SARS-CoV-2 And The Gastrointestinal Disorders
SADIQUE HUSSAIN, CHANDAN MOHAPATRA, KESHAV TRIVEDI, LAKSHIKA GUPTA, HARSHIT BAWEJA
1School of Pharmaceutical Sciences, Jaipur National University, Jagatpura 302017, Jaipur, Rajasthan, India.
2School of Engineering and Technology, Jaipur National University, Jagatpura 302017, Jaipur, Rajasthan, India.
Abstract: Since the 1918 influenza pandemic, the severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) has produced the largest pandemic throughout the globe.SARS-CoV and the Middle East respiratory syndrome (MERS-CoV) are both members of the Beta CoV.The coronavirus disease of 2019 (COVID-19) has terrible implications and is currently a serious health concern throughout the world.SARS-CoV-2 affects the respiratory system first since it is the major site of entrance into the patient, but it can also damage other systems.Aside from the typical respiratory problems, several COVID-19 patients develop gastrointestinal (GI) symptoms such as weight loss, vomiting, nausea, and diarrhea.SARS-CoV-2 may infect the GI system via the angiotensinconverting enzyme 2 (ACE2) receptor, and indications of a fecal-oral transmission pathway are growing.Globally,GI disorders (GIDs) are becoming a major source of morbidity in youth.The condition has a significant financial impact on healthcare systems and hurts people's lives; nonetheless, very little is documented about the condition's worldwide prevalence and incidence.Alterations in gut sensitivity, motility, microbiota, immunological function,and central nervous system processing are all factors that contribute to GIDs.GI malfunction results in changes in changes in gut bacteria as well as an elevation in inflammatory cytokines.As a result, recognizing GI symptoms that precede COVID-19 respiratory issues may be crucial for better early identification and treatment.In GI epithelial cells of the intestinal mucosa, ACE2 and transmembrane protease serine-type 2 were also discovered to be substantially expressed.SARS-CoV-2 may also infect and multiply in both GI and liver cells in a dynamic manner.These findings suggest that SARS-CoV-2 might be a viable target for the GI tract.This review focuses on the GI complications that arise due to COVID-19 and how the CoVs give rise to GI symptoms.
Keywords: COVID, SARS-CoV-2, gastrointestinal diseases, ACE2, intestinal dysfunction
Introduction
Since the year 1000, when the pox virus swept throughout a large part of China, viral illnesses have remained a serious problem.The huge death toll from pox virus infection is sometimes attributed to the bubonic plague, which killed 75-200 million people across Europe between 1347 and 1351.Yellow fever,caused by Flavivirus, was described as the first humaninfected virus in 1901, and it was responsible for the deaths of almost 50 million people [1].A series of acute atypical respiratory diseases emerged in Wuhan, China,in December 2019, and spread to other regions of the globe.It wasn't long before it was determined that a new coronavirus was to blame.Due to its significant resemblance to SARS-CoV, the new coronavirus was first dubbed SARS-CoV-2 (2019-nCoV) and then renamed Coronavirus Disease-19 or COVID-19 [2].The S glycoprotein, the RNA-dependent polymerase,and two proteases; 3C-like protease (3CLpro), and papain-like protease (PLpro), are all shared by both the CoVs.ACE2, which is present in the human respiratory tract, is the entrance receptor for COVID-19, which is identical to SARS-CoV and has been demonstrated to induce pneumonia in lab mice solely expressing human ACE2 [3,4].The coronavirus family also includes numerous viruses which cause moderate to severe human disorders.After HKU1, OC43, NL63,229E, MERS-CoV, and the preceding SARS-CoV,SARS-CoV-2 is the seventh CoV to infect people [5].Coronaviruses (including 229E, OC43, NL63, and KHU1) are frequent in immunocompetent adults and children and cause a considerable percentage of all common colds [6].
Coughing and sneezing create respiratory droplets,which carry the virus quickly from one individual to the next.Although transmission may occur before symptoms appear in patients, it is believed to be most infectious when a person is sick.The time after exposure and development of symptoms is usually between 2-14 days, with a 5-day average.Cough,fever, sneezing, and shortness of breath are all common symptoms of CoV (Table 1) [7].Although serious lung damage has been reported in people of all ages, in some high-risk persons, the virus is more likely to experience serious interstitial pneumonia, acute respiratory distress syndrome (ARDS), and consequent organ failure., such as the elderly or those with multiple comorbidities,resulting in respiratory failure and high mortality rates [8].Cardiovascular illness (CVD), chronic renal disease, sickle cell disease, obesity, chronic lung diseases (especially COPD), hypertension, diabetes,and immunosuppression all predispose individuals to a poor clinical outcome and an increased chance of hospitalization and mortality [9].

