Maturation of robotic liver resection during the last decade: A systematic review and meta-analysis
Tomohiro Ishinuki, Shigenori Ota, Kohei Harada, Makoto Meguro, Masaki Kawamoto, Goro Kutomi, Hiroomi Tatsumi, Keisuke Harada, Koji Miyanishi, Ichiro Takemasa, Toshio Ohyanagi, Thomas T Hui, Toru Mizuguchi
Tomohiro Ishinuki, Toru Mizuguchi, Department of Nursing, Surgical Sciences, Sapporo Medical University, Sapporo 0608556, Hokkaido, Japan
Shigenori Ota, Ichiro Takemasa, Departments of Surgery, Surgical Science and Oncology,Sapporo Medical University, Sapporo 0608543, Hokkaido, Japan
Kohei Harada, Division of Radiology, Sapporo Medical University, Sapporo 060-8543,Hokkaido, Japan
Makoto Meguro, Departments of Surgery, Sapporo Satozuka Hospital, Sapporo 0048686, Japan
Masaki Kawamoto, Departments of Surgery, Nemuro City Hospital, Nemuro 0878686,Hokkaido, Japan
Hiroomi Tatsumi, Department of Intensive Care Medicine, Sapporo Medical University Hospital, Sapporo 0608543, Hokkaido, Japan
Koji Miyanishi, Department of Medical Oncology, Sapporo Medical University, Sapporo 0608543, Hokkaido, Japan
Toshio Ohyanagi, Department of Liberal Arts and Sciences, Center for Medical Education,Sapporo Medical University, Sapporo 0608556, Hokkaido, Japan
Thomas T Hui, Department of Surgery, Division of Pediatric Surgery, Stanford University School of Medicine, Stanford, CA 94598, United States
Abstract BACKGROUND Minimally invasive hepatectomy techniques have developed rapidly since 2000.Pure laparoscopic liver resection (LLR) has become the primary approach for managing liver tumors and procuring donor organs for liver transplantation.Robotic liver resection (RLR) has emerged during the last decade. The technical status of RLR seems to be improving.AIM To conduct a systematic review and meta-analysis comparing the short-term clinical outcomes of LLR and RLR over two 5-year periods.METHODS A systematic literature search was performed using PubMed and Medline,including the Cochrane Library. The following inclusion criteria were set for the meta-analysis: (1) Studies comparing LLR vs RLR; and (2) Studies that described clinical outcomes, such as the operative time, intraoperative bleeding, intraoperative conversion rate, and postoperative complications.RESULTS A total of 25 articles were included in this meta-analysis after 40 articles had been subjected to full-text evaluations. The studies were divided into early (n = 14) and recent (n = 11) groups. In the recent group, the operative time did not differ significantly between LLR and RLR (P = 0.70), whereas in the early group the operative time of LLR was significantly shorter than that of RLR (P < 0.001).CONCLUSION The initial disadvantages of RLR, such as its long operation time, have been overcome during the last 5 years. The other clinical outcomes of RLR are comparable to those of LLR. The cost and quality-of-life outcomes of RLR should be evaluated in future studies to promote its routine clinical use.
Key Words: Hepatectomy; Laparoscopy; Robot; Operation time
INTRODUCTION
Surgery is a curative treatment for liver tumors[1]. The development of surgical devices has promoted minimally invasive surgery (MIS), including minimally invasive liver resection[2]. Therefore, the concept of ‘big surgeons, big incision’ has become a myth[3]. Minimal skin wounds are preferable, and patients who undergo laparoscopic liver resection (LLR) recover faster without somatic pain than those that undergo open liver resection[1,4].
MIS has significant clinical benefits,e.g., it results in faster recovery, less pain, and shorter hospital stays[5]. On the other hand, long operation times and the associated higher costs were reported as disadvantages of the MIS approach[4,5]. However, the disadvantages of the MIS approach might be ameliorated as surgeons gain experience[6]. Initially, LLR was reported to have various clinical benefits but result in longer operation times[4].
