Risk of methicillin-resistant staphylococcus aureus prosthetic joint infection in elective total hip and knee arthroplasty following eradication therapy
Benjamin Pal Kapur, Xenia Tonge, Gunasekaran Kumar
Benjamin Pal Kapur, Xenia Tonge, Gunasekaran Kumar, Trauma and Orthopaedics, Royal Liverpool University Teaching Hospitals, Liverpool L7 8XP, Merseyside, United Kingdom
Abstract BACKGROUND Prosthetic joint infection (PJI) is a devastating complication requiring prolonged treatment and multiple operations, leading to significant morbidity for the patient. Patients are routinely tested for methicillin-resistant staphylococcus aureus (MRSA) colonisation. MRSA positive patients are given eradication therapy. We hypothesise that patients who are MRSA positive pre-operatively, have increased risk of developing PJI.AIM To identify deep wound infection (PJI) rates in patients who are colonised MRSA positive compared with those who are not colonised; and long term clinical and radiological outcomes.METHODS All patients who underwent total hip and knee replacements (THR/TKR) between December 2009 and December 2019 were identified. Patients who were also identified as being MRSA positive at pre-operative assessment were then selected. Confirmation of prescribing eradication treatment was recorded. Patient records, including consultation letters, operation notes and microbiology results were reviewed retrospectively. Comparison of outcomes for each MRSA positive patient was made with 2 MRSA negative patients undergoing the same operation of a similar age by the same consultant.RESULTS Screening identified 42 knee and 32 hip arthroplasty patients as MRSA positive, 84 MRSA negative knee and 64 hip patients were reviewed. Patients were matched with medical co-morbidities in each group. Mean follow up was 5 years. PJI was identified in 4/32 (12.5%) of THR MRSA positive and 3/42 (7%) of TKR patients. All patients had PJI within one year of surgery.CONCLUSION MRSA positive patients are given eradication therapy routinely. However, no confirmation of eradication is sought. Patients who have MRSA colonisation preoperatively, in our study had a significantly increased risk of PJI, when compared to negative patients. We would recommend establishing true eradication after treatment prior to arthroplasty.
Key Words: Hip; Knee; Prosthetic joint infection
INTRODUCTION
Total joint arthroplasty (TJA) of the hip and knee are the two most commonly performed orthopaedic procedures. Due to an aging population, the numbers of patients undergoing TJA is increasing yearly as shown in the National Joint Registry reports[1]. Prosthetic joint infection (PJI) after TJA is reported in 1%-2% of patients[2]. Revision arthroplasty has significantly higher complication rates with infection rates reported over 20%. PJI has increased morbidity and mortality for patients and increased associated healthcare costs due to treatment, length of stay and readmission[2]. PJI was defined by adaptation of the Musculoskeletal Infection Society criteria a described by Parvizi[3] Major and minor criteria were used[3]. In our institution inflammatory markers are taken (C-reactive protein and erythrocyte sedimentation rate) and aspiration of the joint are routinely performed and observation for a sinus tract. We do not perform synovial tests or alpha-defensin.
Depending on microbial virulence, PJI can manifest either early (within the first few weeks after implantation) or with a delay (typically within 3 mo and 3 years). Early infections manifest with clear local and systemic signs of inflammation and are predominately high virulence organisms (Staphylococcus aureus, enterococcus and streptococcus). Delayed infections usually present insidiously with symptoms to suggest failing implants such as joint pain and loosening. Low virulence organisms often responsible such as coagulase negative staphylococci or cutibacterium species[4].
All prosthetic joints remain susceptible to haematogenous seeding from a distant primary focus during their entire indwelling time[2]. High vascularity of periprosthetic tissue exposes the prosthesis to the highest risk of haematogenous infection in the first years after implantation. Patients often present with acute onset of clinical symptoms after a painless post-operative period[5]. The risk after bacteraemia with S. aureus is reported up to 34%[6]. The most commonly isolated organism in PJI after TJA is staphylococcus aureus. Present in the anterior nares, 25%-30% of the population are colonized at any given time. Carriers are at higher risk for surgical site infection (SSI) after invasive medical or surgical procedures. It has been demonstrated in the literature that carriers are 2 to 9 times higher to have a SSI[7]. Strains of methicillinresistant staphylococcus aureus (MRSA) are much lower, 1% of the population with a higher preponderance for the elderly, immune-compromised or those with multiple co-morbidities. It has been shown that 85% of SSIs can be traced to endogenous colonisation of the patient[7].
