Patent hemostasis of radial artery:Comparison of two methods
Vassileios Kyriakopoulos,Andrew Xanthopoulos,Michail Papamichalis,Spyridon Skoularigkis,Chara Tzavara,Emmanouil Papadakis,Sotirios Patsilinakos,Filippos Triposkiadis,John Skoularigis
Vassileios Kyriakopoulos,Emmanouil Papadakis,Sotirios Patsilinakos,Department of Cardiology,Konstantopoulio General Hospital,Athens 14233,Greece
Andrew Xanthopoulos,Michail Papamichalis,Spyridon Skoularigkis,Filippos Triposkiadis,John Skoularigis,Department of Cardiology,University Hospital of Larissa,Larissa 41110,Greece
Chara Tzavara,Department of Health,Medical School,University of Athens,Athens 11527,Greece
Abstract BACKGROUND Radial artery obstruction is the most common complication of coronary angiography performed via transradial access.Patent hemostasis can significantly reduce the risk of radial artery occlusion.Previous studies utilized sophisticated methods to evaluate radial artery patency.Simplified and easily applicable methods for successful patent hemostasis are currently lacking.AIM To determine which method (pulse oximeter vs the traditional radial artery palpation) is better to achieve patent hemostasis.METHODS This prospective,single center study included 299 consecutive patients who underwent coronary angiography or percutaneous coronary intervention between November 2017 and July 2019.Patients less than 18 years old,with a history of radial artery disease,or no palpable artery pulse were excluded from the study.Patients were randomly assigned to two groups.In the first group,radial artery flow was assessed by palpation of the artery during hemostasis (traditional method).In the second group,radial artery patency was estimated with the use of a pulse oximeter.Two different compression devices were used for hemostasis(air chamber and pressure valve).The primary study endpoint was the achievement of successful patent hemostasis.RESULTS The two groups (pulse oximeter vs artery palpation) had no significant differences in age,sex,body mass index,risk factors,or comorbidities except for supraventricular arrhythmias.The percentage of patients with successful patent hemostasis was significantly higher in the pulse oximeter group (82.2% vs 68.1%,P=0.005).A lower percentage of patients with spasm was recorded in the pulse oximeter group (9.9% vs 19.0%,P=0.024).The incidence of local complications,edema,bleeding,hematoma,vagotonia,or pain did not differ between the two groups.In the multivariate analysis,the use of a pulse oximeter (OR:2.35,95%CI:1.34-4.13,P=0.003) and advanced age (OR:1.04,95%CI:1.01-1.07,P=0.006),were independently associated with an increased probability of successful patent hemostasis.The type of hemostatic device did not affect patent hemostasis (P=0.450).CONCLUSION Patent hemostasis with the use of pulse oximeter is a simple,efficient,and safe method that is worthy of further investigation.Larger randomized studies are required to consider its clinical implications.
Key Words:Radial access;Patent hemostasis;Palpation;Oximeter;Coronary angiography;Radial artery occlusion
INTRODUCTION
Transradial access is increasingly used in coronary angiographyvstransfemoral access as it has several advantages.Transradial access is associated with fewer vascular complications,lower bleeding complications,and reduced mortality in specific highrisk populations[1].Furthermore,the technique offers earlier mobilization after the procedure,and the patient usually has a shorter hospital stay.The European guidelines for coronary angiography in patients with acute coronary syndrome favor transradial over transfemoral access with a Class IA indication[2,3].
Radial artery obstruction (RAO) is a frequent complication of coronary angiography performedviatransradial access[4].RAO may prevent radial artery access for future coronary angiography or as a conduit for coronary artery bypass grafting.At the same time,patients requiring hemodialysis lose an artery that can be used to create an arteriovenous fistula.Therefore,prevention of RAO is of particular clinical importance in patients undergoing coronary angiographyviatransradial access.Experts emphasize the need for the adoption of novel techniques that may reduce the incidence of RAO to less than 5%[5].
