Molecular Spectrum of α- and β-Thalassemia among Young lndividuals of Marriageable Age in Guangdong Province,China*
ZHOU Bing Yi, WANG Yong Xia, XU Shan Shan, GU Heng, and LI Ming Zhen
Key words: Thalassemia; Guangdong Province;Molecular spectrum; Marriageable age; China
Thalassemia is a group of genetically heterogeneous diseases characterized by hemolytic anemia due to a genetic defect that results in insufficient or reduced synthesis of one or more hemoglobin chains[1]. The two most common types are α- and β-thalassemia. Alpha-thalassemia is a group of hemolytic anemias caused by impaired α-globin chain synthesis owing to deletion or functional defects in the four alpha-globin genes located on chromosome 16. Beta-thalassemia is a group of hemoglobinopathies in which β-chain synthesis is partially or completely inhibited due to mutations, or rare deletions, of the two beta-globin genes located on chromosome 11. The clinical phenotypes of thalassemia range from asymptomatic to fatal hemolytic anemia with considerable variation. At present, patients with moderate or severe thalassemia often manifest lifelong anemia requiring blood transfusions and iron chelation; however, the definitive cure is through bone marrow transplantation.
Worldwide, thalassemia is most frequent in South China, the Middle East, Southeast Asia, the Mediterranean region, and the Indian subcontinent[2]. Thalassemia has been reported to be highly prevalent in Hainan, Guangxi, and Guangdong in southern China[3]. A meta-analysis indicated that the prevalence of α-, β-, and compound α/β-thalassemia in mainland China was 7.88%,2.21%, and 0.48%, respectively[3]. Thalassemia imposes considerable financial burdens on many families and society, and has become a serious public health problem.
Guangdong Province, located in southern China,has more than 100 million permanent residents that account for 8% of the population in China and has a high incidence of thalassemia. To date, there are few studies on molecular spectrum of α- and β-thalassaemia among young individuals of marriageable age in Guangdong Province based on a large sample. The free pre-pregnancy eugenic health examination project has been conducted in Guangdong Province for comprehensive prevention and control of thalassemia major. Therefore, using data from this project, we conducted a large-scale investigation to detect and analyze α- and βthalassemia gene mutations in subjects suspected to have thalassemia in Guangdong Province in order to decode the epidemiological background of thalassemia and provide data to support optimization of thalassemia prevention and control strategies.
Individuals who participated in the free prepregnancy eugenic health examination project in Guangdong Province from January 2018 to December 2019 were screened and patients suspected of having thalassemia were enrolled in this study. The study subjects were premarital or preconception stage couples and pregnant women.Peripheral venous blood samples were collected from each subject and molecular testing for thalassemia was performed. Subjects that were determined to be thalassemia carriers were further offered genetic counseling. The study was approved by the Ethics Committee of the Family Planning Research Institute of Guangdong Province. All participants provided written informed consent.
Mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) were commonly used as screening indicators for thalassemia, with the cut-off values of MCV and MCH being 80 fL and 27 pg, respectively. Positive thalassemia screening was defined as MCV < 80 fL and/or MCH < 27 pg,while subjects with MCV ≥ 80 fL and/or MCH ≥ 27 pg were regarded as non-carriers of thalassemia or nonclinically thalassemia carrier. Approximately 2 mL of venous blood was collected to test hematological parameters, including MCV and MCH, which were measured by an automated cell counter according to standard laboratory procedures. Subjects were suspected to be thalassemia carriers if they had MCV and/or MCH values below the cut-off values (MCV <80 fL and/or MCH < 27 pg). All thalassemia-positive samples were stored as blood cards and sent to Guangzhou KingMed Diagnostics Group Co., Ltd.(Guangzhou, China) for genetic detection of thalassemia. Genomic deoxyribonucleic acid (DNA)was isolated from peripheral blood leukocytes using TIANamp Genomic DNA kits (TIANGEN Biotech, Co.,Ltd., Beijing, China), according to the manufacturer’s instructions. Gap-polymerase chain reaction was used to detect the three common deletional α-thalassemia types (--SEA, -α3.7, and -α4.2), and polymerase chain reaction-reverse dot blot was used to detect α-thalassemia and β-thalassemia mutations using the thalassemia gene detection kit(Yaneng Bioscience Co., Ltd., Shenzhen, China).Three α-thalassemia point mutations and 17 common β-thalassemia mutations were revealed in the Chinese population and are as follows: Hb Constant Spring (Hb CS; HBA2: c.427T > C), Hb Westmead (Hb WS; HBA2: c.369C > G), Hb Quong Sze (Hb QS; HBA2: c.377T > C), CD41-42 (-TCTT), IVSII-654 (C > T), CD43 (GAG > TAG), CD26 (GAG > AAG),-28 (A > G), CD17 (AAG > TAG), CD31 (-C), -30 (T > C),CD71-72 (+A), IVS-I-5 (G > C), Int (ATG > AGG), CD14-15 (+G), CD27-28 (+C), -29 (A > G), -32 (C > A), IVS-I-1(G > T), and Cap (-AAAC) (HGVS nomenclature were shown in Table 1). For suspected rare thalassemia cases, DNA sequencing was performed to identify rare and unknown thalassemia gene mutations. Data analysis was performed with IBM SPSS Statistics v.26 software (IBM Corp., Armonk, NY, USA). Descriptive statistics was used to analyze the genotypic and allelic frequencies of thalassemia.