The centers of disease control recognised nasal colonisation as a risk factor for SSI[8]. As a result there has been a focus on pre-operative screening and decolonisation prior to the patient undergoing surgery. Most strategies to decrease the incidence of SSIs have focused on timely antibiotic administration, optimising patients comorbidities and nutrition, minimising surgical wound contamination in the operating theatre by using isolation suits and reduced personnel in the theatre suite.
The purpose of this study are to (1) Identify deep wound infection (PJI) rates in patients who are colonised MRSA positive compared with those who are not colonised; and (2) Long term clinical and radiological outcomes.
Ethical approval was not required for this study.
MATERIALS AND METHODS
This study is a retrospective analysis of elective primary total hip and total knee arthroplasty procedures done at our institution from December 2009 to December 2019. Patients were identified from a prospectively collected database and crossreferenced with the hospital database using procedural codes. The policy at our institution is to screen for MRSA using (culture) swabs in surgical pre-operative assessment when the patient is listed for elective surgery. Those patients identified as colonised with MRSA are contacted and instructed to undergo self-administered standard protocol decolonisation eradication therapy. This consists of prontoderm® nasal spray (Braun) and octenisanantimicrobial wash (Schulke) to be used 5 d prior to and finishing on the morning of surgery. The patients are not retested following treatment.
The microbiology data of all these patients was reviewed, which confirmed the preoperatively diagnosed MRSA colonised patients. Detailed review of the medical records of these patients was undertaken to determine risk factors, eradication prophylaxis and perioperative antibiotics and outcomes.
Indication for surgery, operating consultant, co-morbities, age and complications including infection and revision were recorded for all patients. A control group was generated using patients undergoing the same elective arthroplasty procedure by the same consultant, within a 6 mo time period. Patients were matched on a 2 to 1 basis of MRSA negative to positive by comparable age (within 5 years) and same comorbidities to make the groups representative of each other rather than using all the arthroplasty patients. To reduce selection bias, patients in the non-MRSA cohort were selected by operative date closest to the operative date of the MRSA positive patient, surgeon and co-morbidities selected.
Antibiotic prophylaxis for primary arthroplasty patients is teicoplanin 1.2 g intravenous on induction if the patient had tested positive for MRSA colonisation. Standard protocol is a stat dose of cefuroxime 1.5 g intravenous on induction and no further antibiotics.
At pre-operative assessment patients have a health screen, observation parameters are taken and blood tests are performed to identify any abnormalities that require addressing prior to surgery and an electrocardiogram is performed. Patients provide a urine sample for analysis at pre-operative assessment and are treated if required.
Patient outcomes are recorded for SSI, organisms, complications, revision procedures undertaken and eventual outcome.
RESULTS
Between January 2009 and December 2019, 3166 total knee arthroplasty and 2738 hip athroplasty procedures were performed.
For the purpose of this study, we used matched analysis with a ratio of 2 MRSA negative patients to 1 colonised MRSA positive patient.
The total number of MRSA negative patients was 3124 total knee replacements (TKRs) and 2706 total hip replacements (THRs). Combining positive MRSA colonised and negative patients, MRSA colonisation was observed in 74 patients (32 hip, 42 knee) with a colonisation rate of 1.25%.
All 74 patients were issued with decolonisation treatment to be utilised for the 5 d prior to surgery; however, no patients were retested prior to their surgery.
There were 42 MRSA colonised positive TKR patients matched based on surgeon, age, co-morbidities with 84 MRSA negative patients. The average age was 69.3 years (range 54-83). The average follow up was 4.78 years (range 1-10). Table 1 outlines thedemographics of this group.