Complete obstruction of blood flow in the radial artery during hemostasis is a strong predictor of RAO occurrence[6].On the contrary,maintaining circulatory anterograde flow in the radial artery during hemostasis,known as patent or nonobstructive hemostasis,reduces the risk of RAO[7,8].Various methods of patent hemostasis have been described,but there is no current consensus on the optimal method.Of note,the application of nonobstructive hemostasis is technically difficult as it requires intense staff mobilization,multiple evaluations of radial artery blood flow,and adjustment of hemostatic pressure in order to maintain patency.That is why patent hemostasis is not fully adopted in most laboratories[9].The goal of this study was to evaluate a simplified and easily applicable method to achieve patent hemostasis in patients undergoing diagnostic coronary angiography or percutaneous coronary intervention (PCI).
MATERIALS AND METHODS
Patient population
A total of 299 consecutive patients undergoing cardiac catheterization between November 2017 and July 2019 and considered eligible for radial access were included in the study.Patients underwent a Barbeau test precatheterization,to assess collateral palmar arch sufficiency.Patients were randomly assigned to two groups.In the first group,radial artery flow was assessed by artery pulse palpation during hemostasis(traditional method).In the second group,radial artery patency was estimated with the use of a pulse oximeter.Two different compression devices were used for hemostasis,one with an air chamber and another with a pressure valve.The primary study endpoint was the achievement of successful patent hemostasis.
Randomization did not affect coronary angiography,either diagnostic or invasive,and operators were unaware of the patient allocation.RAO was assessed at 24 h and 30 d after the procedure.Patients younger than 18 years of age with a history of radial artery disease or absence of radial artery pulse were excluded from the study.Patients participating in the study provided written informed consent,and the study protocol was approved by the hospital’s ethics review board.
Transradial catheterization procedure
Radial artery catheterization was performed using the Seldinger technique.The catheter diameter was 5/6-French.
Conventional hemostasis with radial artery pulse palpation
The introducer sheath was removed immediately after the procedure.The sheath was pulled out by 4 to 5 cm and a hemostatic bandage was applied around the wrist.The bandage was then tightened and the catheter was removed.In group 1,radial artery patency was assessed by radial artery pulse palpation.The bandage remained in place for 4 h and then was slowly removed.A light dressing was applied at the entry site after the procedure.
Patent hemostasis procedure with the aid of pulse oximeter
The sheath was pulled out by 4 to 5 cm and a hemostatic bandage was applied over the entry site.In group 2 a pulse oximeter sensor was placed on the index finger,the bandage was tightened,and the sheath was removed.The ulnar artery was compressed and the hemostatic bandage gradually began to relax.Radial artery patency was confirmed by plethysmographic signal reoccurrence.In case of bleeding before plethysmographic signal appearance,the hemostatic bandage compression was increased.If radial artery flow was confirmed by the oximeter and no bleeding complications occurred,then a bandage remained in place for 4 h.Radial artery patency was assessed on an hourly basis.
Assessment of radial artery patency
Radial artery flow was evaluated with a Barbeau test.The pulse oximeter sensor was placed on the index finger and the plethysmographic signal was observed.Ulnar and radial artery compression led to signal loss.Radial artery pressure was then removed while maintaining ulnar artery compression.Appearance of the plethysmographic signal was proof of radial artery patency,while absence of a signal indicated RAO.The test was performed precatheterization,at 24 h and at 30 d after coronary angiography.Radial artery patency was also assessed at 30 d by vascular ultrasonography with Doppler assessment.
Hemostatic efficacy
Hemorrhagic complications that resulted in blood loss from the puncture site and judged capable of causing hemodynamic instability,blood transfusion,or death were regarded as significant.Hematomas at the puncture site were considered clinically significant when their diameter exceeded 3 cm.
Statistical analysis
Quantitative variables were expressed as means ± SD or as medians and interquartile range (IQR).Qualitative variables were reported with absolute and relative frequencies.Chi-square and Fisher’s exact tests were used to compare proportions.Student’st-tests were used to compare mean values that were normally distributed.Mann-Whitney tests were used to compare median values when the distribution was not normal.Logistic regression analyses in a stepwise method (Pfor entry 0.05,Pfor removal 0.10) were performed in order to identify factors associated with the presence of specific outcomes.Unadjusted and adjusted odds ratios with 95%CI were computed from the results of the logistic regression analyses.Statistical significance was set at 0.05.The analyses were conducted using SPSS statistical software (version 22.0).
