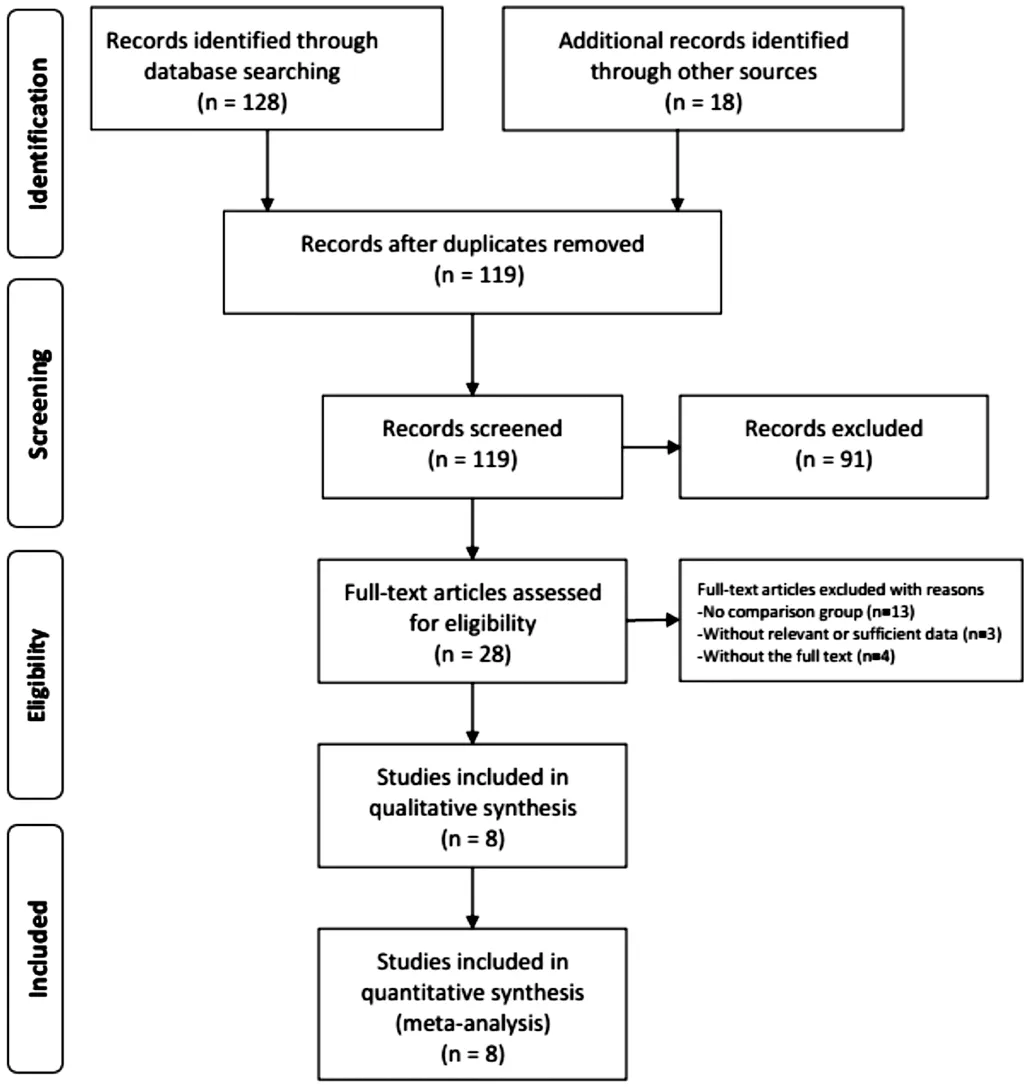
Figure 1 A representation of the study selection process.
Needling or goniopuncture Four studies reported the need for goniopuncture or needling postoperatively. Totally 283 eyes received Phaco-NPGS whereas 286 underwent NPGSalone. Phaco-NPGS group had a significantly lower prevalence of postoperative procedures compared with that in NPGSalone. (RR=0.11, 95%CI: 0.05 to 0.22,P<0.00001; Figure 5).Egger’s regression intercepts in needling were -0.06 (95%CI:-0.15 to 0.04,P>|t|=0.13), which indicated no publication bias.
