Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
Dina Abd Elfattah, Faried Wagdy, Tharwat Mokbel, Hisham Elsorogy, Abd-Elmonem A. Elhesy
1Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University, Mansoura 35516, Egypt
2Menofia University Hospital, Menofia University, Menofia 32511, Egypt
Abstract
● KEYWORDS: stenting; ligation; Ahmed valve; hypotony;glaucoma
INTRODUCTION
Refractory glaucoma is a complicated type of glaucoma that is characterized by high intraocular pressure(IOP), making it difficult to treat by traditional medical or surgical therapies. Trabeculectomy has shown poor long-term outcomes for refractory glaucoma, making shunt surgery a better alternative[1]. Ahmed glaucoma valve (AGV) is effective procedure in management of refractory glaucoma with longterm follow-up in Egyptian patients[2]. AGV, a shunt device,is used either initially or after conventional procedures fail to treat refractory glaucoma. The aqueous humor flows directly through the silicone tube attached to the valve plate[3].
It is effective in reducing the postoperative hypotony that is commonly seen in patients with non-valved implants.However, persistent hypotony is a postoperative complication of AGV usage[4-7]. This is caused by over-priming of the tube and excessive manipulation of the valve housing that can damage the valve mechanism. The outflow of aqueous humor around the silicone tube immediately after performing sclerostomy using a 22G or 23G needle and failure of ciliary body function are other complications associated with AGV usage[8-9]. Closure of the tube by ligation or stenting may be needed when postoperative ocular hypotony occurs[10];however, it does not have adequate control on the outflow[11].Postoperative ocular hypotony can be managed effectively by ab interno tube stenting[12-14]. This study aimed to compare the effectiveness of using intraluminal stenting and external ligation of AGV as modifications to the conventional surgery for refractory glaucoma management and their efficacy in postoperative hypotony prevention.
SUBJECTS AND METHODS
Ethical Approval This prospective blind randomized study was conducted from September 2018 to January 2020 in Menofia University Hospital (ClinicalTrials.gov Identifier:NCT04508881). Approval was provided by the institutional research board committee, and informed written consent was obtained from all participants included in the study.
A total of 30 eyes of 25 patients with refractory glaucoma were included in this randomized study that used a computergenerated random number table. The patients were aged 44 to 56y. Despite taking the tolerated medication after previous trabeculectomy surgery, these patients had high IOP.
The patients were divided into two groups: AGV with intraluminal stenting group (group I,n=15 eyes) and AGV with external ligation group (group II,n=15 eyes). These cases were followed for one year after surgery. The outcome was measured as IOP and its association with the number of postoperative glaucoma medications. A complete success was considered if IOP>6 mm Hg and ≤ 21 mm Hg without medications. A qualified success was considered if IOP >6 mm Hg and ≤ 21 mm Hg with medications, and an IOP<6 mm Hg was defined as hypotony. All patients were preoperatively subjected to IOP measurement using a Goldman applanation tonometer, visual acuity (VA) assessment using a Snellen E chart, visual field (VF) analysis by a Humphrey VF analyzer,angle examination by a goniolens, optic disc examination by a Volk+90 lens, slit lamp examination for assessment of corneal clarity, and assessment for any corneal tube-touch and measurement of anterior chamber depth. All patients were given peribulbar anesthesia. In group I, incision of superiortemporal conjunctiva was performed, and the valve body plate was placed approximately 10 mm posterior to the corneal limbus. A 7-0 Prolene thread was inserted into the tube lumen;inserted along the tube without arriving to the valve plate, and it was removed by fine forceps after 2mo postoperatively in all cases through paracentesis applied at the limbus opposite the tube after inflation of anterior chamber with viscelastic(Figure 1). In group II, the same procedure was followed, 2 interrupted 8-0 Vicryl sutures were used to fixate the tube with the underlying sclera along with two interrupted 8-0 Vicryl sutures that were placed 2 mm apart over the tube itself to partially occlude it and then inserted into the anterior chamber(Figure 2). Those two Vicryl interrupted sutures (absorbable sutures) that were used in external ligation of the tube, were left to be absorbed without removal. A postoperative treatment course of combined antibiotic and steroid eye drops every four hours in the first week, gradually tapered over the next two weeks, was prescribed. IOP, VA, and VF assessments, optic disc examination by Volk+90 lens, and slit lamp examination were performed at the follow-up. Failure was considered if the patient needed implant removal, additional glaucoma surgery,or developed phthisis bulbi.