Table 1 Clinical significance of COVID-19
SARS-CoV and MERS-CoV can both produce respiratory and GI symptoms, with GI symptoms accounting for more than 20% of cases.COVID-19 affects people of various ages, although research suggests that the average age of patients is 47 years old[10].Hypertension (14.9-35.2 percent), diabetes (7.4-16.7 percent), and CVD (2.5-14.5 percent) are the most frequent underlying illnesses among participants.The primary symptoms of COVID-19 patients were fever,cough, and weariness accompanied by GI problems,according to an analysis of their clinical features[11].The frequency of GI symptoms was as high as 79.1% among the 305 COVID-19 patients in Wuhan,according to research, while the incidence of diarrhea was 49.5 percent.Nausea and vomiting were reported in 29.4% and 15.9% of cases, respectively, whereas stomach discomfort was reported in just 6.0 percent of cases.The most prevalent GI symptom is diarrhea,and the incidence of diarrhea in COVID-19 patients in Wuhan was substantially greater than the national average.This might be attributed to the fact that Wuhan was the epicenter of the SARS-CoV-2 outbreak, and that owing to a lack of medical resources, emphasis was given to the care of severely ill patients [12,13].Table 2 shows the comparison of SARS-CoV, MERSCoV, and SARS-CoV-2.

Table 2 Comparison of SARS, MERS, and COVID-19 (14)

Table 3 Indications of gastrointestinal issues in COVID-19 patients
Gastrointesyinal Symptoms Of COVID-19 Patients
COVID-19 is a new virus that is causing a lot of concern because of its respiratory symptoms.Furthermore, diarrhea and other GI symptoms are common in COVID-19 individuals, although the relevance of these symptoms is unknown.Patients in Wuhan, China, provided the first evidence associating digestive disorders to COVID-19 [15].
The majority of patients of COVID-19 showed normal respiratory symptoms, according to 204 COVID-19 patients who presented at 3 hospitals.Many individuals infected with the CoVs, on the other hand, complained of stomach problems including diarrhea [16].
While most Covid-19 patients had a respiratory sickness, some have experienced GI symptoms as the disease progressed.The first instance of nCoV in the United States included a 35-year-old male who reported to the hospital with a 2-day history of nausea and vomiting, followed by diarrhea and stomach pain on the second day of hospitalization.On the seventh day,the SARS-CoV-2 RNA was discovered in the patient's feces using a reverse transcriptase-polymerase chain reaction.Similarly, diarrhea was recorded in two young adults (aged 36 and 37 years) out of six patients in a familial cluster of Covid-19 infections during the early pandemic, with reported bowel openings of up to eight times per day [17].Covid-19 patients have regularly experienced stomach issues in subsequent cohorts.In major research involving 1,099 patients from 552 hospitals in China, nausea or vomiting was observed in 5.0 percent and diarrhea in 3.8 percent of the patients[18].
2 major clinical investigations from China focused on gastrointestinal symptoms and viral identification in feces.Jin et al.looked at 74 SARS-CoV-2 patients who had GI symptoms such as diarrhea, nausea, and vomiting.Up to 28% of patients with GI symptoms had no respiratory sickness.They found that this patient group had generally more severe/critical illness, more patients with fever >38.5°C, familial clustering, and greater rates of liver damage as measured by increased aspartate transaminase levels when compared to individuals without GI symptoms (n=577).Overall,11.4 percent of SARS-CoV-2-infected individuals(n=651) exhibited GI symptoms, which is higher than previously reported rates.Lin et colleagues evaluated 95 SARS-CoV-2-infected individuals with a focus on GI symptoms in a separate investigation.Overall, 58/95 individuals (61.1%) showed signs of GI symptoms,with diarrhea (24.2%), nausea (17.9%), vomiting(4.2%), and decreased liver function as measured by increased transaminases (32.6%) being the most common [19].
It's worth mentioning that GI symptoms like diarrhea might emerge before fever and respiratory symptoms in certain circumstances.Two of the six patients in a family cluster experienced diarrhea as their first symptom and were brought to the hospital without a fever.Compared with patients without GI problems,patients with GI symptoms take a long time from COVID-19 onset to admission.As the epidemic progressed, the rate of diarrhea reported in hospitalized COVID-19 patients seemed to be increasing.The presence of diarrhea is correlated with the severity of COVID-19.Indeed, more critically ill patients have diarrhea [20].