Complete success rate Seven studies reported a complete success rate of surgery, which was obtained from 340 out of 391 (86.9%) eyes undergoing Phaco-NPGS and 312 out of 390 (80%) eyes undergoing NPGS-alone. Figure 6 showed no significant difference in the complete success rate between the two groups (WMD=1.18, 95%CI: 0.68 to 2.03,P=0.55). It should be noted that usually the success criteria varied among the previous studies, however, there is a good consistency among our included studies. Table 1 showed a detailed description of the success criteria of each study. Egger’s regression intercepts at 29.78 were obtained (95%CI: -22.30 to 81.87,P>|t|=0.20), which indicated no publication bias.
DISCUSSION
Glaucoma indicates that the associated economic and social burdens affect the lives of many people[28]. The efficacy of phaco combined with combined surgery for glaucoma patients remains controversial[15]. The single application of trabeculectomy is superior to combined phaco-trabeculectomy.This is because the combination adds inflammation which promotes failure of the filtering bleb and subconjunctival/episcleral scarring[29-30]. However, the efficacy and success rate of NPGS in reducing IOP do not appear to be affected when combined phaco and IOL implantation are performed[31-32].This study first reveals the efficacy in terms of IOP reduction between Phaco-NPGS and NPGS-alone, including subgroup analyses for all NPGSs without using different types of implants or antimetabolites as a combined therapy.
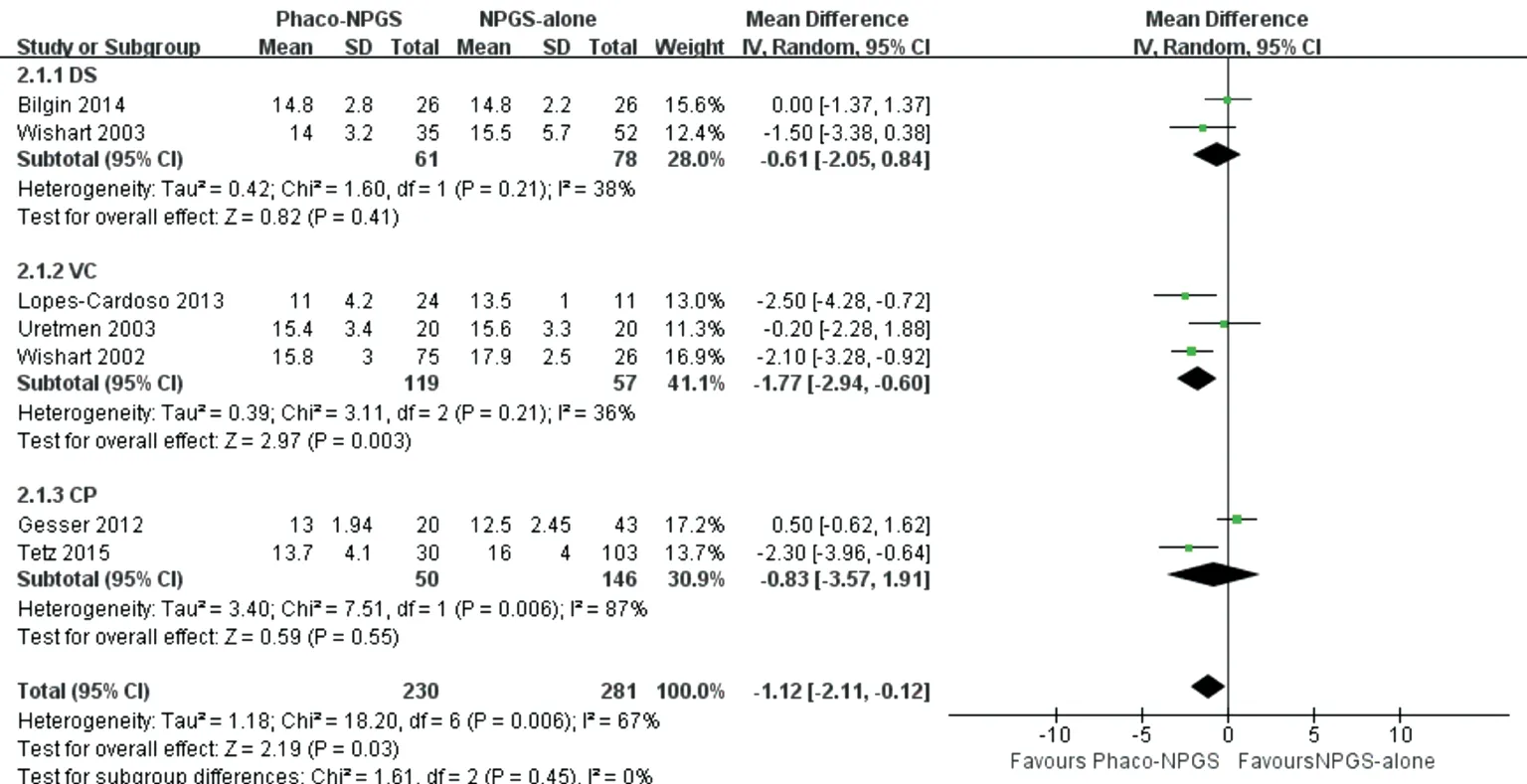
Figure 2 Comparison of the IOP control at latest follow-up in Phaco-NPGS group or NPDS-alone group.
