移植肾吻合口假性动脉瘤3D-DSA腔内修复初步效果
张鲲鹏 刘京礼 桑桂凤 杨牟
[摘要] 目的 总结三维数字减影血管造影(3D-DSA)在移植肾动脉吻合口假性动脉瘤腔内修复中的应用体会。
方法 回顾性分析2012年4月—2020年10月在我院行腔内修复的4例移植肾动脉吻合口假性动脉瘤病人的3D-DSA影像资料,其中1例病人在二次手術时行第2次3D-DSA检查。
结果 5次3D-DSA经容积重建(VR)获得的三维图像均能清楚显示吻合口假性动脉瘤瘤颈及其与邻近血管的空间解剖关系,为腔内覆膜支架置入和球囊扩张提供最佳的工作角度。
结论 在移植肾动脉吻合口假性动脉瘤病人需要进行腔内介入手术干预时,3D-DSA可作为一项重要的诊疗技术。
[关键词] 肾移植;动脉瘤,假性;血管造影术,数字减影;成像,三维;图像处理,计算机辅助;血管成形术
[中图分类号] R654.3;R816.2
[文献标志码] B
[文章编号] 2096-5532(2021)05-0773-04
doi:10.11712/jms.2096-5532.2021.57.177
[开放科学(资源服务)标识码(OSID)]
[网络出版] https://kns.cnki.net/kcms/detail/37.1517.R.20211029.1732.006.html;2021-11-01 10:52:01
PRELIMINARY EFFECT OF THREE-DIMENSIONAL DIGITAL SUBTRACTION ANGIOGRAPHY IN ENDOVASCULAR REPAIR OF PSEUDOANEURYSM AT THE ARTERIAL ANASTOMOSIS OF THE TRANSPLANTED KIDNEY
ZHANG Kunpeng, LIU Jingli, SANG Guifeng, YANG Mu
(Department of Catheterization Room, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai 264000, China)
[ABSTRACT] Objective To summarize the experience in the application of three-dimensional digital subtraction angiography (3D-DSA) in endovascular repair of pseudoaneurysm at the arterial anastomosis of the transplanted kidney.
Methods A retrospective analysis was performed for the 3D-DSA imaging data of four patients with pseudoaneurysm at the arterial anastomosis of the transplanted kidney who underwent endovascular repair in our hospital from April 2012 to October 2020, among whom one patient underwent 3D-DSA examination for the second time during the second surgery.
Results The three-dimensional images obtained by volume reconstruction of the five times of 3D-DSA clearly displayed the aneurysm neck of pseudoaneurysm at the anastomosis and its spatial anatomical relationship with adjacent blood vessels, which provided the best working angle for endovascular covered stent implantation and balloon dilatation.