SARS-CoV-2 can infect epithelial cells on the surface of the stomach, intestine, and colon, causing GI symptoms.COVID-GI symptoms demand significantly more care since there are greater opportunities for infection transfer owing to a lack of knowledge/information about GI consequences.Patients were predicted to have a moderate to high fever and raised liver function, and male patients (68.67 percent) had these tests far more frequently than female patients(38.36 percent) [27].
GI symptoms in COVID-19 patients have been linked to illness outcomes in several studies.Patients with GI symptoms had a lower death rate than those without any GI symptoms, according to Hajifathalian et al [28].Another research including 2,226COVID-19 patients in Spain came to similar findings [29].GI symptoms,on the other hand, have been linked to a poor prognosis in several studies.Individuals with GI symptoms had a greater incidence of severe or criticalCOVID-19 infection than patients without any GI symptoms,according to a meta-analysis [30].SARS-COV-2 CAUSES GASTROINTESTINAL DISORDERS IN HUMANS
SARS-CoV-2 spread quickly and has become a threat to public health all over the globe [31].On February 12, 2020, the World Health Organization(WHO) recognized the nCoV, describing it as a new pandemic disease [32].Coronavirus is a singlestranded RNA with a swath.The spike (S) protein,which is related to the ACE-2 receptor and arbitrates between the virus and host-cell membrane to facilitate viral entry into the host cells, is one of the four primary structural proteins concealed in the corona viral genome [8,33].The COVID-19 epidemic features high contagious levels and comparatively high death rates,especially among elderly people over 80 y of age [34].It is mostly a respiratory illness that also affects other organ systems such as the CVDs, GI system, kidneys,and brain system [35,36].COVID-19 is the seventh coronavirus to be found infecting humans.Before SARS-CoV-2, six other CoV strains were identified to infect humans (Table 4) [31,32].
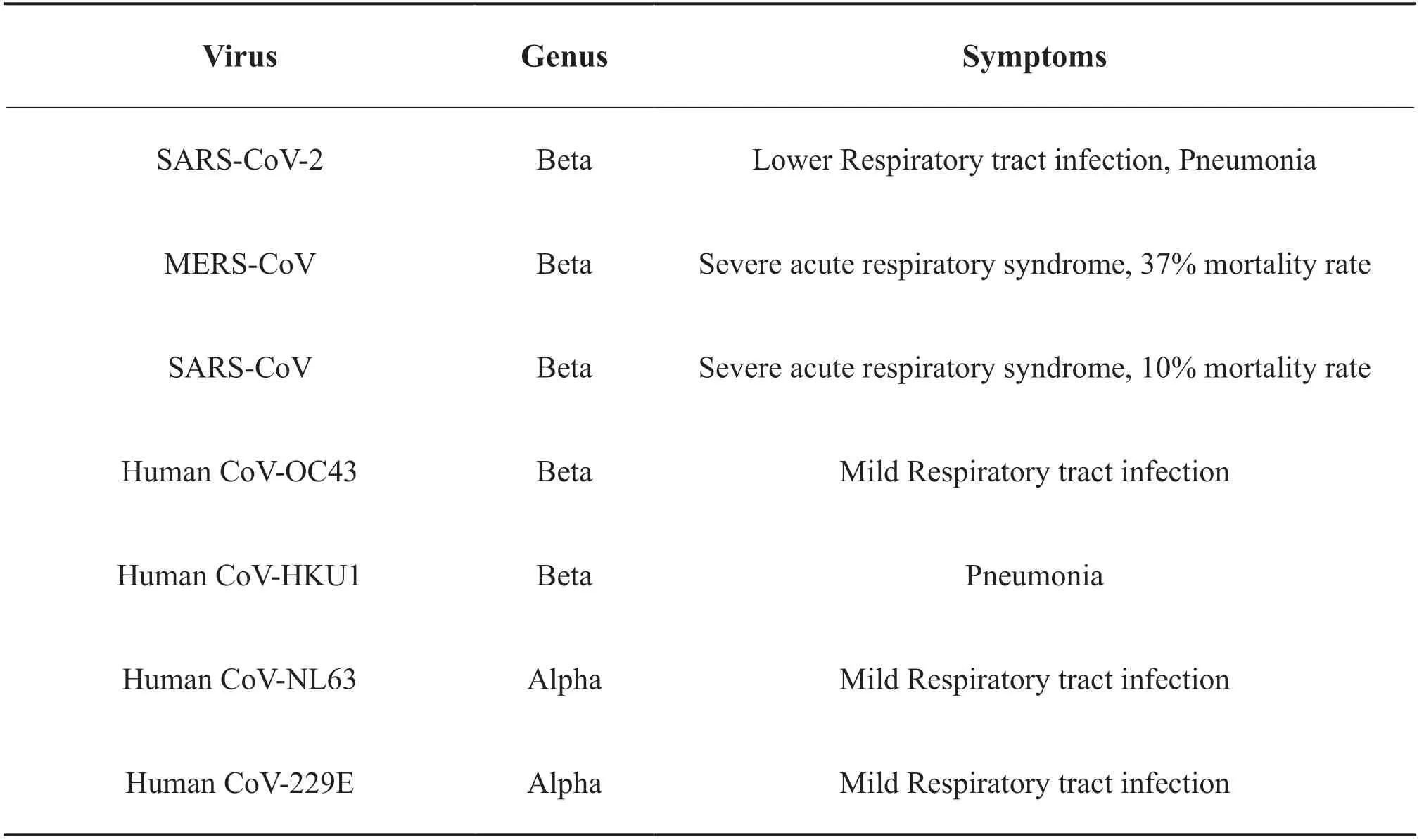
Table 4 List of human pathogenic coronavirus.