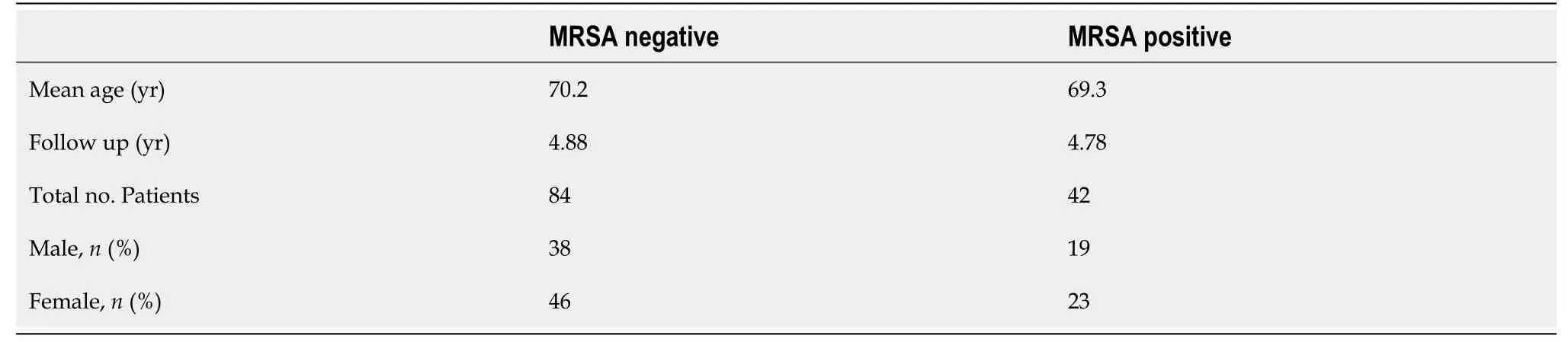
Table 1 Total knee replacement–demographics
Our cohort of colonised patients self-administered their decolonisation therapy and all lived at home. In the MRSA colonised positive TKR group, 7 patients were diabetic, 21 patients had pre-existing cardiac disease and were on anticoagulation, 12 patients had chronic respiratory conditions, 10 has inflammatory conditions (on steroids/ methotrexate) and 2 patients had a malignancy.
Of 3 out of 42 TKR patients developed MRSA PJI requiring revision surgery within 1 year of their index procedure, giving an incidence of 7%. 2 out of 3 patients underwent two-stage revision and 1 patient underwent debridement, antibiotics and implant retention (DAIR). Mean follow up from revision surgery is 4 years and all patients are clinically and radiologically infection free. Patient one was diabetic and had renal disease, patient two was diabetic and had respiratory disease and malignancy and patient three was on steroid for inflammatory disease and had preexisting ischaemic heart disease and used anticoagulation.
The MRSA negative TKR control group, which consisted of 84 patients, matched by surgeon and comorbidities as described above had an average age of 70.2 years (range 50-82). Follow up average 4.8 years (range 1-10). Of the 84 patients there was 1 patient with diagnosed with an e. coli PJI requiring a DAIR. This patient had chronic kidney disease. The patient is clinically and radiologically infection free at 6 years. The incidence of PJI was 1.2%.
There were 32 MRSA positive THR patients matched based on surgeon, age, comorbidities with 64 MRSA negative patients. The average age was 67.6 (range 54-94). The average follow up was 5.1 years (range 1-10 years). Table 2 outlines the demographics of this group.
In the MRSA positive THR group, 4 patients were diabetic, 12 had cardiac conditions and were on anticoagulation, 7 had chronic respiratory conditions, 2 had inflammatory conditions (on steroids/methotrexate) and 4 had malignancy.
Out of the 32 patients, 4 developed MRSA PJI requiring revision surgery within 1 year of their index procedure giving an incidence of 12.5%. Three patients underwent two-stage revision and 1 underwent single stage with prolonged antibiotics. Patient one had diabetes and was on steroid, patient two had chronic kidney disease and ischemic heart disease and used anticoagulation, patient three had malignancy and was on steroid and patient four was diabetic with chronic renal disease and respiratory disease. Mean follow up from revision surgery is 5 years and all patients are infection free clinically and radiologically.
The MRSA negative THR control group, which consisted of 64 patients, matched by surgeon and co-morbidities as described above had an average age of 67.8 years (range 50-94). Follow up average 6 years (range 1-10 years). Of the 64 patients, there have been no incidences of PJI during this follow up period.
The results of the incidence of PJI are summarised in Table 3.