Conclusion 3D-DSA can be used as an important diagnosis and treatment technique in patients with pseudoaneurysm at the arterial anastomosis of the transplanted kidney who require intravascular intervention.
[KEY WORDS] kidney transplantation; aneurysm, false; angiography, digital subtraction; imaging, three-dimensional; image processing, computer-assisted; angioplasty
移植肾动脉吻合口假性动脉瘤是一种罕见的血管并发症,其发生率为0.3%[1]。该病具有潜在的破坏性,可能破裂而导致移植肾丢失[2]。其病因通常为缝合技术缺陷、术中血管壁损伤或局部感染引起的吻合口动脉破裂[3-4]。近年来,血管腔内修复已成为移植肾动脉吻合口假性动脉瘤的一种有效治疗方法[2,5-6],最大程度避免了大血管重建手术创伤以及相关并发症的发生[7]。三维数字减影血管造影(3D-DSA)已被公认为神经介入放射学脑血管疾病诊断的金标准[8-11],其检测能力明显优于三维计算机断层血管造影(3D-CTA)和二维数字减影血管造影(2D-DSA)[12-13]。我们将3D-DSA技术运用于4例移植肾动脉吻合口假性动脉瘤病人的诊疗中,本文总结其应用体会,探讨其可行性。
1 资料与方法
1.1 一般资料
我院泌尿外器官移植科于2012年4月—2020年10月共完成约1 500例肾移植手术,其中4例经B超、CTA检查明确诊断为移植肾动脉吻合口假性动脉瘤(均行同种异体肾移植、盆腔内移植肾动脉与右髂外動脉端侧吻合手术)。4例病人,男性3例,女性1例;年龄23~56岁,平均44岁。从移植到诊断假性动脉瘤时间间隔为(105±36)d。临床表现:3例无症状,通过肾移植术后例行复查诊断;1例出现发热、腰痛和少尿的症状。诊断后均由我院血管外科医生行覆膜支架腔内修复。
1.2 检查方法
本文4例病人共进行5次2D-DSA和3D-DSA检查,其中1例病人因术后切口感染、吻合口出血进行了第2次2D-DSA和3D-DSA检查。
2D-DSA:使用美国GE innova 4100平板血管造影机,利用Seldinger技术经股动脉穿刺置管行右侧髂外动脉正位2D-DSA检查,FOV=32 cm,采集帧频为每秒4帧。使用高压注射器注入非离子型对比剂碘克沙醇,注射总量为6~8 mL,注射流量为3~4 mL/s,压力限制2 MPa。
3D-DSA:将5F多功能导管置于右侧髂外动脉起始段,FOV=32 cm,使用高压注射器注入非离子型对比剂碘克沙醇,注射总量为18 mL,注射流量为3 mL/s,压力限制为2 MPa,设置X线延迟1.5 s。C臂以40(°)/s的速度先后2次旋转扫描共采集294幅原始图像,采集的原始数据自动传至GE AW4.6工作站,经容积重建(VR)以512×512矩阵处理得到三维血管影像。
1.3 图像分析
所得2D-DSA和3D-DSA图像分别由1名高年资影像科医师和1名血管外科医师独立判读,从不同角度观察移植肾动脉吻合口假性动脉瘤的瘤体、瘤颈及其邻近血管的解剖结构,选择腔内修复最佳的工作角度。利用软件工具测量假性动脉瘤瘤颈大小及邻近血管的直径。
2 结 果
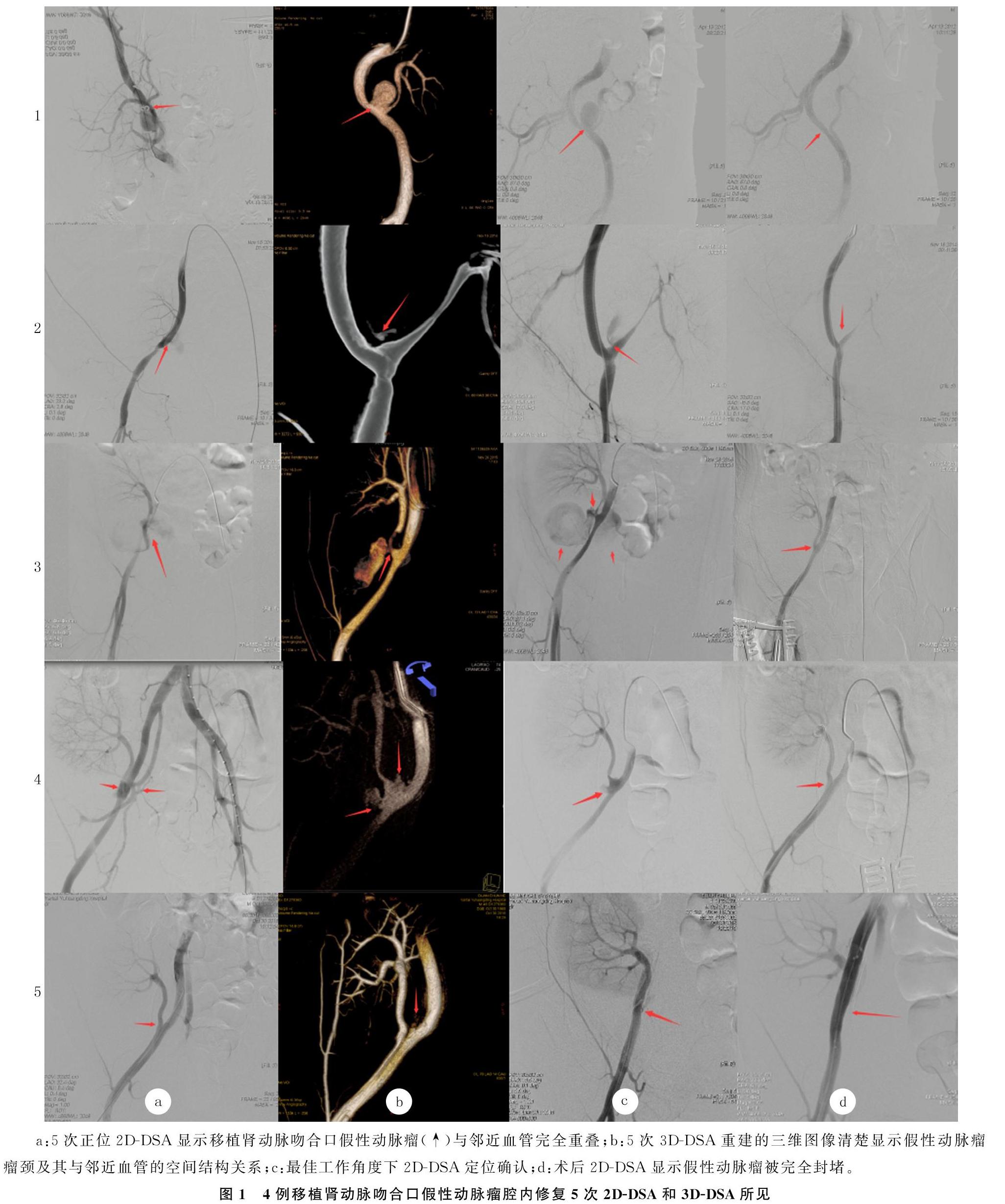
本文4例病人5次正位2D-DSA均能提示吻合口假性动脉瘤形成,但假性动脉瘤与邻近血管明显重叠,不能清楚显示假性动脉瘤瘤颈及其与邻近血管的空间解剖关系(图1a)。5次3D-DSA经VR获得的三维图像均能清楚显示吻合口假性动脉瘤瘤颈及其与邻近血管的空间解剖关系,可为腔内覆膜支架置入和球囊扩张提供最佳的工作角度(图1b),并可依据假性动脉瘤瘤颈大小和邻近血管的直径选择合适尺寸的覆膜支架和球囊。血管外科医生依据最佳工作角度准确定位(图1c),成功置入覆膜支架并完成球囊扩张。术后2D-DSA显示假性动脉瘤被完全封堵(图1d)。
本文4例病人术后均服用阿司匹林及氯吡格雷联合治疗3个月,随访6~36个月。其中3例病人移植肾彩超和肾功能复查均正常;1例病人术后12个月复查发现肌酐升高,住院予以抗排斥等治疗,术后24个月复查发现尿量少,每日约50 mL,肌酐约580 μmol/L,随后择期行第2次同种异体肾移植术,术后随访12个月移植肾功能正常。