Robotic surgery has gained popularity since 2000[7]. Although robotic towers occupy space in the operating room, the skill of surgeons can be enhanced by robotic technology, such as “wristed instruments”, “tremor cancellation”, “enhanced dexterity”, and “3D vision”[8,9]. These technologies are considered to reduce 93% of errors associated with human skill[8].
Total robotic liver resection (RLR) is limited to minor liver resection, which does not require the liver to be mobilized[10]. Furthermore, the robotic approach is only used for parenchymal dissection during laparoscopic surgery[11]. Therefore, the clinical outcomes of LLR and RLR should be similar[5,12]. We systematically reviewed the literature in which the clinical outcomes of LLR and RLR were compared. We divided the studies according to the year of publication to determine how the clinical outcomes of these techniques have changed over time. Early studies were defined as those published in 2016 or earlier. Recent studies were defined as those published in 2017 or later. We also examined the current status of RLR through a meta-analysis.
MATERIALS AND METHODS
Literature search
The Preferred Reporting Items for Systematic Reviews And Meta-Analyses (PRISMA)statement guidelines were followed when obtaining and reporting the meta-analysis data[13]. The PICOS scheme was employed when reporting the inclusion criteria. A systematic literature search of PubMed and MEDLINE, including the Cochrane Library, was performed independently by two authors (Ishinuki T and Ota S). The search was limited to human studies whose findings were reported in English. No restriction was set with regard to the type of publication, the publication date, or publication status. Patients of any age or sex who underwent liver resection for any hepatic lesion were considered, as outlined in the PICOS scheme. The search strategy was based on different combinations of words for each database. For the PubMed database the following combination was used: ("hepatectomy"[MeSH Terms] OR"hepatectomy"[All Fields] OR ("liver"[All Fields] AND "resection"[All Fields]) OR"liver resection"[All Fields]) AND ("laparoscopie"[All Fields] OR "laparoscopy"[MeSH Terms] OR "laparoscopy"[All Fields] OR "laparoscopies"[All Fields]) AND ("robot"[All Fields] OR "robot s"[All Fields] OR "robotically"[All Fields] OR "robotics"[MeSH Terms] OR "robotics"[All Fields] OR "robotic"[All Fields] OR "robotization"[All Fields]OR "robotized"[All Fields] OR "robots"[All Fields]). For the MEDLINE database,including the Cochrane Library database, the following combination was used: #1.liver.mp. [mp=title, abstract, full text, caption text], #2. resection.mp. [mp=title,abstract, full text, caption text], #3. robot.mp. [mp=title, abstract, full text, caption text],#4. 1 and 2 and 3.
Selecting policy of the studies
The independent authors have read the primary studies searched in the database.Similar studies and unrelated studies were excluded. The inclusion criteria for the statistical analysis were following: (1) Studies comparing LLR and RLR; (2) Studies reporting at least one clinical result or variable; and (3) If any institution reported multiple studies, only the recent and the excellent study was selected. The policies of the exclusion were following: (1) The studies dealing with liver transplantation; (2)Reviews, opinions, comments, letters, and case reports; and (3) The studies were impossible to reproduce. The Cohen kappa statistic was used to quantify assess the agreement among the researchers.
PROSPERO was used for the protocol registration (#CRD42021234405).
Data extraction
The independent authors extracted the following initial data: (1) The name of authors,year, and quality of study; (2) The etiology of the disease; and (3) The period of the evaluations.
Bias assessment
The publication bias was assessed by the Newcastle–Ottawa Scale: NOS (http://www.ohri.ca/), as they included observational studies. The NOS consists of domains for the patient selection, comparability of study groups, and outcomeassessment. The low risk of bias results in a score of 9 points. We considered studies that scored ≥ 7, 4-6, and < 4 to be high, moderate, and low quality, respectively[14].
Statistical analyses
RevMan software (version 5.3.; The Cochrane Collaboration) was used for the metaanalysis. For continuous variables, the differences between groups were compared using the inverse-variance method. On the other hand, dichotomous outcomes were compared using the Mantel-Haenszel method. The Egger’s test for publication bias was performed using EZR (version 1.54; https://www.softpedia.com/get/Science-CAD/EZR.shtml)[15].