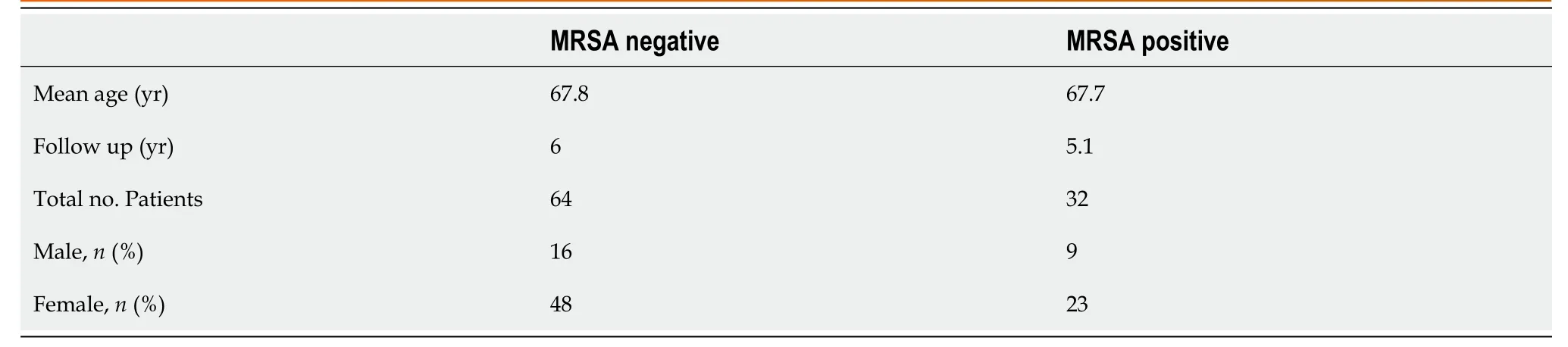
Table 2 Total hip replacement-demographics
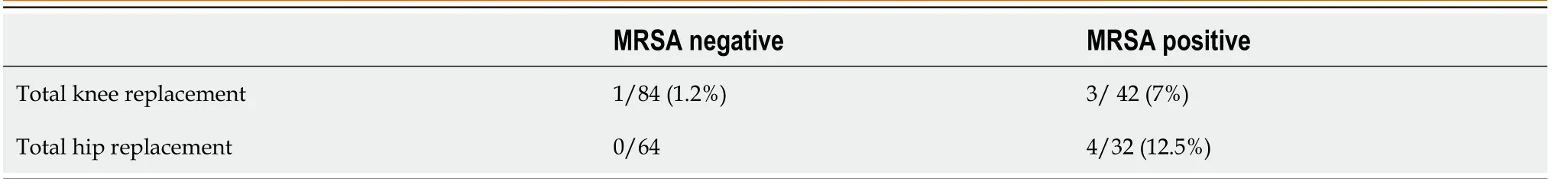
Table 3 The results of the incidence of prosthetic joint infection
All PJI s were methicillin resistant, there were no methicillin sensitive staphylococcus organisms.
DISCUSSION
This study demonstrates a higher incidence of methicillin resistant staphylococcus aureus infection in patients who have been previously colonised in elective hip and knee arthroplasty. The results of this study show that at our institution there is a 1.25% MRSA colonisation rate in patients undergoing total hip and knee arthroplasty. This iscomparable with studies in the literature demonstrating rates by Tandon[8] of 1.3%.
PJI after THR and TKR are associated with substantial patient morbidity and economic burden to the healthcare system. Many approaches and resources have focused on infection reduction methods. A targeted strategy is to identify patients who are MRSA positive and attempt to decolonise them, as MRSA is a risk factor for PJI. There are limited data on the success of decolonisation protocols and their subsequent effect on PJI. A 69% reduction in the prevalence of PJI has been demonstrated with screening and eradication[9,10].
Kim[11] include the single largest cohort of orthopaedic patients[11]. They found a decrease in surgical site and PJI in their treatment group with compared with historical controls and MRSA negative patients.
Literature has shown mixed results on the role of decolonisation of MRSA carriers and is effect on carrier rates and PJI in elective orthopaedic surgery. This in part depends on whether patients comply with treatment.
Shukla[12] identified 2.5 times higher risk than the normal population of developing postoperative MRSA SSI and PJI in carriers in an orthopaedic trauma unit[12].
In a prospective observational study of elective hip and knee replacements, One study showed no postoperative cases of staphylococcus aureus SSI at 1 year follow up in the group who had screening and successful decolonisation treatment. 3.5% infection rate was noted in the concurrent control group[12]. This is in keeping with the results we obtained suggesting retesting and further eradication treatment contributes towards the prevention of PJI.
A weakness of this study is that it is a retrospective analysis. A weakness of our protocol is that patients are issued the treatment and it is used up to and finishing on the day of surgery however, there is no assurance that the patients comply. There is no re-test to ensure eradication of MRSA and no opportunity for further eradication treatment if the patient is still positive.
Kim[11] have shown that there is 22% treatment failure rate with MRSA decolonisation nasal and soap treatment. They hypothesise that the factors associated with treatment failure are non-compliance and the presence of resistant organisms. This supports the need for screening post treatment to ensure eradication and address any modifiable risk factors for PJI. This also has an impact on consent and quantifying risk for patients.