Statistical Analysis Data were statistically analyzed using SPSS version 22 (SPSS Inc., Chicago, IL, USA) software.Non-pairedttest and Mann-WhitneyUtest were applied to the quantitative variables. Fisher’s exact test was applied to the qualitative variables. Correlation was used to assess the strength and direction of association.P<0.05 was considered to be statistically significant.
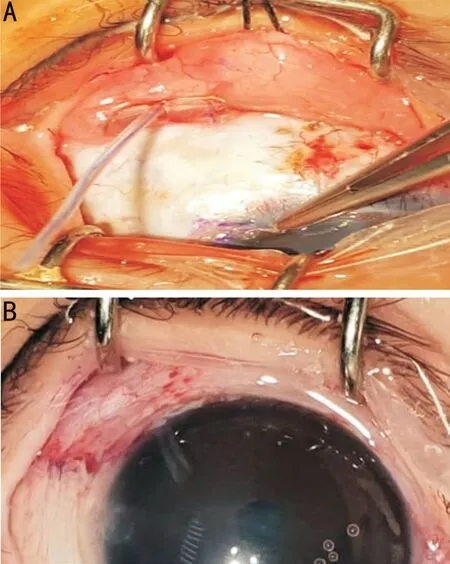
Figure 1 A 50-year-old female patient (intraluminal stenting group) A: An intraoperative intraluminal Prolene stenting; B: The tube implanted in anterior chamber one month after the surgery.
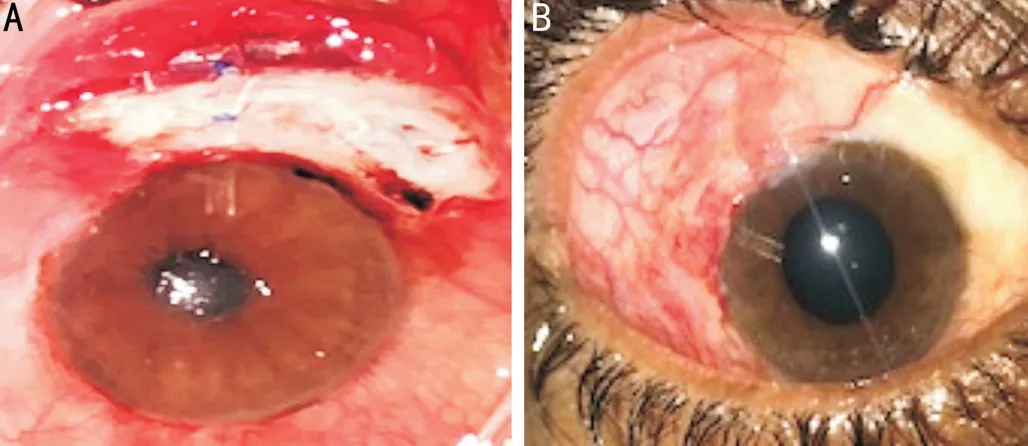
Figure 2 A 48-year-old male patient (external ligation group) A:The two intraoperative vicryl sutures used in ligation with partial occlusion of the tube before tube fixation by another two vicryl sutures; B: The tube implanted in anterior chamber 3mo after the surgery.
RESULTS
This study included 30 eyes of 25 patients. The preoperative mean IOP was 32.7±1.9 mm Hg (range, 30-36 mm Hg) in group I and 33.2±2.2 mm Hg (range, 30-37 mm Hg) in group II (Table 1). Throughout the follow-up period, IOP was significantly reduced in both groups. After 1y, in group I, the mean IOP was 11.67±0.89 mm Hg while in group II, it was 14.2±4.0 mm Hg (P=0.024; Table 2). A significant correlation between preoperative IOP and postoperative IOP measures was observed in group II at 1, 6, and 12mo, which might be due to intra-surgeon hand variation in suture tightening of the tube and so more reduction of postoperative IOP which could not be standardized. A non-significant correlation between preoperative IOP and postoperative IOP measures that was observed in group I at 1, 6, and 12mo, might be due to less intra-surgeon hand variation with a standard calibration of both tube lumen and suture diameters (Table 3, Figure 3).Hypertensive phase occurred in 1 case (6.67%) in group I after one month (IOP was 24 mm Hg and had declined to 16 mm Hg with alpha agonist and betablocker administration). In group II, 2 cases (13.33%) showed elevated IOP; In Case 1, IOP was 25 mm Hg and declined to 14 mm Hg with alpha agonist and betablocker administration; in Case 2, IOP was 28 mm Hg and declined only to 26 mm Hg with alpha agonist, betablocker and prostaglandin administration. Further investigation of the valve morphology in Case 2 revealed tube occlusion; fibrous tissue was removed and reimplantation of the tube was performed.Complete success was higher in group I (93.3%) than in group II (86.67%).