3 讨 论
近些年来,血管腔内修复已成为移植肾动脉吻合口假性动脉瘤的有效治疗方法[2,5-6]。
通过腔内置入覆膜支架来阻止血流继续流入假性动脉瘤内,有效降低了其破裂风险[14]。SMEDS等[15]首次报道了成功使用覆膜支架腔内修复移植肾吻合口假性动脉瘤。大多数关于血管腔内修复的报道显示为单独使用覆膜支架,并取得了良好的效果[16-21]。
旋转技术最早在1972年由CORNELIS等[22]提出,但直到1983年才有临床应用的报道[23]。由于设备的改进,在1989年数字减影技术产生[24],在1997年血管旋转造影的三维重建被报道[25]。随着科学技术和医学的不断进步,3D-DSA技术被广泛应用于医学各个领域。目前,磁共振血管成像(MRA)、3D-CTA和3D-DSA技术被更多地运用在神经血管疾病的诊断中。其中,3D-DSA已被公认为神经介入放射学脑血管疾病诊断的金标准[8-11]。目前已有许多文献报道了3D技术在临床中的广泛应用[26-27],但3D-DSA应用于移植肾动脉吻合口假性动脉瘤的相关报道尚不多见。
传统的2D-DSA通过多角度靶血管造影来显示病变,这不仅延长了手术时间,而且在一定程度上增加了造影剂用量及操作人员和病人的辐射暴露。肾移植病人的血管解剖通常复杂而且迂曲,端侧吻合动脉解剖结构常以重叠、成角关系成像于正位影像上。移植肾吻合口假性动脉瘤腔内覆膜支架置入在技术上具有一定的挑战性。在这种情况下,更全面清楚地了解假性动脉瘤瘤颈及吻合口邻近血管的解剖结构,保证支架的准确定位和通畅性是至关重要的。对于这类肾功能减退的病人,要在手术顺利进行的前提下尽可能减少造影剂用量和造影次数,避免因延长手术时间而增加手术并发症及辐射暴露的风险[28]。
3D-DSA与传统2D-DSA相比有明显优势:①一次旋转造影可以获得多角度的空间影像,能够从不同角度动态观察假性动脉瘤的血流动力学表
现;②3D-DSA能够减少造影次数和造影剂用量,减少手术时间和辐射暴露,从而大大降低这些不利因素带来的风险[29];③经VR获得的清晰三维图像空间分辨率更高,使医生能够多角度地观察病变部位,有效排除了血管重叠、成角等因素的干扰,对移植肾动脉吻合口假性动脉瘤及邻近分支血管有较好的成像能力,能够正确提示假性动脉瘤瘤颈的位置、大小及其与邻近血管的空间解剖关系;④有利于血管外科医生选择腔内修复最佳的工作角度,并根据直接测量结果选取合适的覆膜支架和球囊,有利于腔内手术的准确定位。本文中1例病人行第2次手术时,因已置入覆膜支架,2D-DSA未能清楚显示假性动脉瘤,而3D-DSA可清楚显示残存的假性动脉瘤瘤颈。故3D-DSA能准确诊断移植肾动脉吻合口假性动脉瘤,比2D-DSA更适合血管腔内介入诊疗。
綜上所述,3D-DSA经VR所获得的高空间分辨率的三维图像可清楚显示移植肾动脉吻合口假性动脉瘤,在显示假性动脉瘤瘤颈及其与邻近血管的空间解剖关系方面明显优于2D-DSA,有利于腔内修复的准确定位和提高疗效。在移植肾动脉吻合口假性动脉瘤病人需要进行腔内介入手术干预时,3D-DSA可作为一项重要的诊疗技术。
[参考文献]
[1]DIMITROULIS D, BOKOS J, ZAVOS G, et al. Vascular complications in renal transplantation: a single-center expe-rience in 1367 renal transplantations and review of the literature[J]. Transplantation Proceedings, 2009,41(5):1609-1614.
[2]GANG S, RAJAPURKAR M. Vascular complications follo-wing renal Transplantation[J]. Journal of Nephrology and Renal Transplantation, 2009,2:122-132.
[3]NGUAN C Y, LUKE P P. Renal artery pseudoaneurysm of infectious etiology: a life-threatening complication after renal transplantation[J]. Urology, 2006,68(3):668-669.