RESULTS
Demographic characteristics and risk factors/comorbidities
Radial artery patency during hemostasis was assessed by artery palpation (control group) in 147 patients (49.2%) and by pulse oximeter sensor in 152 patients (50.8%).The demographic characteristics of the study population are shown in Table 1.The study population consisted mainly of men (75%) with a mean age of 60.8 years.Dyslipidemia was the most common comorbidity followed by hypertension,coronary artery disease,and diabetes mellitus.One out of three patients (35%) had previously undergone PCIs and 6% had previously undergone coronary bypass surgery.The two groups of patients did not have significant differences in their baseline clinical characteristics (Table 1).Patients in the control group had a higher rate of supraventricular arrhythmia,mainly atrial fibrillation (26.5%vs13.2%,P=0.004).
Procedural characteristics
Table 2 shows the procedural characteristics of the two study groups.PCI was performed in 30% of the patients.There were no differences in the number of coronary vessels that received intervention.Half the patients underwent coronary angiography using a 5-french introducer sheath and the other half using a 6-french sheath.The two groups of patients did not differ in several other procedural characteristics (e.g.,right or left hand,duration of procedure,radiation time).Patients received similar doses of anticoagulants (heparin) and did not differ in the type of device used for hemostasis(Table 2).
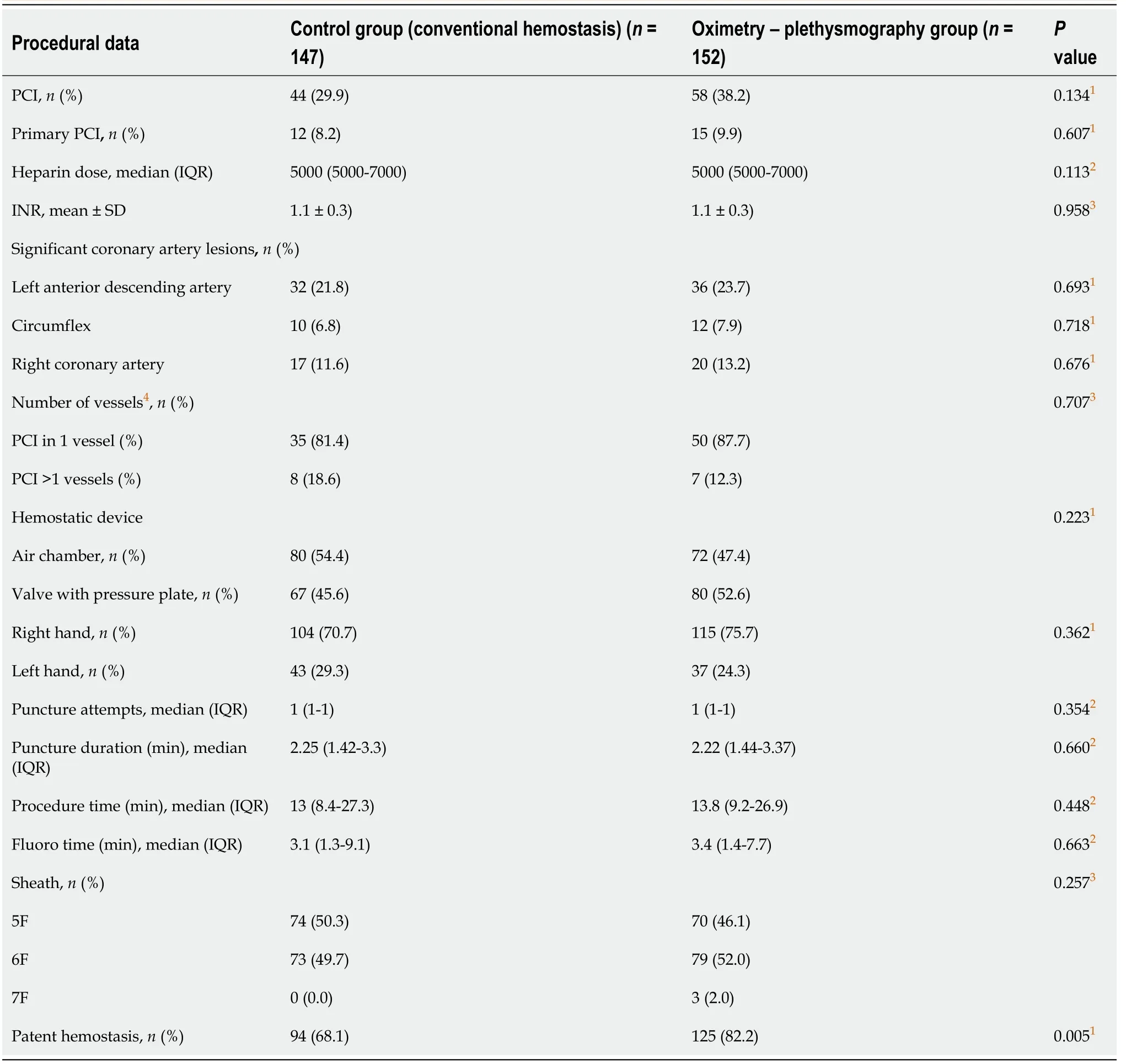
Table 2 Procedural data of the study population
Complications
Table 3 shows the coronary angiography complications.The group of patients in whom the radial artery patency was assessed with the traditional method (artery palpation) had a higher rate of radial artery spasm (P=0.024).The two groups had similar rates of vagotonia,hematoma,bleeding,edema,local complications,and pain.