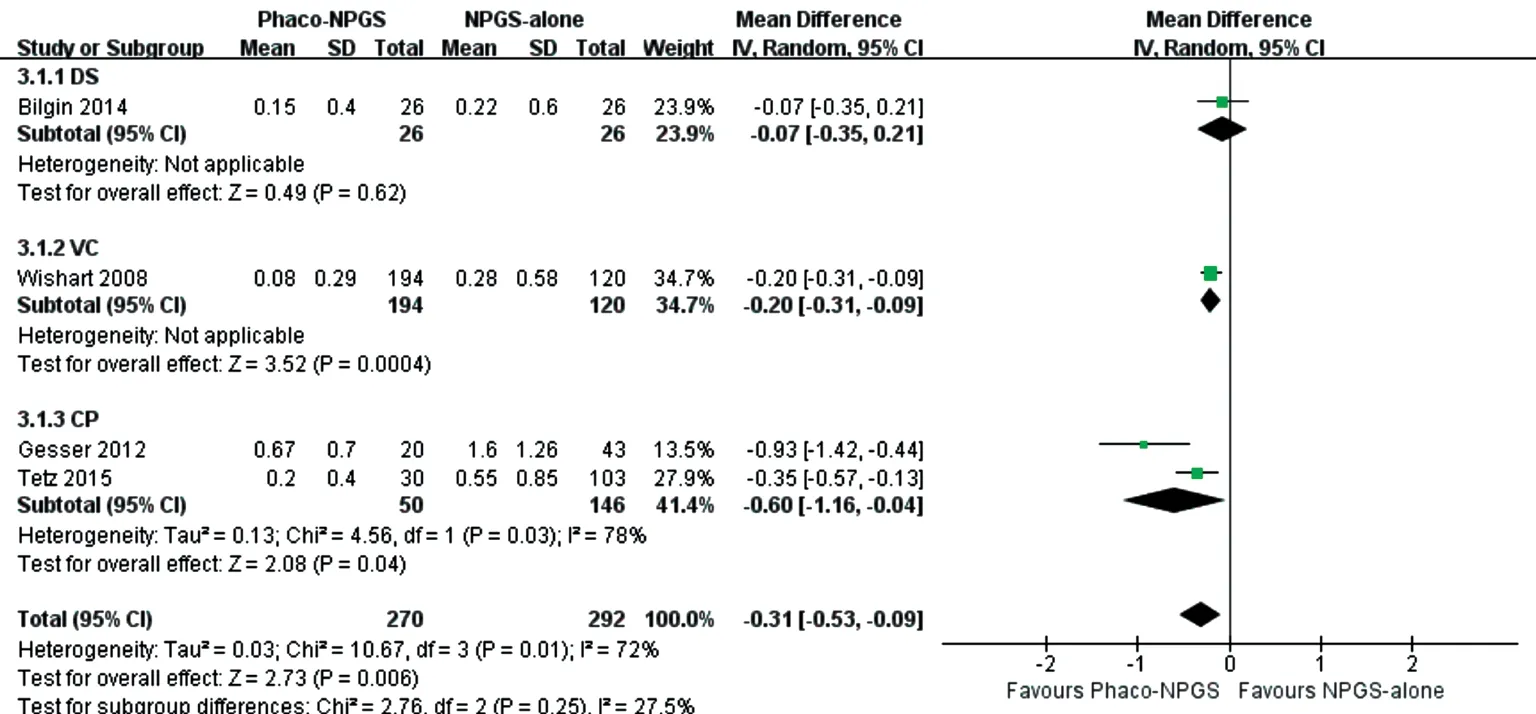
Figure 3 Comparison of the postoperative numbers of medications at latest follow-up in Phaco-NPGS group or NPDS-alone group.