The epidemiology and clinical features of GI diseases in COVID-19 patients have been studied by several research organizations.SARS-CoV-2 has been found in feces in nearly half of COVID-19 cases, and its viral RNA has also been found in the intestinal mucosa,suggesting that the GI tract might be a possible route of infection.Because the SARS-CoV-2 receptor (ACE2)is recognized to be a major component of gastric mucosa and GI cells, the gastric mucosa or GIT may be regarded as a susceptible region for SARS-CoV-2 infection, according to research [39].Depending on the research, the percentage of patients having GI issues varies.Diarrhea (3.8-34%) is the most prevalent GI symptom in COVID-19 patients, followed by nausea and/or vomiting (3.9-10.1%), and stomach discomfort(1.1-2.2%).Anorexia, anosmia, and dysgeusia are further typical GI symptoms observed in COVID-19 patients.In a meta-analysis of 60 trials covering 4243 COVID-19 patients from six countries, Cheung et al discovered GI symptoms in 17.6% of the patients, with anorexia (26.8%), diarrhea (12.5%), nausea/vomiting(10.2%), and stomach pain/discomfort (9.2%) [40].Figure 1, Common Gastrointestinal manifestations of COVID-19.Borges and colleagues published the most recent and thorough meta-analysis to date,which included 59254 patients from 11 countries.The results of the meta-analysis revealed that GI symptoms were present in 9% of the participants.Previous investigations of SARS (2002-2003), also demonstrated concomitant GI signs, which are comparable to the present epidemic [41].
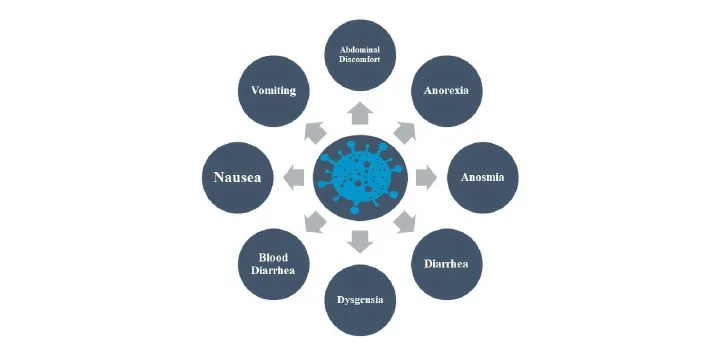
Figure 1 Common Gastrointestinal manifestations of COVID-19
Jin and colleagues in China enlisted 651 individuals before treatment with antiviral or antibiotic medicines,which might have skewed the results.Surprisingly, 11.4 percent of COVID-19 patients reported at least one GI symptom, with diarrhea being the most prevalent.The GI issues lasted a median of four days and appeared to come before the respiratory issues.GI symptoms were more common (23%) in severe/critical COVID-19 individuals than in moderate COVID-19 cases (8%).As shown by the vomiting, nausea, and diarrhea, they believe SARS-CoV-2 may induce acute gastritis and enteritis [42].In previous studies conducted in China and Hong Kong, the proportion of COVID-19 patients who acquired GID was 26%, 25.4%, 18.6%, 11%,13.7%, and 8.7%, respectively (n total = 254, 59, 204,58, 138, and 1099).In other trials, 55%, 35%, and 615 of COVID-19 patients in Europe and 278 and 318 in the United States, respectively, had GI signs and symptoms [43].
