Literature review of the outcome of and methods used to improve transperineal repair of rectocele
Mohammad Fathy,Ahmed Hossam Elfallal,Sameh Hany Emile
Mohammad Fathy,Ahmed Hossam Elfallal,Sameh Hany Emile,General Surgery,Mansoura University Faculty of Medicine,Mansoura 35516,Egypt
Abstract BACKGROUND Rectocele is commonly seen in parous women and sometimes associated with symptoms of obstructed defecation syndrome (ODS).AIM To assess the current literature in regard to the outcome of the classical transperineal repair (TPR) of rectocele and its technical modifications.METHODS An organized literature search for studies that assessed the outcome of TPR of rectocele was performed.PubMed/Medline and Google Scholar were queried in the period of January 1991 through December 2020.The main outcome measures were improvement in ODS symptoms,improvement in sexual functions and continence,changes in manometric parameters,and quality of life.RESULTS After screening of 306 studies,24 articles were found eligible for inclusion to the review.Nine studies (301 patients) assessed the classical TPR of rectocele.The median rate of postoperative improvement in ODS symptoms was 72.7% (range,45.8%-83.3%) and reduction in rectocele size ranged from 41.4%-95.0%.Modifications of the classical repair entailed omission of levatorplasty,addition of implant,concomitant lateral internal sphincterotomy,changing the direction of plication of rectovaginal septum,and site-specific repair.CONCLUSION The transperineal repair of rectocele is associated with satisfactory,yet variable,improvement in ODS symptoms with parallel increase in quality-of-life score.Several modifications of the classical TPR were described.These modifications include omission of levatorplasty,insertion of implants,performing lateral sphincterotomy,changing the direction of classical plication,and site-specific repair.The indications for these modifications are not yet fully clear and need further prospective studies to help tailor the technique to rectocele patients.
Key Words:Transperineal repair;Rectocele;Review;Modifications;Outcome
INTRODUCTION
Anatomic background
Rectocele is a variant of pelvic organ prolapse (POP) that is defined as the herniation of the rectum into the posterior vaginal lumen through a weakness or defect of the rectovaginal septum (RVS)[1].The RVS is the connective tissue fascia that separates the genital system from the digestive tract[2].It is more firmly adherent and closely attached to the vagina than to the anorectum[3].The thickness of the RVS varies from 0.1 mm to 2.6 mm,being thicker medially and looser and more adipose laterally[4].
Incidence and pathogenesis
Rectocele affects nearly two-thirds of parous women at variable degrees that may or may not be associated with symptoms[3].A recent study suggested a strong association between vaginal delivery,namely the first delivery,and the development of rectocele and its size[5].However,it was reported that nearly 12% of nulliparous women may also develop rectocele secondary to congenital defects[6].
The pathogenesis of rectocele is multifactorial including a variety of modifiable and non-modifiable factors that result in loss of integrity of the RVS and the development of rectocele.Non-modifiable risk factors include advanced age and genetic susceptibility whereas the modifiable risk factors include greater parity,history of vaginal delivery,history of pelvic surgery,obesity,level of education,constipation,and chronic increase in the intra-abdominal pressure[4].
Basically,rectoceles are based on defects in the RVS.According to Diets and Steensma[7],vaginal delivery leads to increased prevalence and size of already present,asymptomatic defects in the RVS.Richardson[8] suggested that the etiology of rectocele may be related to discreet defects in the RVS.The most common form of these defects is a transverse break just above the perineal body.
Further factors that may contribute to the development of rectocele include the loss of natural fixation that impairs the ability of the posterior wall to resist pressures from behind[8].In addition,long-standing denervation of the pelvic floor and widening of the genital hiatus during delivery may worsen the condition[9].Also,the change in orientation of the levator ani muscles,which are important elements in vaginal support,in response to birth trauma can contribute to the pathogenesis of rectocele.It was observed that the levator ani muscles are stretched more than 200% beyond the threshold for stretch injuries during the second stage of labor[10].
Clinical features
Rectocele usually presents with many symptoms that may not be constant and may vary from day to day.These symptoms include pelvic pain or feeling of pressure,feeling of the posterior vaginal bulge,manifestations of obstructed defecation syndrome (ODS),constipation,and dyspareunia[11].Physical examination includes both rectal and vaginal assessment.Rectocele can be graded according to the Baden-Walker system,which measures the distance of the most distal point of the prolapsed wall from the hymen during Valsalva maneuver[12].To ensure better accuracy and reliability,the POP quantification system is used to assess the rectocele with a twopoint assessment method followed by grading[13].
Assessment
Fluoroscopic defecography is usually used for the anatomical assessment of rectocele.It involves the introduction of a contrast medium into the rectum and the assessment of the anatomy and function at rest and during straining using an X-ray machine and a special commode[14].It is worthy to note that up to 93% of healthy,asymptomatic women were found to have a radiologic evidence of rectocele in fluoroscopic defecography.Therefore,the indication for surgical treatment of rectocele should be predominantly based on clinical symptoms and not just the radiologic evidence of an anatomical rectocele.
More superior to X-ray defecography is the dynamic magnetic resonance imaging defecography that can confer more detailed diagnosis and can easily reconstruct the sequence of images into a video to assess the condition more precisely[15].Also,endoanal ultrasonography dynamic scan (echodefecography) and transperineal ultrasonography are used successfully in the assessment of rectocele,perineal body,and anal sphincters[16,17].