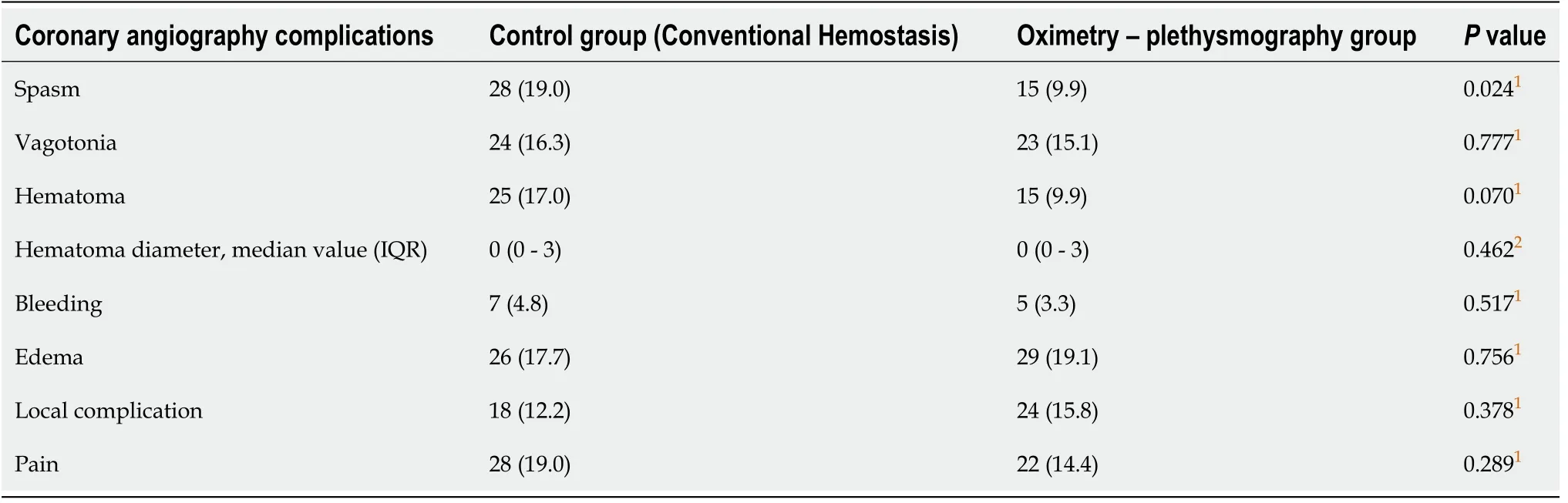
Table 3 Coronary angiography compIications between two hemostatic methods
Patent hemostasis in the study groups
The group of patients whose radial artery patency was assessed using the pulse oximeter achieved significantly higher rates of patent hemostasis than those in the control group,using radial artery palpation (82.2%vs68.1%,P=0.005;Figure 1).The type of hemostatic device (air chamber or pressure valve device) did not affect patent hemostasis (P=0.450).Radial artery flow was restored in a significant percentage of patients at 24 h and at 30 d after coronary angiography (Table 4).