Theχ2test was used to evaluate heterogeneity, and the CochranQandI2statistics were reported. TheI2value describes the percentage variation between studies in degrees of freedom. Low, moderate, and high heterogeneity were defined based on cut-off values of 25%, 50%, and 75%, respectively[16].
All results were considered significant atPvalues of < 0.05.
RESULTS
The PRISMA flow diagram for this study is shown in Figure 1. The database search for relevant studies resulted in 1,068 studies being identified. We excluded 922 studies because of duplication, and the titles and abstracts of the remaining 148 studies were screened. As a result, we reviewed 40 full-text articles to evaluate their eligibility further. We excluded 8 studies for which the outcome involved a non-target comparison, and 4 studies for which the data were not available. Finally, we included 28 studies in our meta-analysis.

Figure 1 PRISMA flow diagram for this study.
The data regarding the frequency of each type of liver resection in the selected studies are shown in Tables 1 and 2. Table 1 shows the data for the studies published in 2016 or earlier[9,12,17-30]. Table 2 shows the data for the studies published in 2017 or later[31-42]. No randomized controlled trials (RCT) comparing the clinical outcomes of LLR and RLR were identified. All of the selected publications related to observa-tional studies. The types of liver resection performed did not differ significantly between the early (Table 1) and recent (Table 2) studies.