Management
Non-surgical management of rectocele involves eating a high-fiber diet,increasing water intake,and stool softeners.In addition,pelvic floor physiotherapy,such as Kegel exercises,is used to improve rectocele symptoms,but they appear to be more successful in anterior compartment prolapse[18].Vaginal pessaries have been used with good results and succeed to avoid surgery in nearly two-third of patients[19].
Surgical management of rectocele is reserved for those who fail to improve after conservative treatment[20].Surgery aims at correcting the anatomy and strengthening the rectal wall as well as correcting any coexisting pathology.Rectocele repair can be achieved through transvaginal,transperineal,transanal,or abdominal approaches.Transvaginal repair is the most common and preferable approach to gynecologists,while transanal and transperineal repairs are the preferable approaches to coloproctologists[3].The transabdominal approach,namely ventral mesh rectopexy,is mainly indicated for high-level rectoceles,rectoceles associated with internal rectal prolapse,and/or descending perinium syndrome,associated genital prolapse,or when transperineal and transvaginal repairs are contraindicated[3,20].
The transperineal approach may have an advantage over the transvaginal and transanal approaches in that it does not involve the vaginal mucosa and does not induce stretching of the anal sphincter muscles and therefore does not compromise sexual functions or the continence mechanism[21].
Classical technique of transperineal repair of rectocele
The procedure is usually done under spinal anesthesia.Patients are placed in the lithotomy position,and the buttocks are separated.A curvilinear incision is made between the anal verge and the posterior fourchette to allow for proper dissection of rectovaginal space anterior to the anal sphincter complex.Using a combination of blunt and sharp dissection,with the help of digital palpation,the separation of vaginal mucosa from the rectal wall is achieved taking care to avoid injury of the vagina and rectum.The dissection is continued until the rectocele bulge is fully exposed.Then,plication of the RVS is performed in a side-to-side manner with interrupted absorbable sutures.The transperineal approach is usually combined with levatorplasty to restore the normal vaginal hiatus.Anal sphincteroplasty can be also performed in case of sphincter defects.After adequate hemostasis,perineorrhaphy is performed,and the skin is closed with interrupted absorbable sutures[22].
MATERIALS AND METHODS
Strategy of literature search
This was a comprehensive literature review in which an organized literature search was completed using the following keywords “rectocele,” “anterior rectocele,”“perineal repair,” “transperineal repair,” “pelvic organ prolapse,” “transperineal approach,” and “rectocele repair.” Eligible studies were identified by searching PubMed/Medline database and Google Scholar in addition to manual search of reference lists of retrieved studies.The search process started from January 1991 through December 2020.
The inclusion criteria comprised prospective or retrospective case series and cohort studies and randomized clinical trials that reported the outcome of classical transperineal rectocele repair and its technical modifications with at least 6 mo of follow-up.We excluded irrelevant studies,studies assessing techniques for rectocele repair other than the transperineal repair,studies that did not report the outcome of transperineal repair clearly,and articles without an English full text.
RESULTS
Literature analysis
The preliminary search yielded 306 articles.After duplicates subtraction,264 articles were initially screened.After screening,we excluded irrelevant studies,other study types (review articles,case reports,letters,and conferences papers),and articles in languages other than English,and finally 24 studies were eligible for analysis.The studies included were 13 retrospective studies,7 prospective studies,and 4 randomized trials.The literature search and study selection process are outlined in Figure 1.
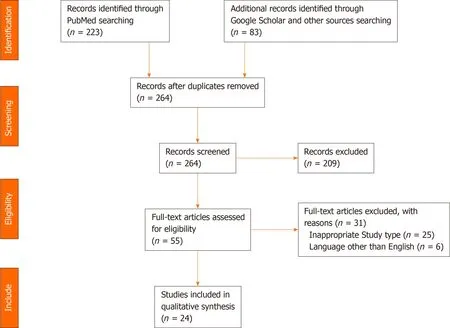
Figure 1 PRISMA diagram outlining study selection process.