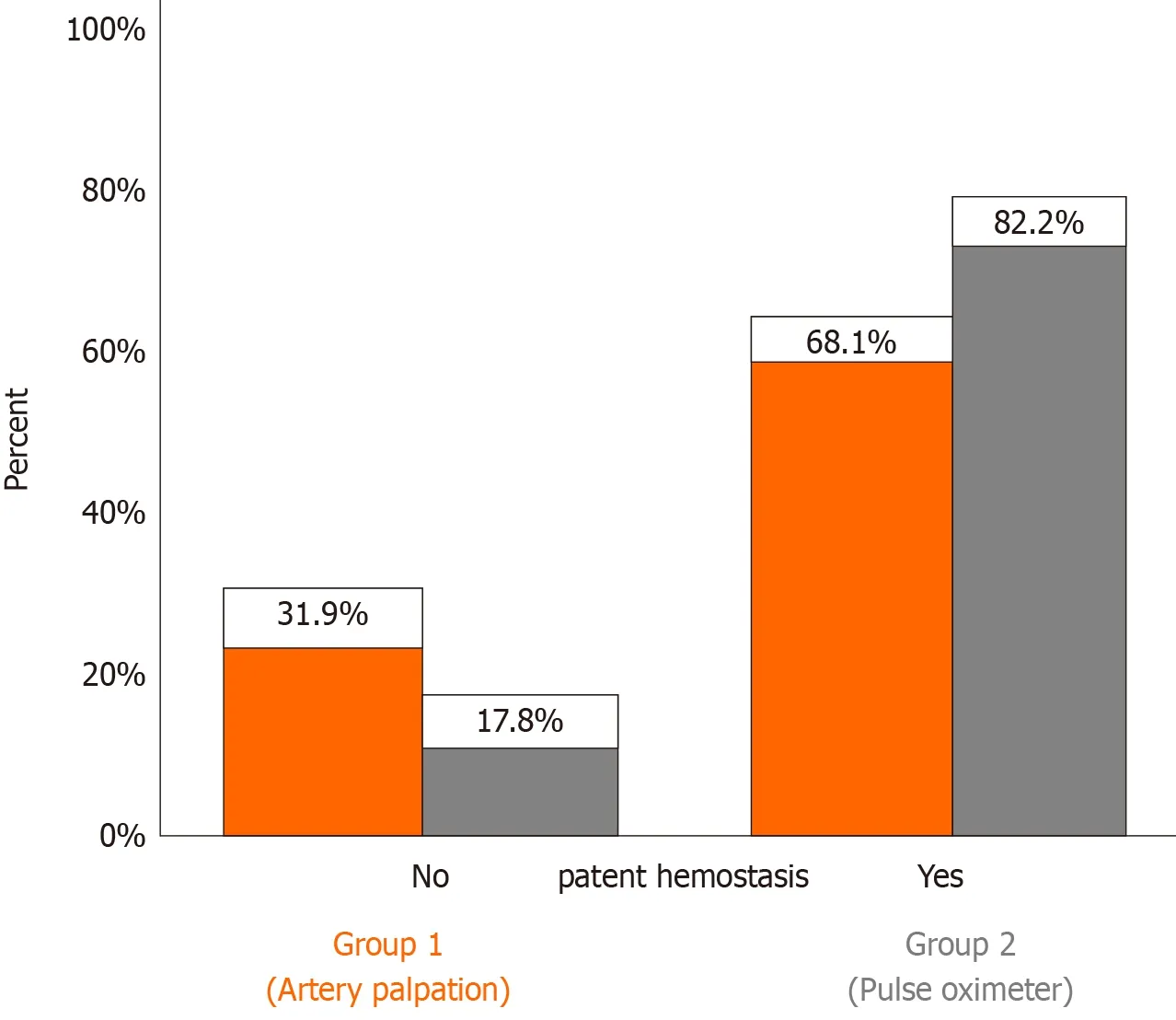
Figure 1 Percentage of patent hemostasis in each study group.