The balance is in favour of screening, eradication therapy and re-screening to reduce the risk of PJI, which is a costly complication following elective surgery. The financial implications of treating MRSA PJI are immense. Current revision practice is changing in the United Kingdom[13]. Pathways for centralisation and regionalisation of revision services are being created. Nathwani[14] studied the impact on separate elements –hospital, patient and society[14]. Bozic and Ries[15] showed that costs associated with revision arthroplasty due to infection are 2.8 times higher than aseptic revision and 4.8 times higher than primary arthroplasty[15]. Revisions due to infection were associated with 3 times the number of repeat hospitalisations and outpatient visits and nearly 4 times the number of operations with approximately 22 d in hospital when compared with aseptic revisions. Given the current protocol–12.5% of THR and 7% of TKRs becomes infected with MRSA, which generates complications and carries with it the financial implications.
Screening for MRSA is inexpensive (500 rupees for a screening test). Although this study did not investigate the cost analysis of MRSA PJI, VandenBergh[16] determined the cost-effectiveness of perioperative mupirocin (Bactroban; GlaxoSmithKline, Middlesex, United Kingdom) in cardiothoracic surgery[16]. They suggested that due to the immense cost of a PJI, an effective intervention with a relatively cheap agent like mupirocin is likely to be cost-effective as a risk reduction of 1% would be cost-effective already. Also the side effect profile of mupirocin is negligible. This has to be balanced with the risk of recurrence and resistance to standard treatment, which is a recognised complication[16,17]. Young and Winston[18] estimated the cost effectiveness of a screen and treat strategy. Based on a carriage rate of 31% and a risk reduction of 48%, a saving of approximately $1.5 million10000 patients screened was predicted. In the United States of America for example where 30 million surgical procedures are performed annually, extrapolation results in a saving of $4.5 billion (£3.5 billion). This would reduce the revision burden in the healthcare economy and also patient morbidity.
We acknowledge that this is a retrospective study and therefore has limitations however we aimed to reduce bias by using continuous patients in the non-MRSA group to match the MRSA positive patients by demographic and co-morbidities.
CONCLUSION
In conclusion, our retrospective study has demonstrated that there is a significantly higher risk of MRSA PJI in patients who have had MRSA colonisation undergoing total hip and knee replacements. We advocate rescreening of patients and further eradication treatment. If the patient fails to respond and remains MRSA positive then this can form the basis of discussion during the consent process for joint arthroplasty. Screening and treatment for MRSA is cheap and effective when used which in comparison to the morbidity and cost associated with MRSA PJI.
ARTICLE HIGHLIGHTS
Research background
Difference in screening between two hospital trust which were merging.
Research motivation
Developing a uniform policy for screening and managing methicillin-resistant staphylococcus aureus (MRSA) prosthetic joint infection (PJI).
Research objectives
Eradication therapy is not universally effective. The reasons for this are multifactorial including dose strength and compliance.
Research methods
All patients who underwent total hip and knee arthroplasty between December 2009 and December 2019 were identified. Patients who were also identified as positive for MRSA in the preoperative evaluation. After recording the confirmation of the eradication treatment prescription, all the processes were reviewed retrospectively.The results of each MRSA-positive patient were compared with the results of two MRSA-negative patients who had the same consultant, were of the same age, and had the same surgery.
Research results
Screening identified 42 knee and 32 hip arthroplasty patients as MRSA positive, 84 MRSA negative knee and 64 hip patients were reviewed. Patients were matched with medical co-morbidities in each group. Mean follow up was 5 years. PJI was identified in 4/32 (12.5%) of total hip replacements MRSA positive and 3/42 (7%) of total knee replacements patients. All patients had PJI within one year of surgery.
Research conclusions
MRSA positive patients are given eradication therapy routinely. However, no confirmation of eradication is sought. Patients who have MRSA colonisation preoperatively, in our study had a significantly increased risk of PJI, when compared to negative patients. We would recommend establishing true eradication after treatment prior to arthroplasty.
Research perspectives
Further research needs to be performed into eradication therapy and strategy and also for those patients who do not respond to eradication therapy.
 World Journal of Orthopedics2021年11期
World Journal of Orthopedics2021年11期
- World Journal of Orthopedics的其它文章
- Management of acute length-unstable Monteggia fractures in children: A case report
- Spontaneous pneumothorax in a 17-year-old male patient with multiple exostoses: A case report and review of the literature
- Pathological humerus fracture due to anti-interferon-gamma autoantibodies: A case report
- Allergic dermatitis after knee arthroscopy with repeated exposure to Dermabond Prineo™ in pediatric patients: Two case reports
- Role of coatings and materials of external fixation pins on the rates of pin tract infection: A systematic review and meta-analysis
- Femoral lengthening in young patients: An evidence-based comparison between motorized lengthening nails and external fixation