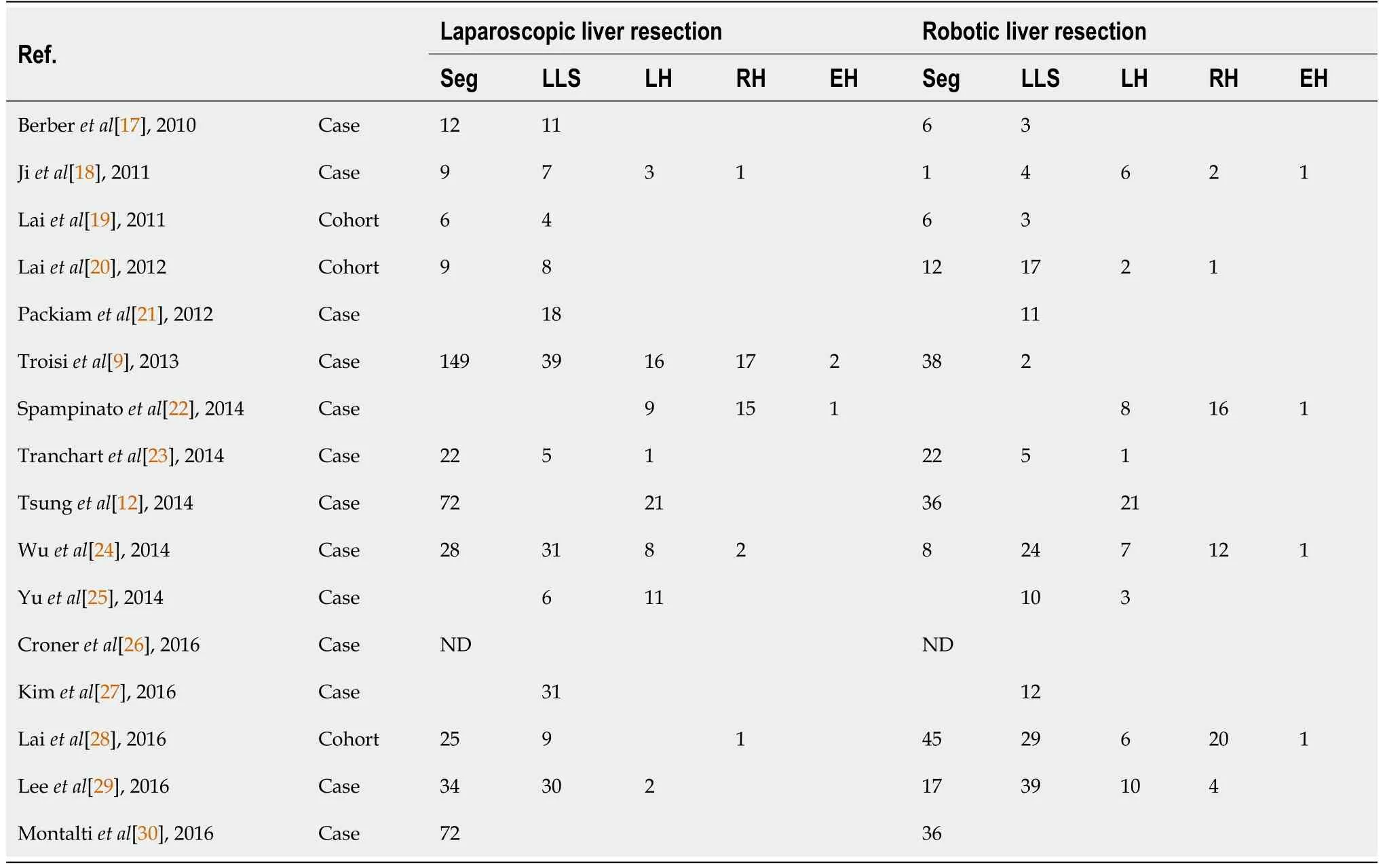
Table 1 Frequency of each type of liver resection in the studies published in 2016 or earlier
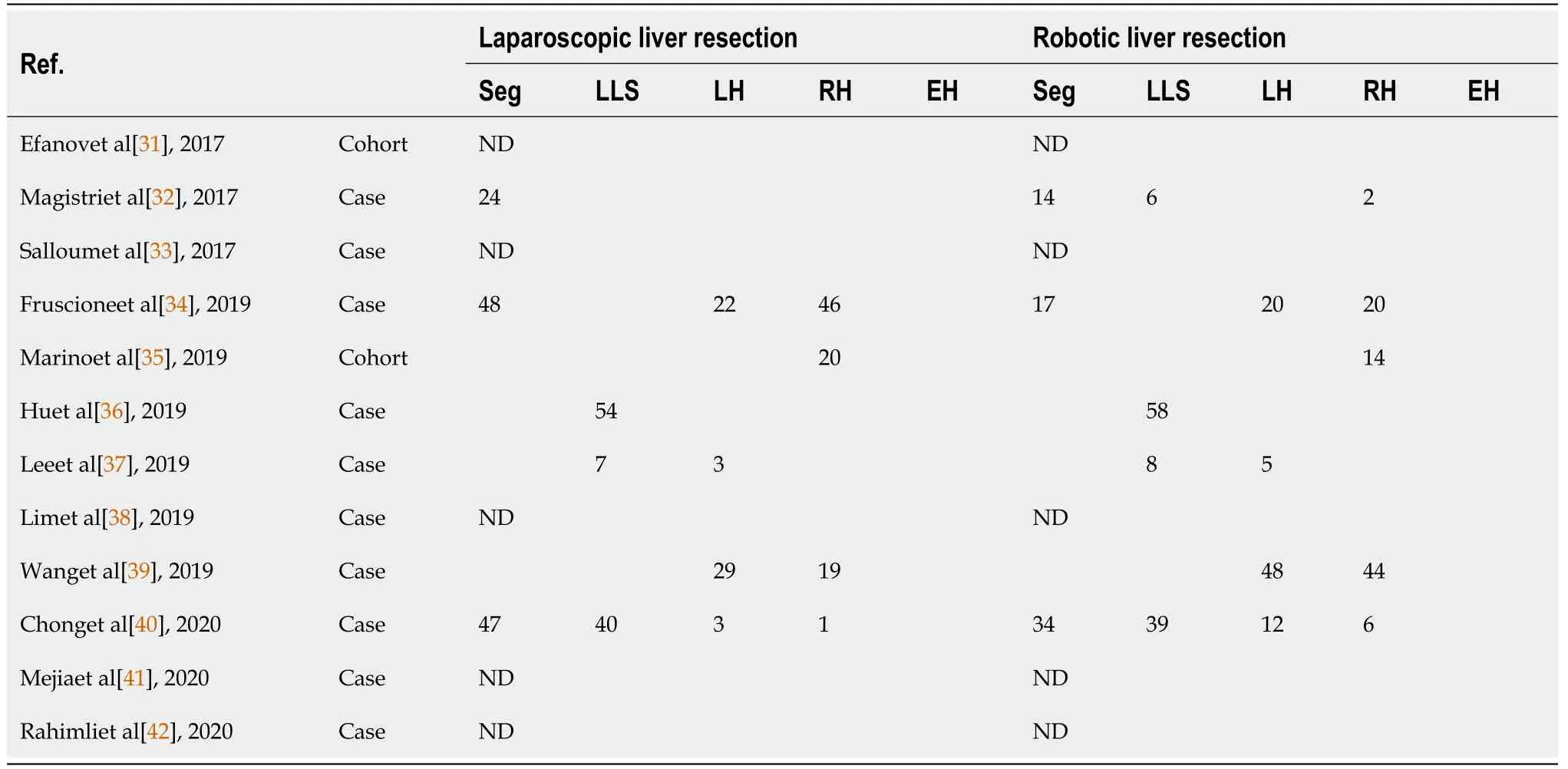
Table 2 Frequency of each type of liver resection in the studies published in 2017 or later
Frequency of Clavien-Dindo grade 3/4 complications
The data regarding complications of grade ≥ 3 according to the Clavien-Dindo (CD)classification are shown in Figure 2. There was no significant difference in the frequency of such complications between LLR and RLR in the early or recent studies.Scores ofI2in both analyses were 0%, which indicated no heterogeneity. The funnel plots were shown in Supplementary Fig ure 1.
Intraoperative conversion rate
The data regarding the intraoperative conversion rate are shown in Figure 3. There was no significant difference in the intraoperative conversion rate between LLR and RLR in the early or recent studies. Score ofI2in the early studies was 20% and the one in the recent studies was 44%. The heterogeneities were acceptable in the both analyses. The funnel plots were shown in Supplementary Figure 2.
Intraoperative blood loss