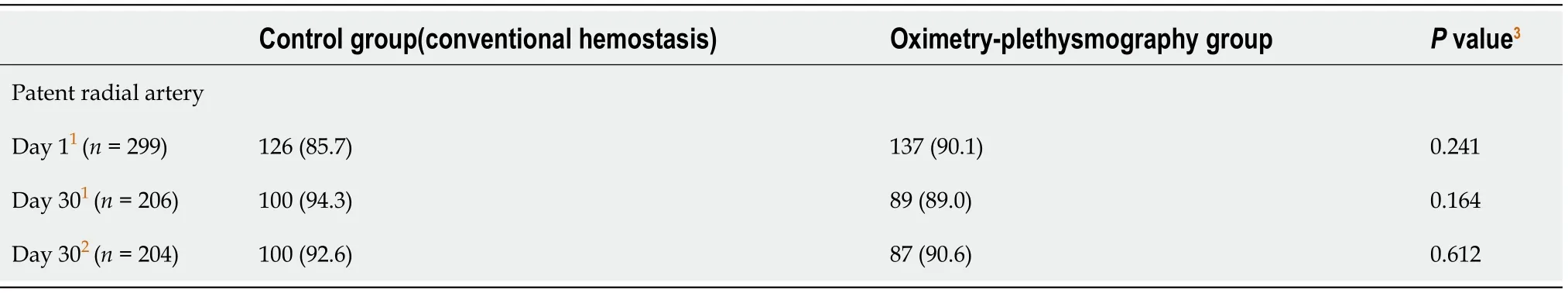
Table 4 Patent radiaI artery by patient group
Predictors of patent hemostasis
Multivariate logistic regression analysis revealed that pulse oximeter use (OR:2.35,95%CI:1.34-4.13,P=0.003) and patient age (per 1 year increase;OR:1.04,95%CI:1.01-1.07,P=0.006) as independent predictors of patent hemostasis (Table 5).
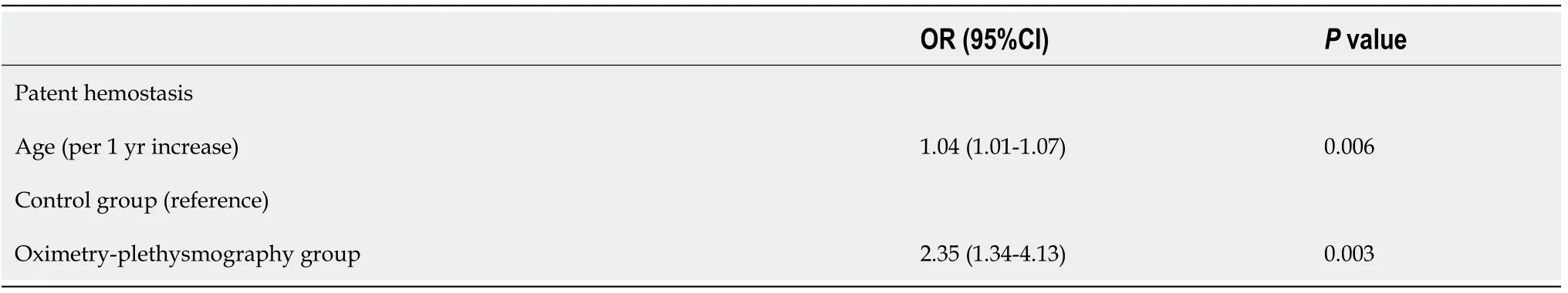
Table 5 Predictors of patent hemostasis
DISCUSSION
The main study findings were:(1) Successful patent hemostasis was significantly more frequent in the pulse oximeter groupvsthe radial artery palpation group;(2) A lower percentage of complications (i.e.spasm) was recorded in the pulse oximeter group;and (3) Advanced age and the use of a pulse oximeter were independent predictors of successful patent hemostasis.
Many studies have reported the safety and efficacy of performing coronary angiographyviathe transradial access.Transradial access is preferred over transfemoral artery access for percutaneous diagnostic and interventional procedures because it is associated with lower rates of vascular and hemorrhagic complications that lead to transfusions[5,10-12].A systematic review and meta-analysis including 11707 patients who presented with ST-segment elevation myocardial infarction,reported an association between transradial access and reduction in 30-d mortality(relative risk,0.72),major bleeding (relative risk,0.60),and access-site complications(relative risk,0.40) compared with transfemoral access[11].Interestingly,the transradial approach has the advantage of a rapid interval to patient mobilization[13].