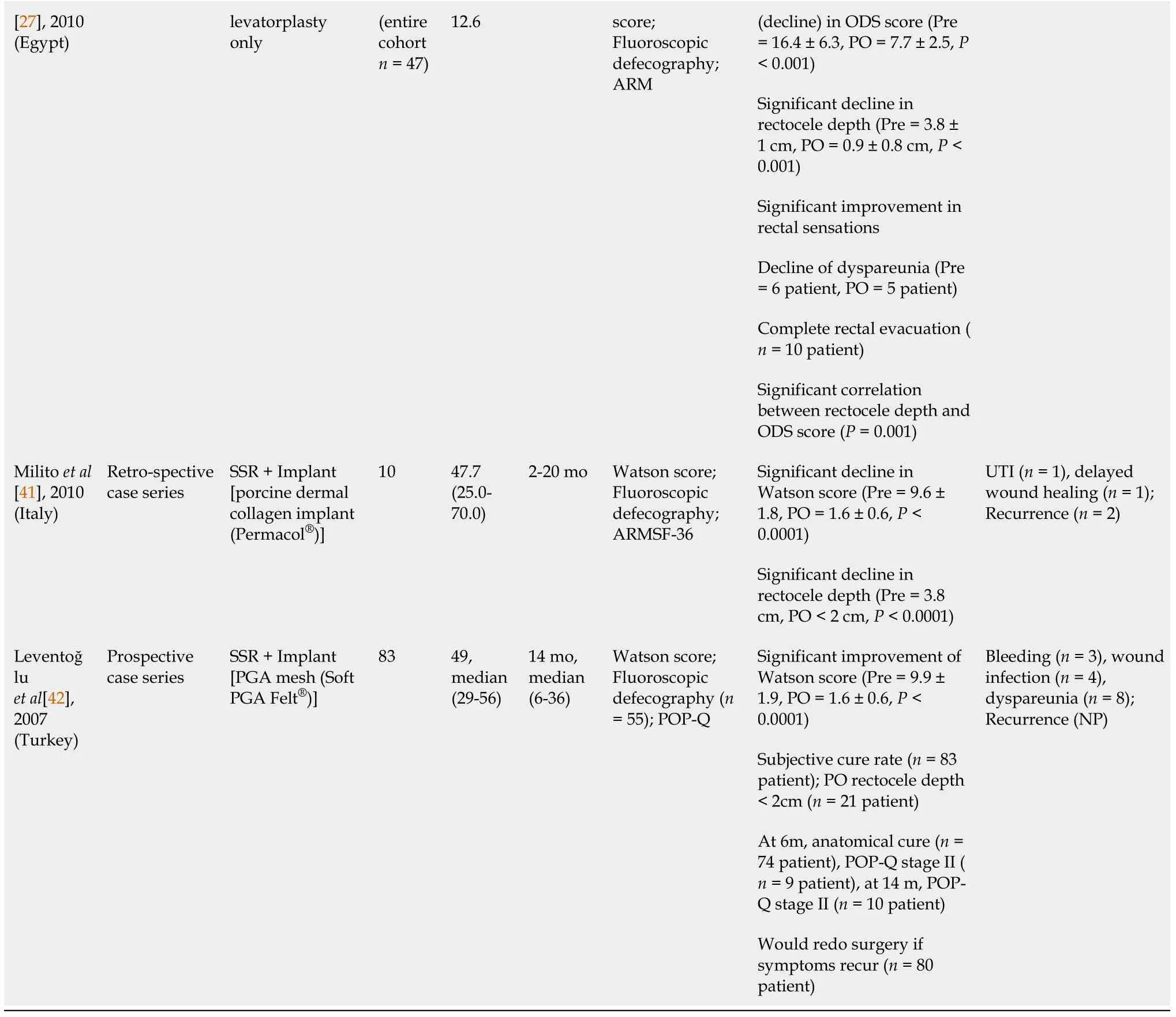
The 24 studies included 1349 patients,821 (60.9%) of whom underwent TPR of rectocele,either using the classic repair or modified repair techniques as shown in Figure 2.
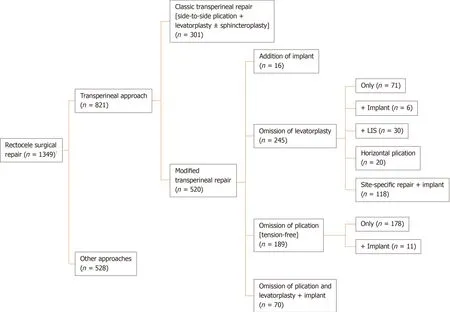
Figure 2 Diagram illustrating different techniques of transperineal repair assessed in the studies reviewed .
Classical transperineal repair
A total of 301 patients from nine studies underwent the classical TPR of rectocele.The average age of the patients ranged from 43.2-63.3 years,and the mean follow-up duration ranged from 6-48 mo (Table 1).

Table 1 Results of classical transperineal repair (transperineal repair + levatorplasty ± sphincteroplasty)
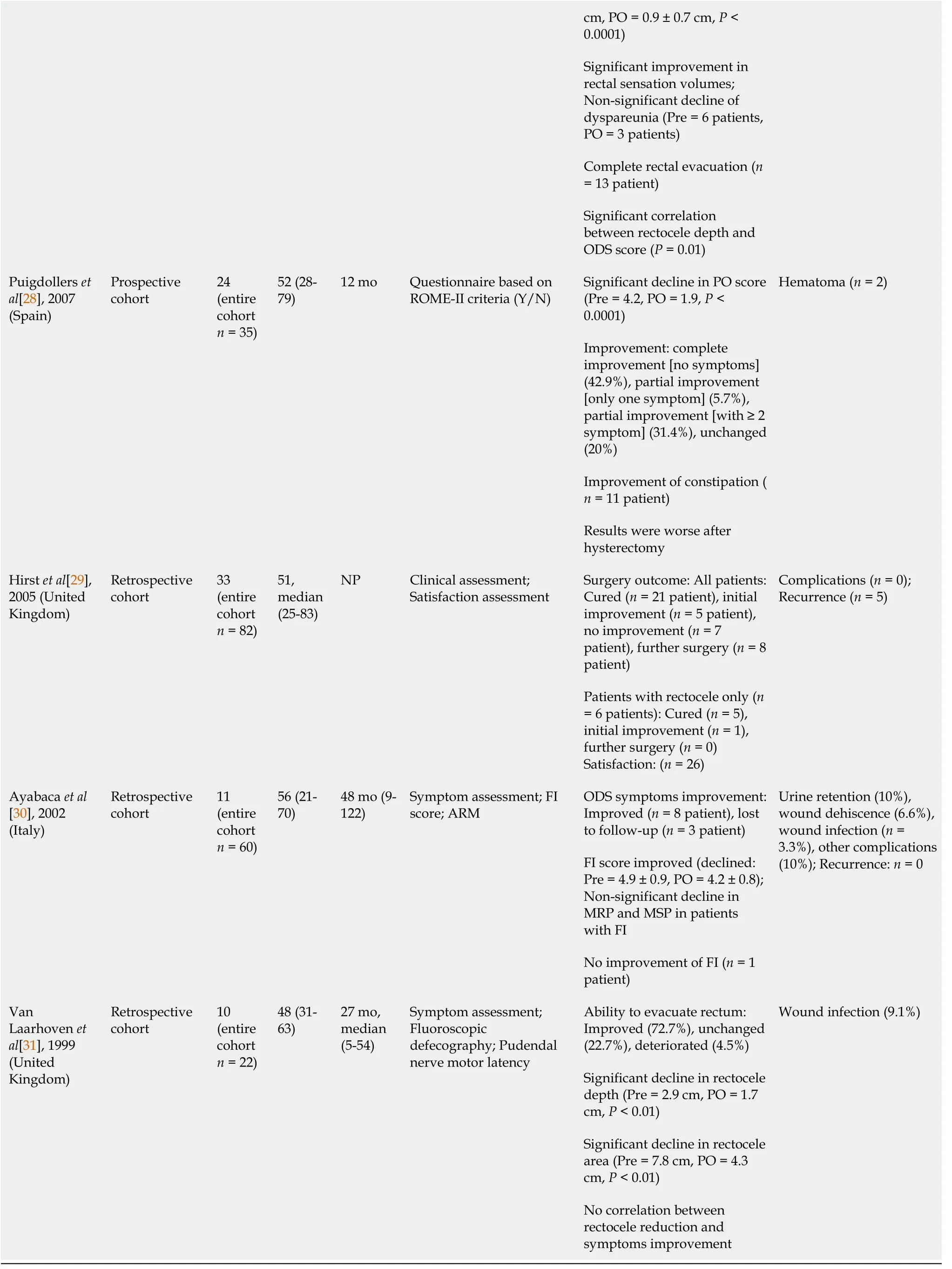
ARM:Anorectal manometry;FI:Fecal incontinence;MRP:Maximum resting pressure;MSP:Maximum squeeze pressure;NP:Not provided;ODS:Obstructed defecation syndrome;PISQ-12:12-Item Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire;PO:Postoperative;Pre:Preoperative;RCT:Randomized controlled trial;ROME-II:2nd edition of criteria of functional gastrointestinal disorders;US:Ultrasonography.
The median rate of postoperative improvement in ODS symptoms was 72.7%(range,45.8%-83.3%)[23-31].More specifically,a significant decline in the symptom score used to measure ODS symptoms ranged from 54.8%-78.0%[23,24,27,28].The studies that used fluoroscopic defecography for assessment reported a reduction in rectocele depth ranging from 41.4%-95.0%[23-25,27,31].In regard to changes in the continence state,Mills[26] reported an improvement in fecal incontinence in all patients during follow-up,including patients with combined ODS and fecal incontinence who reported significant improvement in both complaints.