The data regarding intraoperative blood loss are shown in Figure 4. Although LLR tended to cause less intraoperative blood loss than RLR in the early studies, no marked difference in intraoperative blood loss between LLR and RLR was seen in the recent studies. Scores ofI2in the early and recent studies were 88% and 94%, respectively.Severe heterogeneities were observed in both the early and recent analyses. The funnel plots were shown in Supplementary Figure 3.
Operation time
The data regarding the operation time are shown in Figure 5. Although in the early studies the operation time of LLR was significantly shorter than that of RLR (P<0.0001), there was no significant difference between the operation times of LLR and RLR in the recent studies. Scores ofI2in the early and recent studies were 81% and 93%, respectively. Severe heterogeneities were observed in both the early and recent analyses. The funnel plots were shown in Supplementary Figure 4.
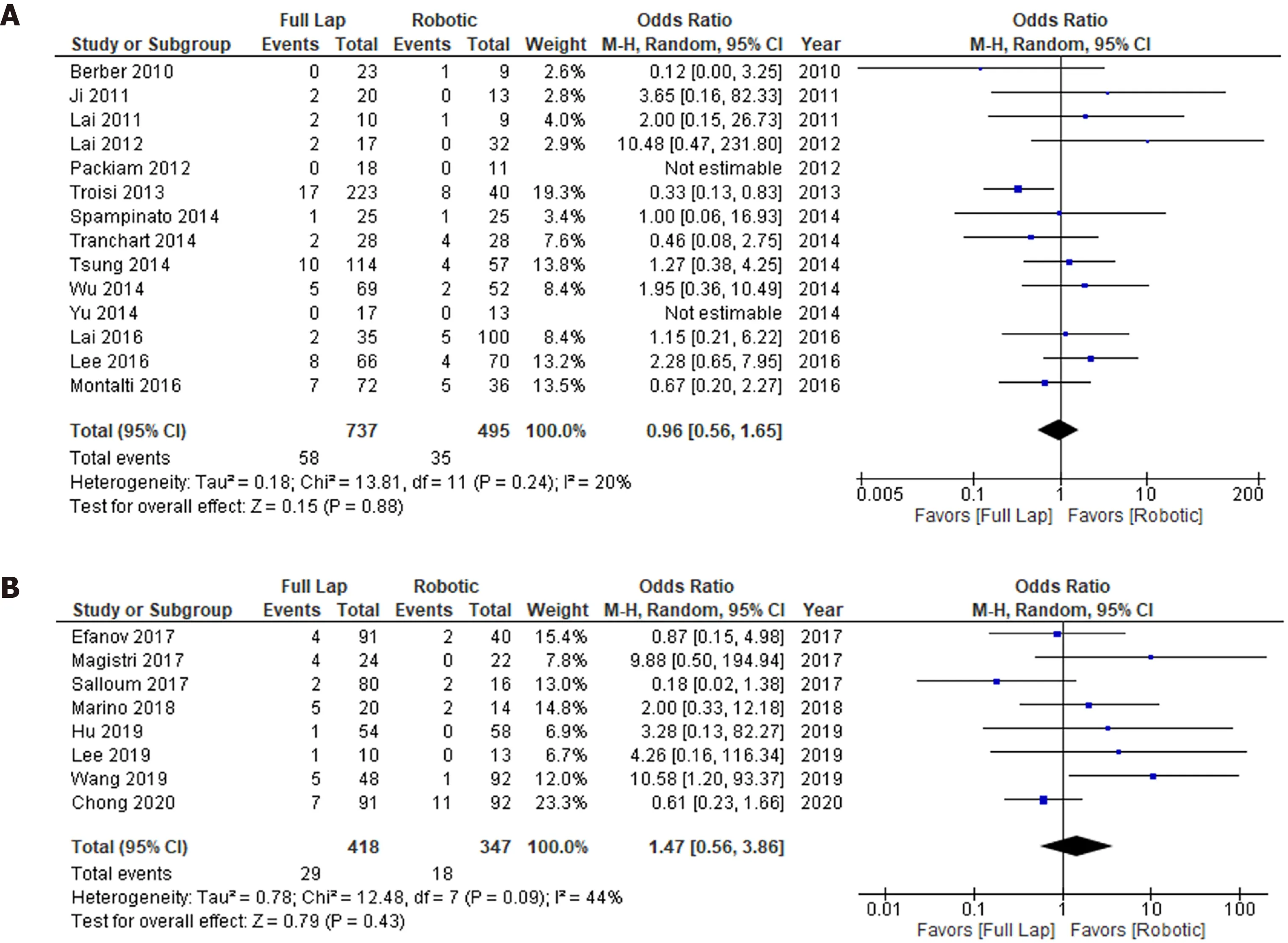
Figure 3 Intraoperative conversion rate. A: 2010-2016; B: 2017-2020.

Figure 4 Intraoperative blood loss. A: 2010-2016; B: 2017-2020.
Quality assessment of the bias
The quality assessment was conducted using the NOS score (Supplementary Table 1 and 2). There was no significant difference in the NOS score between the early and recent studies, although the quality of the studies varied. Summary of the publication bias in each analysis was shown in Supplementary Table 3.
DISCUSSION
MIS has become the standard approach for liver resection[1,4]. The initial disadvantages of RLR were that it involves large amounts of intraoperative blood loss and a long operation time. The recent studies examined in this review indicated that these initial disadvantages have been ameliorated. This finding strongly indicates that a new era of MIS may be upon us.
The CD classification is the standard grading system for surgical complications[43].The definitions of the grades in the CD classification are based on how the complications are managed,e.g., with pharmacological interventions, surgical interventions, or intensive care. These are indirect signs of complications. Furthermore, the grading system is divided into 5 grades plus 2 sub-grades. We did not find any difference in the types of complications encountered according to the CD classification between LLR/RLR or the early/recent period. This may have been because the CD classification is not suitable for identifying differences between clinical studies due to its use of indirect definitions and a relatively large number of grades. Ideally, surgical complications should be analyzed based on direct symptoms of the actual complications and a simple grading system[44].