A total of 24,788 subjects (12,397 men and 12,391 women), ranging from 20 to 54 years of age,were screened for thalassemia. Of all the samples,14,346 (57.87%) were diagnosed with thalassemia,including 7,556 cases of α-thalassemia alone(52.67%), 5,860 cases of β-thalassemia alone(40.85%), and 930 cases of compound α/β-thalassemia (6.48%). The previous survey showed that the overall prevalence of thalassemia in the Guangdong population was 16.45%[4]. The prevalence of α-, β-, and combined α-/β-thalassemia were 12.03%, 3.80%, and 0.63% respectively[4]. In agreement with the findings of other studies on thalassemia in Guangdong Province, there were more cases of α-thalassemia in this study[4,5].Currently, over 1,000 gene mutations of thalassemia have been entered in the IthaGenes database;α-thalassemia mutations are primarily deletions,while β-thalassemia mutations are primarily point mutations. Thalassemia is heterogeneous, with significant geographical differences and population specificity[5,6].
Among the 7,556 α-thalassemia cases, 7,245(95.88%) cases had heterozygous mutations, 282(3.73%) cases had compound heterozygous mutations, and 29 cases (0.38%) had homozygous mutations. Meanwhile, 25 different genotypes were identified. The three most frequent mutations were seen in genotypes --SEA/αα (67.83%), -α3.7/αα(14.93%), and -α4.2/αα (6.60%). Five common Hb H genotypes were detected, including two deletional types (--SEA/-α3.7) and (--SEA/-α4.2), and three nondeletional types (--SEA/-αCS), (--SEA/-αWS), and (--SEA/-αQS). In addition, two rare α-thalassemia genotypes were detected, including two cases of Thai thalassemia (--THAI, NC_000016.10:g.149863_183312del) and two cases of Hong Kongαα (HKαα)thalassemia (Table 2). However, the genotypes of αthalassemia differed in regions and populations; the-α3.7/αα and -α4.2/αα genotypes were more frequent than the --SEA/αα genotype among the Li people in Hainan, and the ααCS/αα genotype was more frequent than the -α4.2/αα genotype in the Baise and Yulin regions[7-9]. Among the 5,860 cases of βthalassemia, 18 different genotypes were identified.The most frequent genotype was βCD41-42/βN(38.05%), followed by βIVS-II-654/βN(25.70%), β-28/βN(15.87%), and βCD17/βN(10.00%), and the above four genotypes accounted for 89.62% of all β-thalassemia genotypes. In addition, three rare genotypes of βthalassemia were detected, including βCD113/βN(eight cases), β-90/βN(two cases), and βCD56/βN(one case)(Table 2). Among the 930 cases of compound α/βthalassemia, 458 cases (49.25%) had α+thalassemia and β-thalassemia, 457 cases (49.14%) had α0thalassemia and β-thalassemia, 15 cases (1.61%) had Hb H disease and β-thalassemia (Table 2) (The specific genotypes were shown in Supplementary Table S1, available in www.besjournal.com). Hb H disease is caused by the loss of function of three α-globin genes and the clinical severity of patients is variable, depending on the type of α-globin mutations. Clinically, patients with double heterozygous thalassemia often present with mild anemia. This is due to the reduced synthesis of both α- and β-globin chains, which extenuates the imbalance of globin chain synthesis and alleviates anemia symptoms. Since mild compound α/βthalassemia rarely causes phenotypic aggravation of the disease, attention should be paid to whether both spouses are α- or β-thalassemia heterozygous carriers or compound α/β-thalassemia gene carriers in the premarital and preconception examination. If both spouses are double heterozygous thalassemia carriers, the risk of having a child with thalassemia major may increase.