[4]BAXTER G M. Ultrasound of renal transplantation[J]. Clinical Radiology, 2001,56(10):802-818.
[5]BRACALE U M, CARBONE F, DEL GUERCIO L, et al. External iliac artery pseudoaneurysm complicating renal transplantation[J]. Interactive CardioVascular and Thoracic Surge-ry, 2009,8(6):654-660.
[6]HEGDE U N, RAJAPURKAR M M, GANG S D, et al. Percutaneous endovascular management of recurrent aneurysm of transplant renal artery anastomosed to internal iliac artery[J]. Indian Journal of Urology: IJU: Journal of the Urological Society of India, 2008,24(3):411-413.
[7]CURTI T, STELLA A, ROSSI C, et al. Endovascular repair as first-choice treatment for anastomotic and true iliac aneurysms[J]. Journal of Endovascular Therapy, 2001,8(2):139-143.
[8]CONNOLLY E S Jr, RABINSTEIN A A, CARHUAPOMA J R, et al. Guidelines for the management of aneurysmal su-
barachnoid hemorrhage: a guideline for healthcare professi-
onals from the American Heart Association/American Stroke Association[J]. Stroke, 2012,43(6):1711-1737.
[9]KUCUKAY F, OKTEN R S, TEKINER A, et al. Three-dimensional volume rendering digital subtraction angiography in comparison with two-dimensional digital subtraction angio-
graphy and rotational angiography for detecting aneurysms and their morphological properties in patients with subarachnoid hemorrhage[J]. European Journal of Radiology, 2012,81(10):2794-2800.
[10]LANZMAN R S, KRPIL P, SCHMITT P, et al. Nonenhanced ECG-gated time-resolved 4D steady-state free precession (SSFP) MR angiography (MRA) for assessment of cerebral collateral flow: comparison with digital subtraction an-
giography (DSA)[J]. European Radiology, 2011,21(6):1329-1338.
[11]VAN ROOIJ W J, SPRENGERS M E, DE GAST A N, et al. 3D rotational angiography: the new gold standard in the detection of additional intracranial aneurysms[J]. AJNR American Journal of Neuroradiology, 2008,29(5):976-979.