LLR and RLR exhibited similar intraoperative conversion rates in both periods. The background data for each study varied, as they were all observational studies. The selection criteria for LLR and RLR were also unclear. Therefore, we could not conclude which type of surgery was safer. The maximum intraoperative conversion rate of LLR was about 25% among the recent studies. The maximum intraoperative conversion rate of RLR was about 20% among the early studies, although the mean conversion rate was < 10% in both study periods. In future, these rates could be used as standard clinical goals in order to ensure that surgical quality is maintained.
In the early studies, LLR tended to result in less intraoperative blood loss than RLR,although no marked differences in intraoperative blood loss were seen between LLR and RLR in the recent studies. Several strategies can reduce blood loss during pneumoperitoneum, such as using the head-up position, inducing a high peritoneal pressure, reducing the intratracheal pressure to increase the respiration time, reducing the respiratory volume, using a low central venous pressure, and employing inflow blood control based on the Pringle maneuver[2,45,46]. In addition, it is easier to change the body positions of patients during LLR than during RLR, which could help to control bleeding from veins. Various hemostatic devices are available, such as ultrasonic dissectors, and various hemostatic surgical devices were used for RLR in the recent studies, which may have counteracted the positional disadvantages of RLR. In addition to technical improvements associated with experience, various surgical devices can be used to reduce blood loss during RLR.
In the early studies, the operation time of the RLR was longer than that of the LLR.This is reasonable because it takes time to install robotic towers for robotic procedures.However, the difference in the operation time between the surgical procedures disappeared in the recent studies. It could be that the surgeons became familiar with the robotic procedures, which reduced the time required to set up the robot. Visual support and human-error-canceling functions could also have reduced the operation time[8]. Therefore, the initial disadvantages of RLR have recently been ameliorated.
One advantage of RLR is that it can be used to approach the dorsal segment and caudate lobe of the liver[47,48]. In addition, RLR is superior to LLR for bile duct reconstruction[49]. Therefore, separate tumor location- and surgical proceduredependent indications need to be developed for RLR and LLR. The differences in the cost and quality-of-life outcomes of RLR and LLR should also be elucidated in the future.
This study had several limitations. First, all of the included studies were observational studies, and no RCT were identified. In addition, the indications for each procedure were not described clearly. The number of subjects recruited for each study varied, as did the quality of each study. In addition, the clinical backgrounds of the studies differed. Although a few studies involved prospective protocols, at present there is no international registration system for such studies.
CONCLUSION
In conclusion, the initial disadvantages of RLR have been ameliorated. The clinical outcomes of LLR and RLR are comparable. Separate indications for each approach should be developed based on their cost and quality-of-life outcomes. A reliable international registration system for such cases needs to be established.
ARTICLE HIGHLIGHTS
Research background
Robotic liver resection (RLR) has emerged during the last decade. But the clinical outcome of the RLR has been debated.
Research motivation
Clinical outcomes among the laparoscopic liver resection (LLR) and RLR should be compared regarding merit and demerit.
Research objectives
The objective of this study was to conduct a systematic review and meta-analysis comparing the clinical outcomes of LLR and RLR over two 5-year periods.
Research methods
A systematic literature search was performed using PubMed and Medline, including the Cochrane Library.
Research results
A total of 25 articles were included in this meta-analysis after 40 articles had been subjected to full-text evaluations.
Research conclusions
The initial disadvantages of RLR, such as its long operation time, have been overcome during the last 5 years. The other clinical outcomes of RLR are comparable to those of LLR.
Research perspectives
The cost and quality-of-life outcomes of RLR should be evaluated in future studies to promote its routine clinical use.
 World Journal of Meta-Analysis2021年5期
World Journal of Meta-Analysis2021年5期
- World Journal of Meta-Analysis的其它文章
- Current and future of anterior cruciate ligament reconstruction techniques
- Weight regain after bariatric surgery: Promoters and potential predictors
- Review of the effects of SARS-CoV2 infection and COVID-19 on common pediatric psychiatric illnesses
- COVID-19 and psychiatry training: A cross-national trainee perspective