Anal pressure and sensation assessment of the patients showed variable results.According to Balataet al[23],there was a significant increase in the maximum resting pressure (MRP) and maximum squeeze pressure after TPR.In contrast,Ayabacaet al[30] reported a non-significant decline in the MRP and maximum squeeze pressure after repair.Two studies reported a significant decrease in the threshold of rectal sensation after TPR[24,27].
Patient satisfaction with the procedure was not commonly assessed in the literature.Balataet al[23] documented a significant improvement in the 12-Item POP/Urinary Incontinence Sexual Questionnaire score.Also,they reported a non-significant improvement in sexual satisfaction and a decreased incidence of dyspareunia at 12 mo after repair[23].Another study[27] reported an improvement in dyspareunia reaching up to 50%,whereas Hirstet al[29] reported satisfaction in 78.8% of their patients.
Faridet al[27] reported a correlation between the reduction in rectocele size and the improvement in ODS symptoms,in contrast to another study that failed to find significant correlation between the two parameters[31].Overall,recurrence of rectocele was recorded in 7 (2.3%) patients after TPR,and the rates of recurrence ranged from 6.3%-15.2% across the studies reviewed[23,29].Complications developed in 43 (14.3%)patients,and the most common complication of TPR was wound infection.Other complications included wound dehiscence,hematoma,and urine retention[23-31].
Modifications of the classical transperineal repair
Insertion of implant with or without performing the classical repair:Six studies including 86 patients inserted an implant to reinforce the RVS,with or without performing the classical TPR.The average age of patients ranged from 50.0-58.7 years,and the average follow-up ranged from 9-29 mo (Table 2).