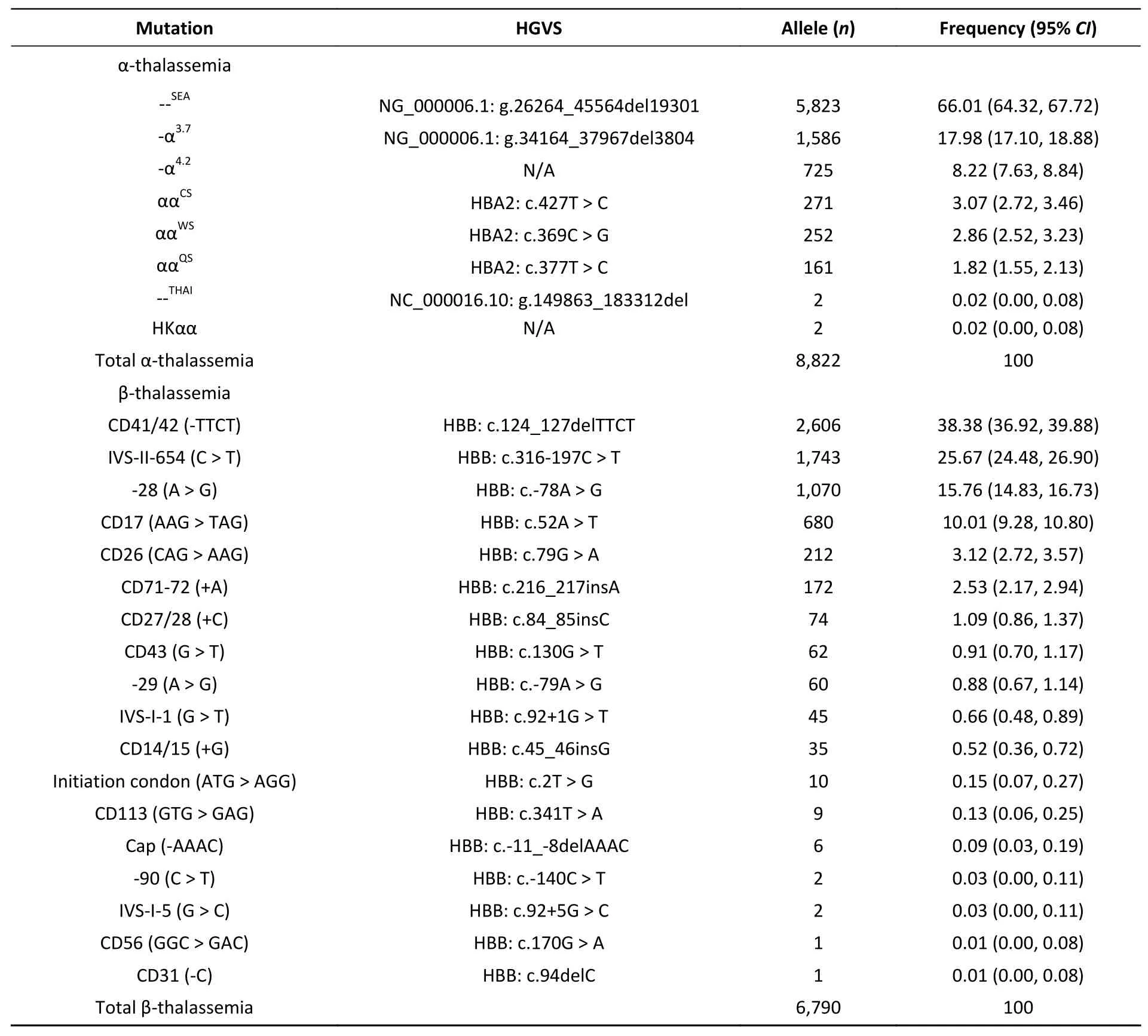
Table 1. Allelic frequencies of thalassemia in Guangdong Province
In this study, eight different mutation types of αthalassemia were detected, and the three deletion mutations (--SEA, -α3.7, and -α4.2) accounted for approximately 92% of all α-thalassemia mutations in Guangdong Province (Table 1). The --SEAdeletion was the most common mutation (66.01%), followed by-α3.7deletion (17.98%) and -α4.2deletion (8.22%),which was similar to the findings of α-thalassemiastudies conducted in Fujian, Yunnan, and Hubei[6,10,11]. The other most common α-thalassemia point mutations (and their respective allele frequencies) are: ααCS(3.07%), ααWS(2.86%), and ααQS(1.82%). Among the non-deletion mutations,the detection rate of ααWSwas higher than that in previous studies[4]. In addition, --THAImutations,regarded as rare mutations in China, were detected in two cases, and the allelic frequency was only 0.02% in this study. Because of the rarity of the --THAImutation in southern China, it is not routinely detected, which usually leads to missed diagnosis.Furthermore, two cases were identified as positive for HKαα/αα with the allele frequency of 0.02% in Guangdong population. It was reported that HKαα/αα carriers and -α3.7/αα carriers had similar phenotypes and showed small-cell hyperpigmented anemia or normal hematologic manifestations[12]. If one spouse is a carrier of α-thalassemia and the other has positive hematological phenotypes, or if a baby was born with severe or moderate thalassemia,but no mutations were detected by applying the routine thalassemia diagnostic kit, rare mutations should be seriously considered to prevent missed diagnosis[6]. Meanwhile, eighteen different mutation types of β-thalassemia were detected in this study,and CD41-42 (-TTCT) mutation is the most common mutation (38.38%), followed by IVS-II-654 (C > T)(25.67%), -28 (A > G) (15.76%), and CD17 (AAG >TAG) (10.01%) (Table 1). In addition, three rare βthalassemia mutations were detected, including CD113 (GTG > GAG), CD56 (GGC > GAC), and -90 (C >T). The genotype proportions coincided with the allelic frequencies of β-thalassemia. The