D’Eliseoet al[33]reported that compared to sclerectomy alone,the success rate of DS combined with phaco (IOP≤20 mm Hg without medication) is higher (90% versus 62%). But another study reported that DS alone and PDS have no significant difference in success rates[12]. We noted that number of medications and postoperative IOP and were markedly lower in Phaco-NPGS consistent with the report by D’Eliseoet al[33],whereas the complete surgical success rate were similar. As previously reported, cataract removal might lower IOP and play a crucial role in the control of co-morbid glaucoma[14,34-35].There are growing evidences to support the fact that includes structural alterations accompanying the removal of the lens[35];production of endogenous prostaglandins and cytokines activated by intraoperative ultrasound, which enhances outflow facilityviaaffecting the lumen of Schlemm’s canal, and the trabecular meshwork[36]; cataract extraction which substantially affects ciliary body functions and postoperatively posterior displacement of the iris may alter the ciliary body shape[37]. Of note, the IOP-lowering effect may be beneficial in glaucoma.
These results indicate that for patients who require a persistent decrease in IOP and reduced postoperative IOP values, Phaco-NPGS might be a better choice for glaucoma patients with coexisting cataracts.
In particular, our Meta-analysis showed that VC has the best effect of lowering IOP among different kinds of NPGS. Of note, VC can improve the prognosis by restoring a natural aqueous outflow pathway independent of chronic inflammation[38]. Hence, VC can allow the aqueous-originating vasoactive activators of fibroblast to enter the Schlemm’s canal through TDW and exit the eyeviathe uveoscleral outflow or pre-existing collector channels and hence will not interact with fibroblasts in the subconjunctival space as for the scenario after trabeculectomy[34].
Another key factor in the incidence of surgical complications is the choice of which method to use to consider surgery.Regarding the prevalence of complications, NPGS-alone was more prone to complications than Phaco-NPGS with significant difference (5.6% versus 1.2%,P=0.01), in which hyphema was one of the most frequently reported complications. Five studies[20,23,27,33-34]reported hyphema in 7 out of 305 (2.3%)eyes undergoing Phaco-NPGS and 27 out of 321 (8.4%) eyes undergoing NPGS-alone. In addition, some authors considered that transient hyphema predicts better prognosis post-CP,showing that outflow pathways are open and function well[39].Among all common complications, only the prevalence of bleb fibrosis was statistically significantly higher in NPGS-alone(8.1%) than in Phaco-NPGS (0.43%). Compare to Phaco-NPGS, patients are prone to develop a relatively shallow anterior chamber after NPGS[40]. There is a theoretical risk of peripheral anterior synechiae development. Once the iris is in contact with the trabecular meshwork, it may cause physical or mechanical resistance to the outflow of aqueous humor. Since the eyes after Phaco-NPGS may get sufficient angle space and Schlemm’s canal opening compared to NPGS, NPGS is more prone to complications. As for the need for postoperative procedures, NPGS-alone is more prone to needling or goniopuncture than Phaco-NPGS with significant difference(22.0% versus 3.5%, P<0.00001), which is consistent with a higher incidence of complications in the NPGS group.