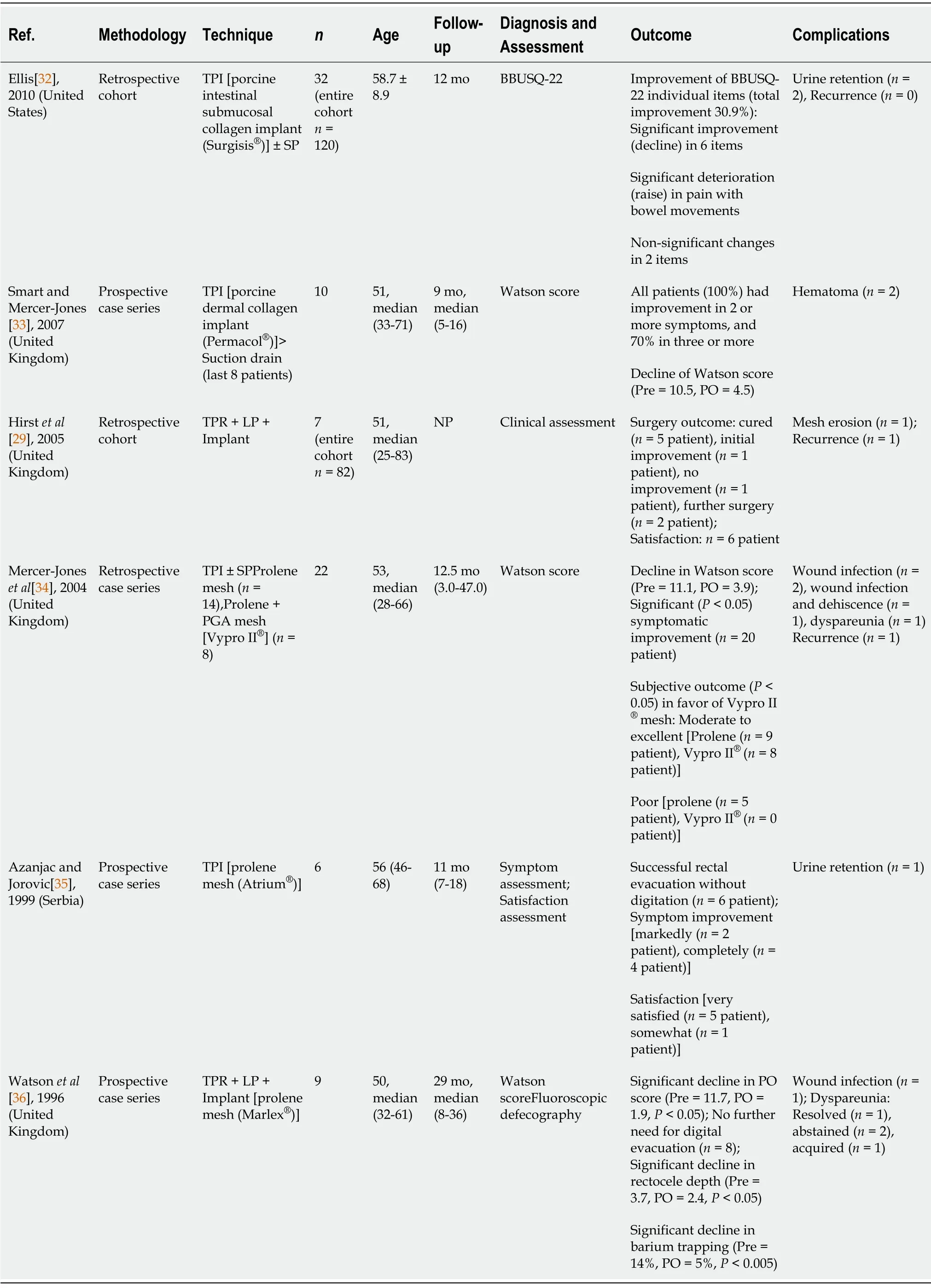
Table 2 Results of modification of classic transperineal repair
When the classical repair was omitted and an implant only was inserted the median improvement in ODS was 90.9% (range,70%-100%)[32-35].A significant drop in ODS score was reported in 30.9%-64.9% of patients[32-34],and significant satisfaction was reported by 83.3% of the patients according to Azanjac and Jorovic[35].
On the other hand,when a synthetic mesh implant was inserted to reinforce the classical transperineal repair,the improvement in ODS ranged from 71.4%-88.9% with a median of 80.1%[29,36].Watsonet al[36] reported a reduction in rectocele size and barium entrapment equal to 35.1% and 64.3%,respectively[36],and Hirstet al[29]reported complete or partial satisfaction in 85.7% of patients.
Mercer-Joneset al[34] compared two types of meshes,polypropylene mesh and composite mesh of polypropylene and polyglycolic acid.The authors reported better outcome with the composite mesh,reaching 100% as compared to 64.3% with polypropylene mesh.New-onset dyspareunia was reported after both techniques[34,36].Additionally,Watsonet al[36] reported improvement in dyspareunia in 1 patient and persistence of symptoms in another 2 patients[36].
Overall,only two rectocele recurrences (2.3%) were reported after insertion of mesh implant[29,34].Twelve (13.9%) patients developed complications.The most common reported complication was wound infection,whereas the most serious complication was mesh erosion,reported in 1.1% of patients[29].Other complications included wound dehiscence,hematoma,and urine retention[32-36].