types and frequencies of β-gene mutations correlate with the regional and ethnic distribution. The CD41-42 mutation was the most frequent, in consistent with the findings in Hainan and Yulin of Guangxi[8,10].However, the IVS-II-654 mutation was the most frequent in Fujian and Hubei[6,11], and the CD17 mutation was the most frequent in Baise of Guangxi and Yunnan[8,10]. It was reported that the IVS-II-654 mutation had the highest frequency with 40.81%,followed by CD41-42(-TCTT) (32.44%) in the Hakka population in Guangdong[5]. The reason for this discrepancy may be due to the ethnic specificity of β-thalassemia. Moreover, we identified three rare types of mutations, and did not detect compound heterozygotes and homozygotes of β-thalassemia.The most likely explanations are the following:1) the implementation of the premarital and preconception screening programs for thalassemia may have resulted in a lower birth rate of compound heterozygotes and pure heterozygotes; and 2) severe acute anemia may result in a higher mortality rate among children due to the lack of diagnostic facilities and treatment measures. Under these circumstances, it appears that most homozygotes and compound heterozygotes would have died early in life without effective medical rescue. The results indicate that β-thalassemia is diverse and genetically heterogeneous, and the few rare and unknown gene mutations should be further investigated.
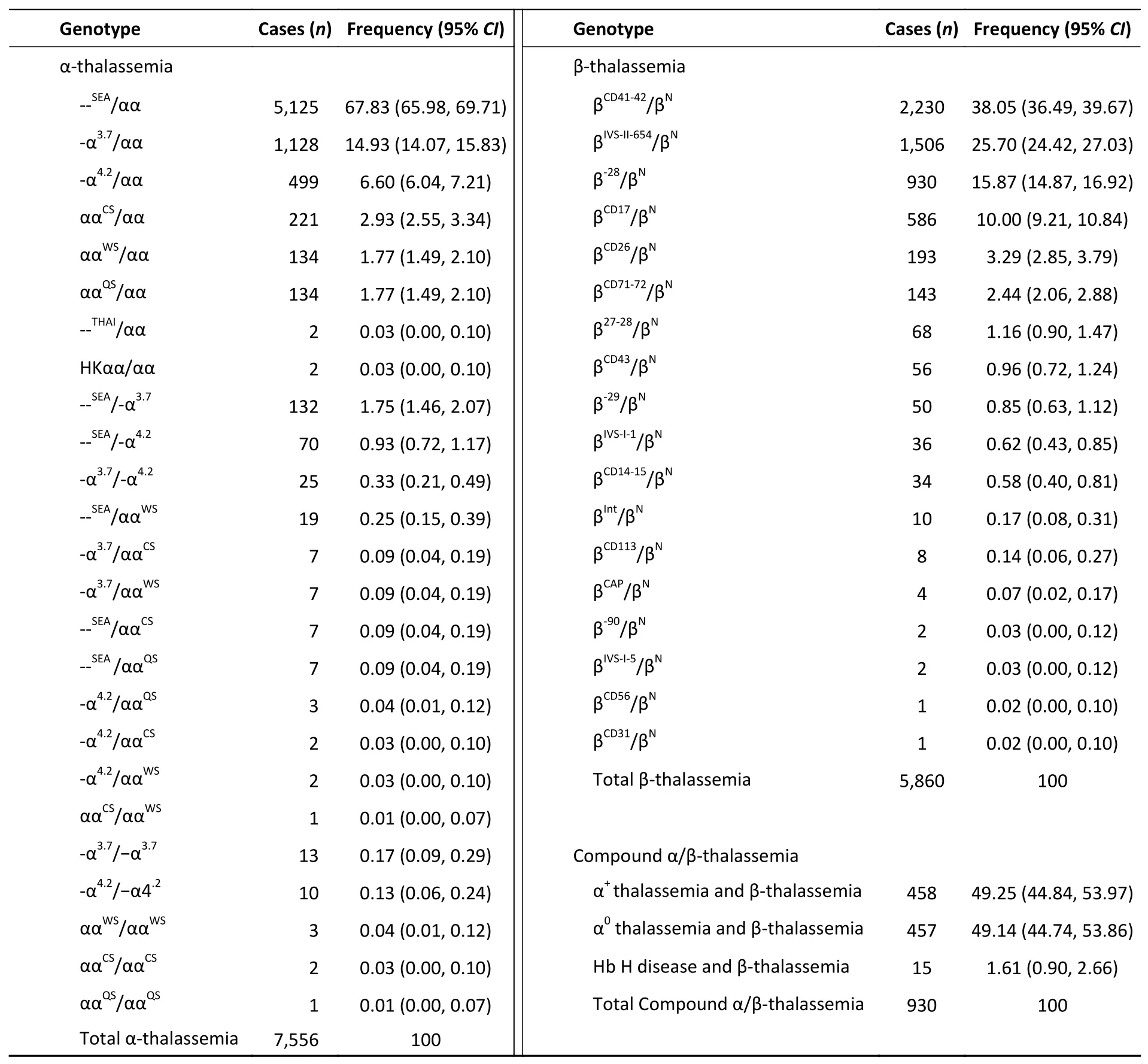
Table 2. Genotype, case and frequency of thalassemia in Guangdong Province
The limitation of this study is that it did not demonstrate the prevalence of thalassemia because the study included only subjects suspected of having thalassemia, and did not include randomized population.
In conclusion, this study investigated the genotype distribution and allele frequencies of αand β-thalassemia among young individuals of marriageable age in Guangdong Province, and demonstrated that thalassemia is heterogeneous with significant geographical differences and population specificity. Our findings is important to decode the epidemiological background of thalassemia. In addition, the results suggested that the detection of rare and unknown thalassemia gene mutations should be given serious consideration.Moreover, the study provided a valuable reference for genetic counseling and prenatal diagnosis and data to support optimization of thalassemia prevention and control strategies.