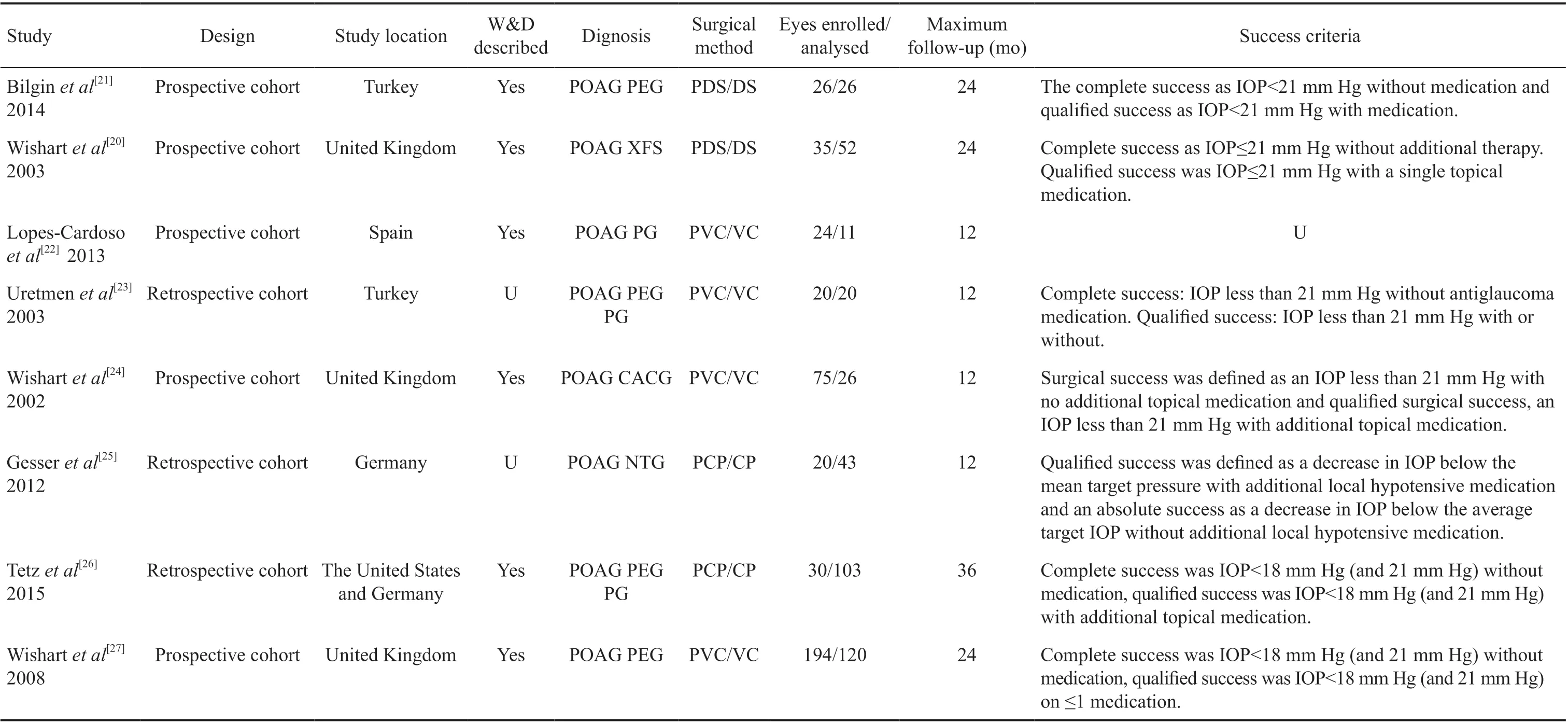
Table 1 Characteristics of included studies

Figure 4 Comparison of the risk of postoperative complications in the Phaco-NPGS group or NPDS-alone group.
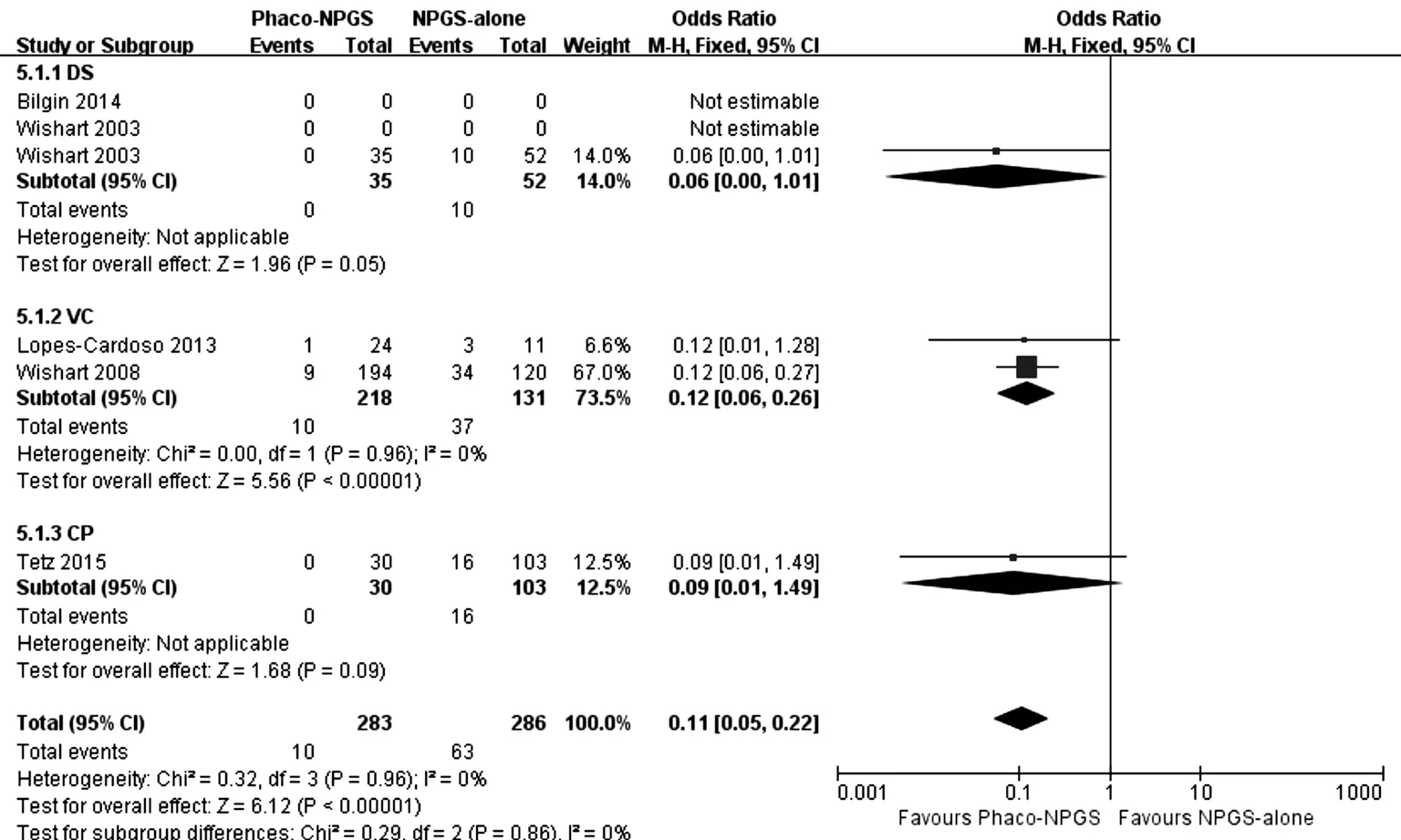
Figure 5 Comparison of the postoperative incidence of needling or goniopuncture in the Phaco-NPGS group or NPDS-alone group.
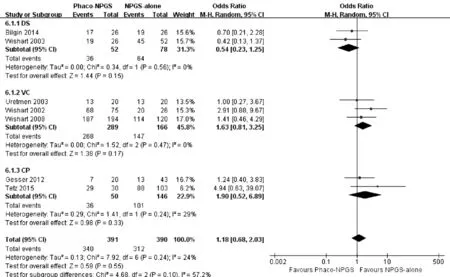
Figure 6 Comparison of the complete success after the Phaco-NPGS or NPDS-alone.
Previous studies included in the literature are applied in defining qualified or complete success criteria that vary widely,which makes comparisons between studies challenging.Previously, 92 successful definitions related to IOP were highlighted[41]. However, the criteria in our research for complete success were almost the same for all participants in each study, which allowed specific comparisons and we found similar complete success rates between the two operations. Of importance, we included different types of NPGS surgeries all without using implants or antimetabolites as a combination therapy, which is a great advantage over other Meta-analyses[42-43]. This study, thus, will be beneficial to ophthalmologists.