[12]VAN ROOIJ W J, PELUSO J P, SLUZEWSKI M, et al. Additional value of 3D rotational angiography in angiographically negative aneurysmal subarachnoid hemorrhage: how negative is negative[J]? AJNR American Journal of Neuroradiology, 2008,29(5):962-966.
[13]KAWASHIMA M, KITAHARA T, SOMA K, et al. Three-dimensional digital subtraction angiography vs two-dimensional digital subtraction angiography for detection of ruptured intracranial aneurysms: a study of 86 aneurysms[J]. Neurology India, 2005,53(3):287-289;discussion290.
[14]TAGHAVI M, SHOJAEE FARD A, MEHRSAI R, et al. Late onset anastomotic pseudoaneurysm of renal allograft artery: case report, diagnosis, and treatment[J]. Transplantation Proceedings, 2005,37(10):4297-4299.
[15]SMEDS M R, OFSTEIN R, PETERSON G J, et al. Endovascular repair of a Para-anastomotic pseudoaneurysm after renal autotransplantation: an alternative to open reconstruction[J]. Annals of Vascular Surgery, 2013,27(1):110.e5-110.e8.
[16]KOO C K, RODGER S, BAXTER G M. Extra-renal pseudoaneurysm: an uncommon complication following renal transplantation[J]. Clinical Radiology, 1999,54(11):755-758.
[17]ZAVOS G, PAPPAS P, KAKISIS J D, et al. Endovascular repair as first-choice treatment of iliac pseudoaneurysms follo-
wing renal transplantation[J]. Transplantation Proceedings, 2005,37(10):4300-4302.
[18]MCINTOSH B C, BAKHOS C T, SWEENEY T F, et al. Endovascular repair of transplant nephrectomy external iliac artery pseudoaneurysm[J]. Connecticut Medicine, 2005,69(8):465-466.
[19]FREYRIE A, ROSSI C, CIRELLI M R, et al. Endovascular treatment of a false aneurysm in the site of nephrectomy of a transplanted kidney[J]. Italian Journal of Vascular and Endovascular Surgeryg, 1999,6(2):129-138.
[20]DILLER R, HLZEN J, SENNINGER N, et al. Interventional stenting for ruptured iliac aneurysm following transplant nephrectomy[J]. Transplantation Proceedings, 2006,38(3):718-720.
[21]LIAPIS C D, PETRIKKOS G L, PARASKEVAS K I, et al. External iliac artery stent mucormycosis in a renal transplant patient[J]. Annals of Vascular Surgery, 2006,20(2):253-257.
[22]CORNELIS G, BELLET A, VAN EYGEN B, et al. Rotational multiple sequence roentgenography of intracranial aneurysms[J]. Acta Radiologica: Diagnosis, 1972,13(1):74-76.
[23]THRON A, VOIGT K. Rotational cerebral angiography: Procedure and value[J]. American Journal of Neuroradiology, 1983,4(3):289-291.
[24]SCHUMACHER M, KUTLUK K, OTT D. Digital rotational radiography in neuroradiology[J]. American Journal of Neuroradiology, 1989,10(3):644-649.
[25]CARSIN M, CHABERT E, CROCI S, et al. The role of 3-dimensional reconstructions in the angiographic evaluation of cerebral vascular malformations:3D morphometry[J]. Journal De Neuroradiologie, 1997,24(2):137-140.
[26]ANZALONE N, RIGHI C, SIMIONATO F, et al. Three-dimensional time-of-flight MR angiography in the evaluation of intracranial aneurysms treated with Guglielmi detachable coils[J]. American Journal of Neuroradiology, 2000,21(4):746-752.
[27]SATO M, ENDO Y, MATSUMOTO M, et al. Three-dimensional CT angiography in acute cerebral aneurysm surgery[J]. Japanese Journal of Neurosurgery, 2001,10(1):18-26.
[28]PEDICELLI A, ROLLO M, LELLA G M, et al. 3D rotational angiography for the diagnosis and preoperative assessment of intracranial aneurysms: preliminary experience[J]. La Radiologia Medica, 2007,112(6):895-905.
[29]BECK J, ROHDE S, BERKEFELD J, et al. Size and location of ruptured and unruptured intracranial aneurysms measured by 3-dimensional rotational angiography[J]. Surgical Neurology, 2006,65(1):18-25;discussion25-27.
(本文編辑 马伟平)