RAO is a potential complication of coronary angiography using the transradial approach[5,10].In randomized trials,RAO incidence ranged up to 10%[5].However,in daily clinical practice RAO frequency is much higher[4,14-16].Radial artery patency should be routinely checked before discharge of any patient who has undergone coronary angiographyviatransradial access[5].Radial artery palpation is the most common technique used[17].However,artery palpation may be misleading as the presence of collateral circulation from palmar arches in the upper extremity is likely to lead to a palpable pulse from the distal stump even in the presence of RAO[5].RAO is more common at the end of hemostasis and thereafter gradually decreases in the first 24 h and even further in the 30 d after the procedure.In a meta-analysis of 112 studies including 46.631 patients,late revascularization occurred in a significant proportion of patients with RAO[18].In this study,radial artery flow was restored in a significant percentage of patients at 24 h and at 30 d after coronary angiography.
Measures to reduce RAO incidence include smaller catheters,adequate anticoagulation,the adoption of patent hemostasis strategies with or without ulnar artery compression,and the reduction of hemostasis time to ≤ 120 min[5,16,18-24].Patent hemostasis is the technique of maintaining radial artery forward flow through guided artery compression during hemostasis after coronary angiography[7].In patients undergoing coronary angiography,complete absence of radial artery flow during hemostatic compression is a strong predictor of RAO[6,24].On the contrary,maintaining radial artery antegrade flow during hemostasis,known as patent or nonocclusive hemostasis,is an important factor in preventing RAO,but its complexity has limited adoption[5,7,25].Maintaining radial artery antegrade flow during hemostatic compression constitutes part of the recommended best practice after transradial access for coronary angiography[25].
The best technique to achieve patent hemostasis is a subject of ongoing research.Previous studies utilized relatively sophisticated methods to evaluate radial artery patency.In the landmark prevention of radial artery occlusion-patent hemostasis evaluation trial (the PROPHET study),436 patients were randomized to undergo either conventional hemostasis or patent hemostasis after diagnostic coronary angiographyviathe transradial approach.Twelve percent of patients who underwent conventional hemostasis experienced RAO at 24 h.The corresponding rate for patients in the patent hemostasis group was 5%[7].The use of an oximetry-plethysmography test was the strongest predictor of achieving patent hemostasis.In the prophylactic hyperperfusion evaluation trial (PROPHET-II),ipsilateral ulnar artery compression during radial artery hemostatic compression increased the rate of patent hemostasis and reduced the incidence of RAO from 3.0% to 0.9%[25].In the randomized radial compression guided by mean artery pressurevsstandard compression with a pneumatic device (RACOMAP) trial,a significant reduction in RAO rates from 12.0%to 1.1% was observed in patients following the patent hemostasis protocol compared with traditional arterial obstructive compression[8].In the RACOMAP trial,nonobstructive hemostasis was performed by compressing the radial artery during hemostasis,guided by the mean blood pressure[8].
In a study by Edriset al[26],patent hemostasis was achieved with rapid deflation of the compression band.The technique increased patent hemostasis rates from 40% to 95% and reduced RAO rates from 14.9% to 2.0% without bleeding complications.A study comparing nonobstructive hemostasis to conventional hemostasis reported reduced RAO at 24 h in the patent hemostasis group,whereas the difference at 7 d between the two groups was not statistically significant[27].The result is similar to that observed in this study in which RAO rates at 30 d did not differ between the two groups.The rates of patent hemostasis in this study are similar to those in previous studies (68.1% to 82.2%)[7,24].Furthermore,in previous studies,nonocclusive hemostasis did not increase bleeding complications compared with conventional hemostasis[7,8].Plethysmographic evaluation of radial artery flow allows easier achievement of patent hemostasis without adversely affecting the method safety.Similarly,in the present study,no difference was observed in the hemorrhagic events that occurred in the two treatment groups.Interestingly,in the current study,manual compression was not required to achieve hemostasis in the pulse oximeter group.In the PROPHET study manual compression was required in a small percentage of patients (3.6%) to achieve hemostasis[7].Lastly,the rates of spasm in our study,which were lower in the oximetervsthe artery palpation group,were in accord with those reported in the literature[4].