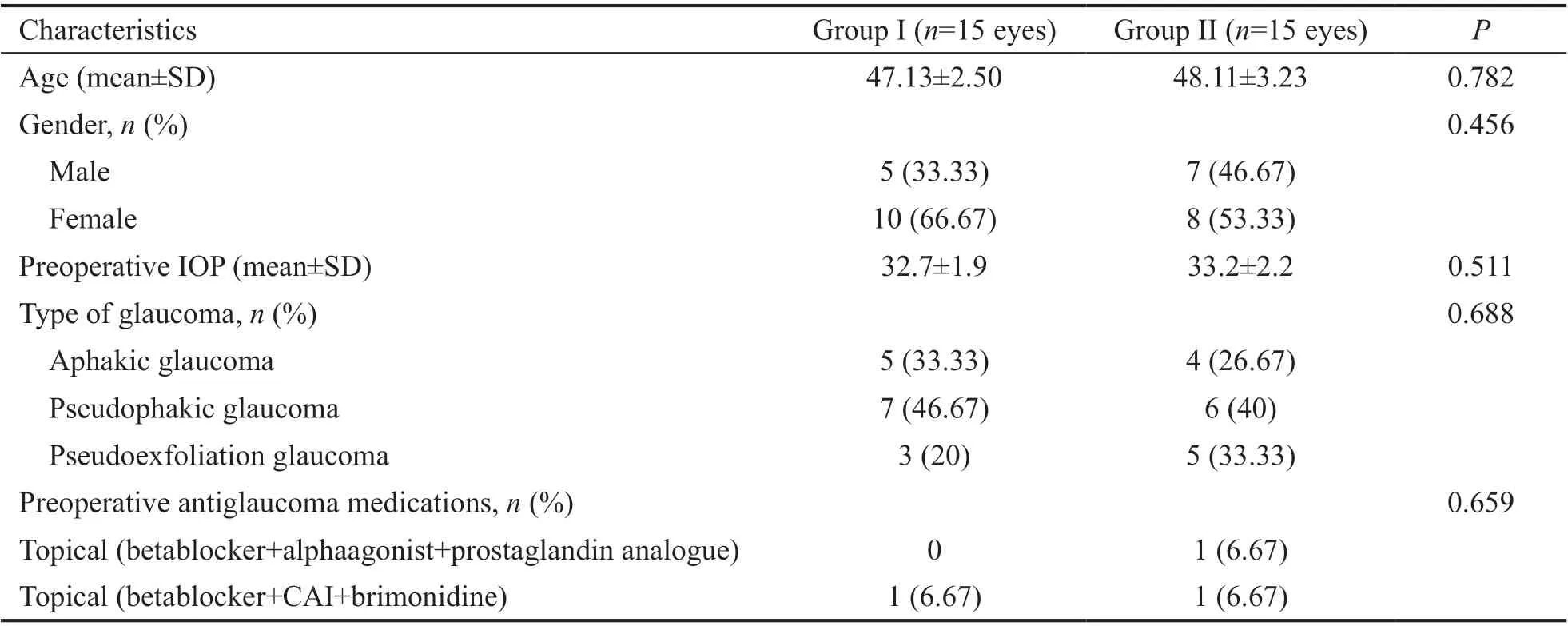
Table 1 Baseline characteristics of the two groups
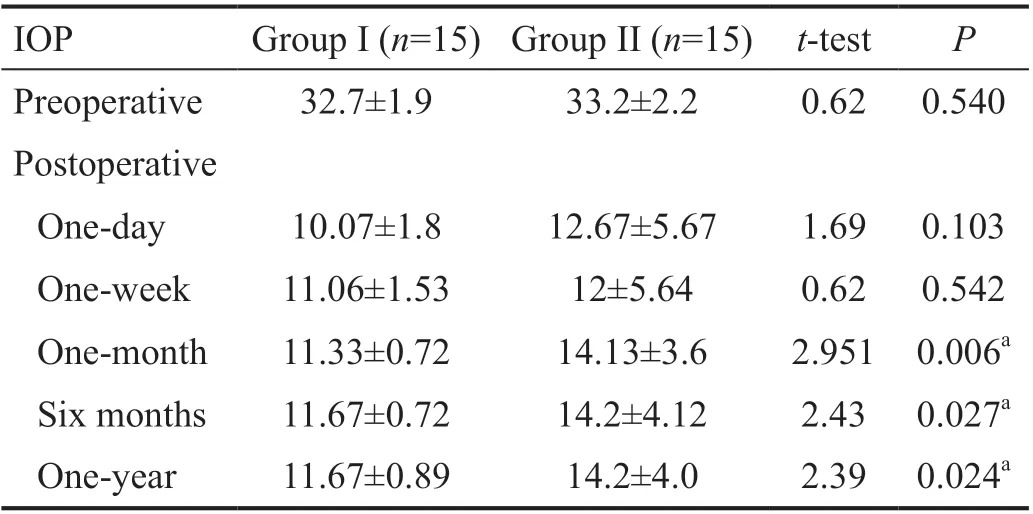
Table 2 Intraocular pressure of the studied groups mm Hg

Table 3 Correlation between preoperative IOP and postoperative follow-up measures of IOP in study groups
Postoperative hypotony occurred in both groups with no significant differences but was more in group II; on postoperative day 1, 2 cases of hypotony (13.33%) were encountered in group II. One case improved with steroid medications and cycloplegic eye drop after 2wk while the other case showed choroidal detachment and persistent hypotony. This case improved after 2mo of treatment. In group I, hypotony only occurred in 1 case (6.67%) on postoperative day 1, which improved 1wk later with steroid medications and cycloplegic eye drops. A shallow anterior chamber was seen in 1 case in group I and 2 cases in group II that were associated with hypotony and improved after 2d of topical steroid and cycloplegic eye drop administration. Hyphema occurred in 4 cases in group II (26.67%) while it occurred in only one case in group I (6.67%; Table 4). There were minimal changes as regarding best corrected visual acuity (BCVA) and VF. Two cases only showed reduction in postoperative BCVA after 1y(13.3%), one case showed a decline of one line in Snellen E chart and deteriorated VF; while the other case of choroidal detachment showed a decline of two lines in Snellen E chart.
DISCUSSION
AGV has a flow-restricting system; moreover, early postoperative hypotony is frequently seen after AGV implantation.Hypotony results from valve failure or aqueous leak around the tube opening site in the early postoperative phase and tube occlusion by ligation or stenting may be required to treat it[7,12]. This study aimed to evaluate the efficacy of applying external ligation or internal stenting in increasing the success rate of AGV and preventing transient or persistent hypotony that occur with AGV. Hypotony after AGV occurs due to valve mechanisms like over-priming of the tube and excessive manipulation of the valve housing; the outflow of aqueous humor around the silicone tube after utilization of a 22 or 23G needle to create the sclerostomy and ciliary body functionfailure are other complications associated with AGV[11-12].