COVID-19 pathogenicity in regards to the GI tract has recently been examined elsewhere.To enter human host cells, an S protein component of the virus interacts with cell surface ACE-2 receptors.The nasal epithelium,as well as upper and lower respiratory tract epithelial cells, are rich in ACE-2 receptors.Furthermore, ACE-2 receptors are abundantly expressed throughout the epithelium of the human GI tract, notably in the terminal ileum and to a lesser extent in the colon.Finally, trypsinized are upregulated, which may aid in the solubilization of viral S protein and thus virus assimilation in human host cells.In contrast,investigations have shown that people with severe COVID-19 have a huge surge in the production of many cytokines, known as the cytokine storm [44,45].
Mechanisms Of Gastrointestinal Tract Involvement
Previous SARS research has shown that CoVs have a preference towards the GI system.SARS-CoV RNA was found in stool samples from SARS patients, and electron microscopy of biopsy and autopsy materials revealed active viral replication in both the small and large intestines [46].MERS-CoV might also cause enteric infection since human intestinal epithelial cells are very sensitive to the virus and can maintain vigorous viral replication [47].This GI tropism might explain why diarrhea is so common in CoV infections.This fecal source, especially when infective aerosols are created from the toilet plume, can contribute to fomite transmission [48].
ACE2 is a critical regulator of dietary amino acid balance, innate immunity, gut microbial ecology, and transmissible susceptibility to colitis in the intestines.It is predominantly localized on the luminal surface of differentiated small intestinal epithelial cells.These may have a role in the virus's invasion, the activation and amplification of gastrointestinal inflammation,and the development of GI symptoms in COVID-19 patients [49].The high expression ofACE2 in the intestinal tract makes the small bowel and colon highly susceptible to SARS-CoV-2 infection.Currently, a bioinformatic study based on single-cell transcriptomes to determine the location of ACE2-expressing cells in a COVID-19 patient has corroborated this idea.A recent study found that ACE2 expression was more common in the ileum and colon than in the lung and that it was primarily expressed in the ileum and colon's absorptive enterocytes, which might explain diarrhea seen in many COVID-19 patients.Furthermore, this study discovered that ACE2 is present in the stratified epithelial cells of the esophagus, which may contribute to explaining COVID-19-induced esophagitis.[50].
Potential Oral-fecal Transmission Of SARSCOV-2
Although the pathophysiology of SARS-CoV-2 infection-related digestive symptoms is unknown at this time, an increase in reports of viral RNA identification in stool samples and virus detection in the GI tract underscores the critical role of feces in SARS-CoV-2 virus transmission.SARS-CoV-2 RNA was found in the feces of around half of the COVID-19 patients, and viral nucleocapsid protein and RNA were also analyzed in GIT.SARS-CoV-2 RNA has also been found in the esophagus, stomach, duodenum, and rectum lately [51].More notably, SARS-CoV-2 RNA was found in most infected patients' self-collected saliva, and repeated saliva samples revealed a decrease in salivary viral load following hospitalization.All of these observations of viral RNA or proteins in the feces and GI tract suggested that SARS-CoV-2 might be transmitted from mouth to mouth [52,53].
Conclusion
The latest COVID-19 outbreak has wreaked havoc on human health on a scale never seen before.Because the causal agent of this COVID-19 pandemic infects the lungs as its major site of infection, initial research has mostly focused on its population dissemination and resulting pulmonary diseases.With a large number of research from diverse medical, biomedical, and related sectors, it is now clear that SARS-CoV-2 effects are not restricted to the lungs.The presence of systemic infection and clinical symptoms, including those in the GI tract, has been verified.Given the importance of the GI system in physiological maintenance, it is crucial to battle the anatomical damage caused by the SARS-CoV-2 infection.COVID-19 GI abnormalities cause problems that are difficult to control in patients with co-morbidities such as obesity, hyperglycemia,hypertensive disorders, liver illnesses, cardiovascular disorders, and so on.
 Medical Theory and Hypothesis2021年4期
Medical Theory and Hypothesis2021年4期
- Medical Theory and Hypothesis的其它文章
- Hypothesis on how Distance External Qi Therapy works
- Observation of the clinical effects of catgut implantation at acupoints on postpartum obesity with insulin resistance
- Study on the Mechanism of Shimian Granules (SMG) against Depression via Regulating Circadian Rhythms
- CiteSpace-based Knowledge Graph Analysis of the Current Status and Trends of Chinese Medicine Research in Idiopathic Membranous Nephropathy