In this study,we observed an association between increased age and successful patent hemostasis.Several speculations can be made regarding that finding.Firstly,radial artery spasm is more frequent in younger than in older patients undergoing PCIviaradial access and therefore older adults are more likely to have a successful patent hemostasis[28-31].Secondly,increased arterial stiffness in elderly patients produces a steeper increase in radial artery flow,resulting in reopening of the occlusion in the early period and maintaining vessel patency in the long-term[32].Lastly,increased arterial stiffness in older patients may preclude the total interruption of flow during manual compression and therefore facilitate patent hemostasis[32].
The current study has several limitations that need to be addressed.Firstly,the study population was not large,but it was comparable to previous studies in the field.Secondly,at 30 d,radial artery patency was assessed with duplex ultrasonography in 204 out of 299 patients.We performed a telephone follow-up of the patients who did not return at 30 d.The three main reasons cited for follow-up interruptions were lack of understanding regarding the necessity of follow-up,social reasons (e.g.,distant hometown,financial barriers,relocation) and unawareness of the appointment schedule.Nevertheless,radial artery flow was restored in a significant percentage of patients who presented at follow-up,which is in accord with the current literature.Thirdly,patent hemostasis achieved in the current study by the use of pulse oximetry is relatively more simple than the techniques described in previous studies,and can be more widely implemented in everyday clinical practice.
CONCLUSION
Oximetry-plethysmography is an efficient and safe method to achieve patent hemostasis after coronary angiographyviatransradial access.Larger randomized control trials are urgently needed.
ARTICLE HIGHLIGHTS
Research background
Radial artery obstruction is a frequent complication of coronary angiography performed via transradial access.Maintaining circulatory anterograde flow in the radial artery during hemostasis (patent or nonobstructive hemostasis) reduces the risk of radial artery obstruction.
Research motivation
Simplified and easily applicable methods for successful patent hemostasis are currently lacking.
Research objectives
To determine which method,pulse oximeter vs the traditional radial artery palpation,is better to achieve patent hemostasis.
Research methods
This a prospective,single center study included 299 consecutive patients who underwent coronary angiography or percutaneous coronary intervention between November 2017 and July 2019.The exclusion criteria were:(1) Age of < 18 years;(2)History of radial artery disease;and (3) No palpable arterial pulse.Patients were randomly assigned to two groups.In the first group,radial artery flow was assessed by palpation of the artery during hemostasis (traditional method).In the second group,radial artery patency was estimated with a pulse oximeter.Two different compression devices were used for hemostasis (air chamber and pressure valve).The primary study endpoint was the successful achievement of patent hemostasis.
Research results
The two groups (pulse oximeter vs artery palpation) had no significant differences in age,sex,body mass index,risk factors,or comorbidities except for supraventricular arrhythmias.The percentage of patients with successful patent hemostasis was significantly higher in the pulse oximeter group (82.2% vs 68.1%,P=0.005).A lower percentage of patients with spasm was recorded in the pulse oximeter group (9.9% vs 19.0%,P=0.024).Multivariate analysis found that the use of pulse oximeter (OR:2.35,95%CI:1.34-4.13,P=0.003) and advanced age (OR:1.04,95%CI:1.01-1.07,P=0.006),were independently associated with an increased probability of successful patent hemostasis.The type of hemostatic device did not affect patent hemostasis (P=0.450).
Research conclusions
Patent hemostasis with the use of pulse oximeter is a simple,efficient,and safe method,and is worthy of further investigation.
Research perspectives
Larger randomized studies are required to consider its clinical implications.
 World Journal of Cardiology2021年10期
World Journal of Cardiology2021年10期
- World Journal of Cardiology的其它文章
- Cardiac involvement in hydrocarbon inhalant toxicity—role of cardiac magnetic resonance imaging:A case report
- Cardiovascular efficacy and safety of dipeptidyl peptidase-4 inhibitors:A meta-analysis of cardiovascular outcome trials
- Elderly patients with non-cardiac admissions and elevated highsensitivity troponin:the prognostic value of renal function
- Coronavirus and cardiovascular manifestations- getting to the heart of the matter
- Artificial intelligence and machine learning in cardiovascular computed tomography
- Electrocardiographic changes in Emphysema