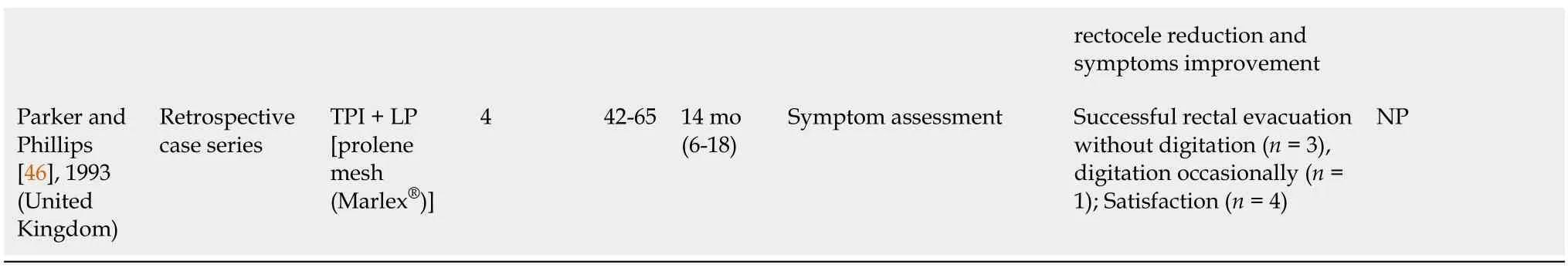
Omission of levatorplasty:Seven studies including 245 patients performed the classical TPR without performing levatorplasty.The average age of patients ranged from 41.4-52.0 years,and the mean follow-up ranged from 6-54 mo (Table 3).
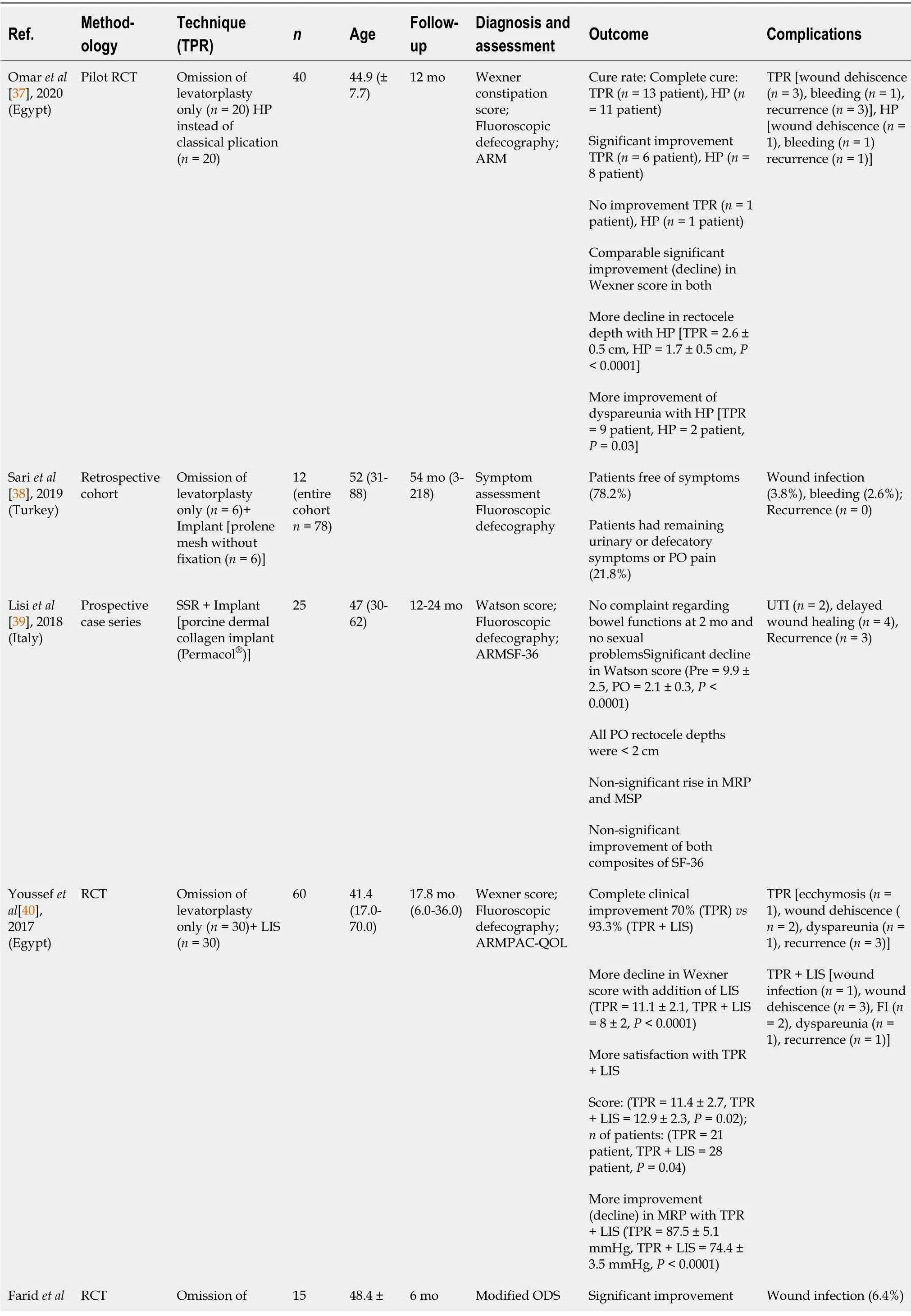
Table 3 Results of modification of classic transperineal repair (with the omission of levatorplasty ± other additions or substitutions)
ARM:Anorectal manometry;FI:Fecal incontinence;HP:Horizontal plication;LIS:Limited internal sphincterotomy;MRP:Maximum resting pressure;MSP:Maximum squeeze pressure;NP:Not provided;ODS:Obstructed defecation syndrome;PAC-QoL:Patient Assessment of Constipation Quality of Life;PGA:Polyglycolic acid;PO:Postoperative;POP-Q:Pelvic Organ Prolapse Quantification System;Pre:Preoperative;RCT:Randomized controlled trial;TPR:Transperineal repair (classic vertical plication);SF-36:36-Item Short Form Survey;SSR:Site-specific repair;UTI:Urinary tract infection.