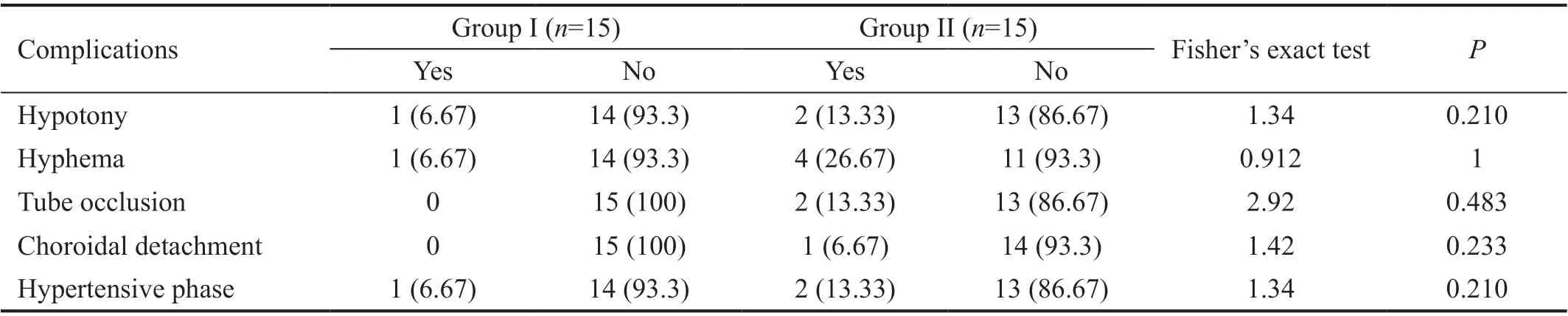
Table 4 Postoperative complications of the studied groups n (%)
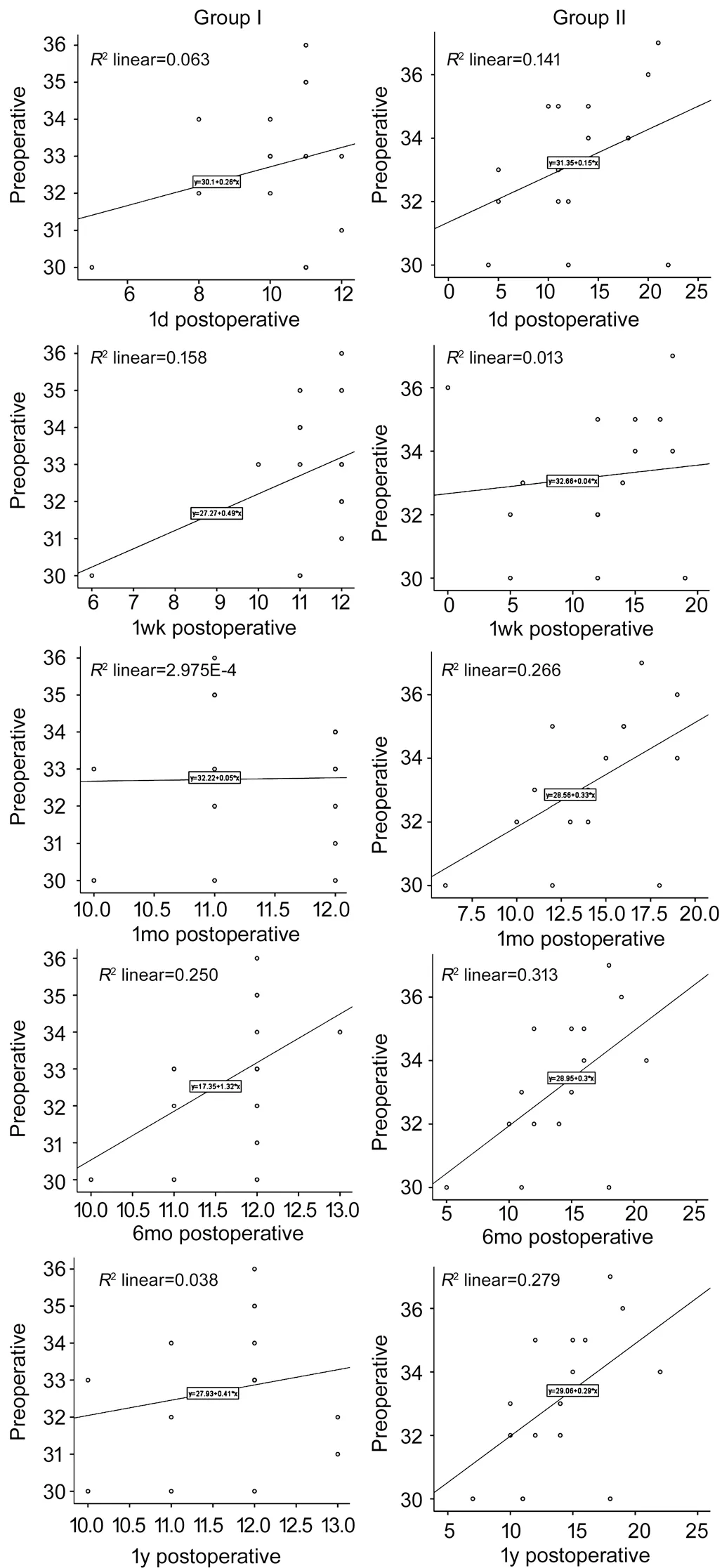
Figure 3 There was no significant correlation between pre- and postoperative IOP measure in group I while in group II there was significant positive correlation between pre- and postoperative IOP measures (at 1, 6mo, and 1y).