The key limitations to note are 1) inadequate data to allow the analysis of the impact of surgery on visual acuity preservation since only 2 studies reported postoperative visual acuity; 2)evidence is based on cohort non-randomized comparative studies; 3) The technique used to perform Phaco-NPGS and NPGS depends on the discretion of each center which was not completely the same; 4) despite subgroup analyzes based on surgery types, heterogeneity could not be reduced adequately;5) the final sample size was small in each comparison, hence reducing the power of some outcomes.In conclusion, a greater postoperative IOP and medication reduction, a more favorable safety profile were showed in Phaco-NPGS compared to NPGS-alone. Phaco-NPGS might be a better option for glaucoma patients with coexisting cataract who needs surgical intervention in IOP control.Further studies with prospective designed randomized trials, a longer follow-up period, and larger samples are warranted to verify our findings.
ACKNOWLEDGEMENTS
Authors’ contributions: Xiao JY contributed to the design,analysis of data and drafted the manuscript. Liang AY and Wang YL participated in the acquisition and analysis of data.Cheng GW and Zhang MF contributed to the conception and critically revised the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest:Xiao JY, None; Liang AY, None; Wang YL, None; Cheng GW, None; Zhang MF, None.
 International Journal of Ophthalmology2021年12期
International Journal of Ophthalmology2021年12期
- International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