Omission of levatorplasty only (n= 71):The omission of levatorplasty resulted in postoperative improvement in ODS symptoms in 66.7%-78.2% of patients[27,37,38-40].The reduction in ODS scores ranged between 32.8% and 53.0%[27,37,40].A significant reduction in rectocele size was recorded in 45.8%-76.3% of patients[27,37].Youssefet al[40] reported an increase in MRP,in contradiction to another study that reported a decrease in anal pressures[40].Satisfaction was reported in 70% of patients[40].Two studies reported an improvement in dyspareunia in 16.7%-35.7% of patients[27,37],whereas another study documented de novo dyspareunia[40].Two studies reported recurrence rates ranging between 10% and 15%,whereas Sariet al[38] did not
report any recurrence.Complications included wound dehiscence,wound infection,bleeding,and hematomas[27,37,38,40].
Addition of implant (n= 6):Only a small number of patients had a synthetic implant along with omission of levatorplasty.There were not differential results from the entire cohort.The rate of improvement in ODS symptoms after this technique was 78.2%,and the rate of complications was 6.4% with no reported recurrence[38].
Addition of limited internal sphincterotomy (LIS) (n= 30):Only one study[40]combined LIS with transperineal repair in patients with type-I anterior rectocele associated with high resting pressure.This technique resulted in a greater improvement in ODS symptoms in 93.3% of patients as compared to 70.0% when LIS was not performed.Also,the quality-of-life score was better in patients with concomitant LIS than in patients without LIS (12.9vs11.4,P= 0.02,respectively).Obviously,lower MRP was recorded after LIS as compared to patients without LIS(74.4 mmHgvs87.5 mmHg,P<0.0001).Complications included fecal incontinence in 2 patients and new-onset dyspareunia in 1 patient.Only 1 patient experienced recurrence of rectocele at 12 mo after TPR combined with LIS.
Horizontal plication (n= 20):Omaret al[37] replaced the classical vertical plication of the RVS with craniocaudal or horizontal plication.Although the rate of complete cure of rectocele after horizontal plication was lower than the classical plication (55%vs65%),the postoperative constipation scores were comparable.Horizontal plication managed to confer a more significant reduction in rectocele size,more improvement in dyspareunia,and lower recurrence rate than the classical repair.
Site-specific repair with an implant (n= 118):Replacement of the classical repair with site-specific repair along with the insertion of implants resulted in a greater improvement in ODS symptoms,reaching up to 100%.The improvement in Watson score ranged from 78.8% up to 83.8%.Additionally,three studies[39,41,42] that used site-specific repair reported a significant reduction in rectocele size.Leventoğluet al[42] used POP quantification to assess postoperative anatomic correction.At 6 mo after surgery,10.8% remained POP quantification stage II,which then increased to 12% at 14 mo.Lisiet al[39] reported a non-significant increase in anal pressures.Two studies reported normal sexual functions in sexually active patients[39,41],while another study reported postoperative dyspareunia in 9.6% of patients[42].Two studies used the 36-Item Short Form Survey to assess the quality of life with non-significant increase in both composites of the tool[39,41].Leventoğluet al[42] reported that 96.4%of the patients were satisfied and would redo the surgery if the symptoms recurred.Two studies reported recurrence in 16%-20% of patients[39,41].Complications were delayed wound healing,wound infection,urinary tract infection,and bleeding[39,41,42].
Omission of RVS plication:In five studies comprising 189 patients,plication of the RVS was not done,and only levatorplasty or implant insertion was done.The average age of patients ranged from 52.1-59.0 years,and the average follow-up ranged from 14-42 mo (Table 4).

Table 4 Results of modification of classic transperineal repair (with the omission of rectovaginal septum plication ± other additions or substitutions)
ARM:Anorectal manometry;FI:Fecal incontinence;LP:Levatorplasty;MRP:Maximum resting pressure;MSP:Maximum squeeze pressure;NP:Not provided;PO:Postoperative;Pre:Preoperative;RVF:Rectovaginal fistula;SP:Sphincteroplasty;TPI:Transperineal implant;TPLP:Transperineal levatorplasty.