This study analyzes the role of ligation and stenting in decreasing the incidence of postoperative hypotony; the occurrence of which was low when compared with other studies that reported the “hypotensive” phase to have occurred in 13% and 15% of patients. Choroidal effusion may also be present. In these cases, hypotony resolves spontaneously as encapsulation of the plate increases outflow resistance within days or weeks from the surgery[10]. This study provided better results than a previous retrospective study that included a total of 20 eyes and followed for the patients for at least 1y.Conventional AGV (CAGV) surgery was performed in 12 eyes, while Ologen-augmented AGV (OAGV) implantation was performed in 8 eyes. Complete success was significantly higher in the OAGV group (50.0%) than in the CAGV group(8.3%). No significant differences were reported regarding qualified success, early hypertensive phase incidence, or changes in IOP within 1y postoperatively[15].
The present study reported lower occurrence of complications associated with CAGV surgery than those seen in previous literature, such as hypotony (0-9%), tube exposure (2%-14.3%),corneal complications (9%-27%), and endophthalmitis (0.8%-6.3%)[16]. The results of the current study were similar to that of a previous study, which showed that, at 12mo postoperatively,mean IOP reduced from 37.1±9.7 to 15.2±5.6 mm Hg. Qualified success occurred in 84.2% of the cases; hypotony was seen in 8.4% of patients and did not require surgical intervention.No suprachoroidal hemorrhage occurred in the study and hyphema was observed in 17.9% of patients[17]. Another study analyzed the role of intraluminal stenting with 4-0 Prolene in management of early postoperative hypotony; in this study,IOP rose from 7 to 10 mm Hg, BCVA improved to 20/30, and choroidal folds were resolved. IOP and BCVA remained stable throughout the 1y follow-up period, and patients did not require additional pharmacological or surgical interventions[18].Similar results were observed in a Korean study carried out in 32 eyes divided into two groups to understand the role of partial ligation. It revealed that in the partial-ligation group,62.5% of the patients had successful IOP control without any additional medical treatment, whereas IOP in the non-ligation group was controlled with or without medical treatment in 56.37% of the patients. Early postoperative hypotony occurred in 6.3% of the patients in the partial ligation group and in 25%in the non-ligation group. The final results showed a nonsignificant difference in the success rate of the partial ligation and non-ligation groups[19].
Additionally, the modifications that were added to AGV surgery in this study were useful in decreasing the rate of hypertensive phase occurrence with no encapsulation, which usually occurs in the first 2mo following CAGV surgery and results in optic nerve dysfunction. This might be related to the reduction in aqueous outflow that probably occurred after tube ligation or stenting. These results are similar to that of another study that decreased the rate of aqueous outflow by using aqueous suppressant medication and studied its effect in limiting the occurrence of hypertensive phase[20].
The relatively small sample size and short-term followup were the main limitations. These techniques require substantial experience in performing CAGV surgery. The low cost, reduced operating time, and ease of performing in addition to the low rate of postoperative hypertensive phase occurrence of AGV surgery are the main strength. Future work on a large sample in association with long term follow up to detect the degree of effectiveness and in decreasing the rate of postoperative hypotony either transient or permanent especially for the beginners is available. In the future, studies comparing efficacy of these surgical modifications and postoperative aqueous suppressants on reducing the occurrence of hypertensive phase should be conducted.
In conclusion, intraluminal stenting or external ligation seems to be effective when used in AGV surgery to prevent transient and persistent hypotony that usually occur with CAGV surgery,in addition to a benefit in lowering the rate of hypertensive phase that mostly related to aqueous outflow reduction. They provide good surgical outcomes with limited complications.
ACKNOWLEDGEMENTS
Conflicts of Interest:Abd Elfattah D, None; Wagdy F,None; Mokbel T, None; Elsorogy H, None; Elhesy A, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
- Vitreous function and intervention of it with vitrectomy and other modalities