Conflicts of InterestThe authors declare no potential conflicts of interest.
AcknowledgmentsThe authors sincerely thank all staff of Guangzhou KingMed Diagnostics Group Co.,Ltd. for their collaboration in thalassemia detection and data collection.
Authors’ ContributionsZHOU Bing Yi contributed to data collection and analysis, and drafted the manuscript. WANG Yong Xia contributed to data collection and revised the manuscript for important intellectual content. XU Shan Shan contributed to thalassemia diagnosis and data analysis. GU Heng contributed to data collection and analysis. LI Ming Zhen contributed to study design, thalassemia diagnosis, and data analysis. All authors have read and approved the final version of the manuscript.
&These authors contributed equally to this work.
#Correspondence should be addressed to LI Ming Zhen, Tel: 86-13660775576, E-mail: bzh777@163.com
Biographical notes of the first authors: ZHOU Bing Yi,female, born in 1979, Master’s Degree, majoring in medical genetics; WANG Yong Xia, female, born in 1980,Master’s Degree, majoring in pathology.
Received: January 3, 2021;
Accepted: April 6, 2021
 Biomedical and Environmental Sciences2021年10期
Biomedical and Environmental Sciences2021年10期
- Biomedical and Environmental Sciences的其它文章
- Deep Learning in Chest Radiography: Detection of Pneumoconiosis*
- Relationship between TERT Polymorphism and Telomere Length in Workers Exposed to Omethoate*
- lsolation and Characterization of Vagococcus fluvialis from Bats*
- Cerebrospinal Fluids from Patients with Five Common Genetic Prion Diseases in China Display Distinct Reactivities in the RTQulC Assays*
- Obesity rather than Metabolic Syndrome is a Risk Factor for Subclinical Hypothyroidism and Thyroid Autoimmunity*
- The Combined Effect of Dyslipidemia on the lncidence of Type 2 Diabetes: A Prospective Cohort Study in Northwest of China*