Transperineal levatorplasty (n= 178):This modification resulted in improvement of ODS symptoms in 87.9% to 93.6% of patients[43-45] with lower rates of improvement(72.7%) observed when sphincteroplasty was added to treat coexisting fecal incontinence[44].Reduction in the rectocele size ranged between 44.1%-50.0%[43,44].According to two studies,there were non-significant increases in both MRP and maximum squeeze pressure[43,44].The incidence of continence improvement reached 100% in one study[43].Satisfaction ranged between 87.5% and 90.0%[43,45],while in patients with baseline fecal incontinence,satisfaction rates were 91% at 12 mo and 54.5% at 36 mo postoperatively[45].The most serious complication was rectovaginal fistula,and other complications were mostly wound infection[43-45].
Transperineal implant with levatorplasty (n= 11):Only a small number of patients underwent this technique[31,44,46].Two cohort studies did not report differential results of subgroups[31,44].Parker and Phillips reported successful rectal evacuation in 75% of patients,and all patients were satisfied with the procedure.No complications were recorded[46].
Combined approaches
Three studies used the transperineal approach as an auxiliary procedure for the main approach.D’Hooreet al[47] performed laparoscopic ventral mesh rectopexy combinedwith TPR to facilitate proper mesh placement in large rectoceles[47].Altomareet al[48]adopted the transanal approach and used a circular stapler to repair rectoceles.The combination with transperineal approach helped proper placement of rectal wall into the stapler with sparing of the vaginal wall[48].Finally,Boccasantaet al[44] combined transperineal levatorplasty with different transanal procedures including Block’s obliterative suture,Sarles’ procedure,and stapled mucosectomy to augment the repairs.
DISCUSSION
The transperineal repair of rectocele is associated with satisfactory,yet variable,rates of improvement in ODS symptoms with a parallel increase in quality-of-life score.Several modifications of the classical TPR are described.These modifications include omission of levatorplasty,insertion of implants,performing LIS,changing the direction of classical plication,and site-specific repair.The indications for these modifications are not yet fully clear and need further prospective studies to help tailor the technique to rectocele patients.
One of the important modifications of TPR is the insertion of mesh implant to reinforce the repair of the RVS.The insertion of mesh implant along with TPR appeared to reduce the recurrence of rectocele significantly,down to less than 5%,with acceptably low complication rates that mostly comprised of wound infections.Mesh-related complications such as erosion were reported only once after TPR[29].In contradiction,the Food and Drug Administration has recommended stopping the use of mesh implants to augment transvaginal repair because the agency did not receive sufficient evidence to assure that the potential benefits of mesh implants outweigh their probable risks that include mesh fistulation and erosion[49].
Limitations of the review
The present review has a few limitations that include the small number of studies that assessed the outcome of transperineal repair of rectocele,namely those describing technical modifications.The heterogeneity of data reported in the studies precluded the conduction of a formal meta-analysis of the success and complications of the procedure.Further randomized trials comparing transperineal repair to other repair techniques would add more evidence on the efficacy of this approach.
CONCLUSION
The transperineal repair of rectocele is associated with satisfactory,yet variable,improvement in ODS symptoms with a parallel increase in quality-of-life score.Several modifications of the classical TPR were described.These modifications include omission of levatorplasty,insertion of implants,performing lateral sphincterotomy,changing the direction of classical plication,and site-specific repair.The indications for these modifications are not yet fully clear and need further prospective studies to help tailor the technique to rectocele patients.
ARTICLE HIGHLIGHTS
Research background
Rectocele is a common finding in women.However;it may require surgical treatment when associated with symptoms of obstructed defecation.Transperineal repair is one of the common procedures used for rectocele repair with variable outcomes.
Research motivation
The variable outcomes after transperineal repair of rectocele moved us to review the current literature for different technical modifications described to improve the procedure.
Research objectives
To review the technique and outcomes of transperineal repair of rectocele and to investigate the different technical modifications introduced to the original technique of repair.
Research methods
An organized literature search for studies that assessed the outcome of transperineal repair of rectocele was performed.PubMed/Medline and Google Scholar were queried in the period of January 1991 through December 2020.
Research results
Twenty-four studies were included to this review.Nine studies including 301 patients assessed the classical transperineal repair of rectocele.The median rate of postoperative improvement in symptoms was 72.7% (range,45.8%-83.3%),and reduction in rectocele size ranged from 41.4%-95.0%.Modifications of the classical repair entailed omission of levatorplasty,addition of implant,concomitant lateral internal sphincterotomy,changing the direction of plication of rectovaginal septum,and site-specific repair.
Research conclusions
The transperineal repair of rectocele is associated with satisfactory,yet variable,improvement in obstructed defecation symptoms with parallel increase in quality-oflife score.Several modifications of the classical transperineal repair were described.
Research perspectives
The indications for the technical modifications of transperineal rectocele repair are not yet fully clear and need further prospective studies to help tailor the technique to rectocele patients.
 World Journal of Gastrointestinal Surgery2021年9期
World Journal of Gastrointestinal Surgery2021年9期
- World Journal of Gastrointestinal Surgery的其它文章
- Trends of rapamycin in survival benefits of liver transplantation for hepatocellular carcinoma
- Role of minimally invasive techniques in gastrointestinal surgery:Current status and future perspectives
- Fluorescence in situ hybridization-based confirmation of acute graftvshost disease diagnosis following liver transplantation:A case report
- Three colonic cancers,two sites of complete occlusion,one patient:A case report
- Perioperative steroid administration reduces overall complications in patients undergoing liver resection:A meta-analysis
- Quality of life after colorectal surgery:A prospective study of patients compared with their spouses
