Fate of root shell after pontic/socket shield techniques, is it better to extract the whole tooth?
Amit Arvind Agrawal
Amit Arvind Agrawal, Department of Periodontics and Implantology, MGV’s KBH Dental College and Hospital, Nasik 422002, Maharashtra, India
Abstract A series of changes occur in the remaining alveolar process after whole tooth extraction.The basic question is, why do the bony walls (especially the labial/buccal) get resorbed immediately after the tooth is removed? This could be because, with cementum of the concerned tooth and its periodontal ligament, the supporting bundle bone is dependent on the presence of the tooth.This loss can be compensated using numerous techniques, such as socket grafting using various biomaterials to preserve the alveolar bone and buccal grafting with guided tissue regeneration to increase the thickness of buccal bone or placement of implant immediately.However, none of these techniques prevent the modelling of the alveolar bone post-extraction.Few studies have demonstrated that preservation of the roots in the alveolar process maintains the bone volume and facilitates vertical bone growth.A histological study in animals and humans has shown that the retained root shell does not pose any interference in the osseointegration of the implant (if placed simultaneously).Although various names have been proposed to describe the concept of retaining full or part of the root to prevent the resorption of the ridge, socket-shield and pontic-shield are the two most commonly used terms worldwide.The extraction of the whole tooth might be the choice of therapy when socket-shield or pontic-shield is not possible due to anatomical variations, infections, or lack of clinical expertise.Irrespective of the size, when a whole root or a root fragment (is left in situ), it is the dentist’s ethical duty to advise/inform the patient and ensure repeated clinical and radiographic follow-up.The present study aimed to highlight the current status of these techniques, their benefits, and possible complications and address whether the paradigm of the teeth extraction methods should be altered.
Key Words: Socket shield technique; Pontic shield technique; Alveolar resorption; Tooth root; Tooth extraction; Ridge preservation; Alveolar resorption
INTRODUCTION
Subsequent to whole tooth extraction, a series of changes occur in the remaining alveolar process.This may prevent or pose difficulty in implant installation at a prosthetically driven position.Also, there is an increasing demand for functional restoration and its aesthetic aspect.This emphasizes the importance of retaining sufficient alveolar ridge volume to deliver a functionally and aesthetically acceptable implant-supported prosthesis.
The basic question is, why do the bony walls (especially the labial/buccal) get resorbed rapidly after the tooth is removed? The answer is that with the cementum of the concerned tooth and its periodontal ligament (PDL), the supporting bundle bone is dependent on the presence of the tooth.The structure of the buccal bony wall of anterior teeth also has the same structure, and it is also tooth-dependent[1].Interestingly, the bundle bone has the potential to exist in a thinner dimension compared to the alveolar/basal bone because of the PDL that provides the functional, nutritional, and cellular source existence and maintenance.
The majority of the dimensional changes that occur as a part of socket healing are primarily observed in the first 3 mo after extraction.However, the reorganization of the alveolar ridge can continue for almost a year[2], indicating a greater degree of bone modelling in the first 3 mo, followed by remodelling (Figure 1).However, the rate and pattern of socket healing could be attributed to the biological differences among individuals, the size of the socket under consideration, the prominence of root in the arch, and the degree of surgical trauma induced during extraction.In addition, the reflection of mucoperiosteal flap/full-thickness flap might lead to bone resorption of the thin buccal bone walls[3-5].However, various human clinical and animal studies could not conclude that extraction without reflection of full-thickness flap prevents the resorption of alveolar bone/crest.The studies highlighted that the extraction procedure induces significant surgical trauma that exceeds the effect (if any) of fullthickness flap reflection[6-9].Since there is more bundle bone at the crest of the buccal bone than the lingual, bone loss is pronounced in the buccal wall.
To compensate for this loss, there are numerous techniques described in the literature.Socket grafting (with various biomaterials) to preserve the alveolar bone (Figure 2C), buccal grafting with guided tissue regeneration (GTR) to increase the thickness of the buccal bone (Figure 2D), or placement of immediate implant (Figure 2E).However, none of these techniques truly prevent the modelling of the alveolar bone post-extraction[10-12].This could be ascribed to significant alterations after tooth extraction due to the loss of PDL and subsequent trauma to the buccal bone.Thus, it could be hypothesized that root retention (vital/pulpless) may avoid tissue alterations that usually occur after whole tooth extraction.Few studies have demonstrated that preservation of the roots in the alveolar process maintains the existing bone volume and helps vertical bone growth[13].Eventually, instead of retaining the whole root, retaining only a part of the root in contact with the buccal bone plate could be acceptable as only the buccal bone site is at a major risk of resorption (Figure 2F).These methods, termed as ‘socket shield’ or ‘pontic-shield’ techniques, were examined in an investigation in beagle dogs.The histological results of this study revealed that there was no bone modelling observed on the buccal wall, indicating that no resorption occurred[14].In this study, we described the pros and cons of leaving the root fragment behind intentionally.Although it might be rational to adopt this technique, whether extracting the whole tooth would is beneficial or leaving a part of the root is justified is yet to be investigated.
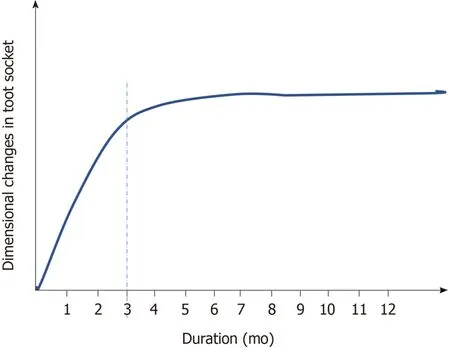
Figure 1 Dimensional changes as a part socket healing.
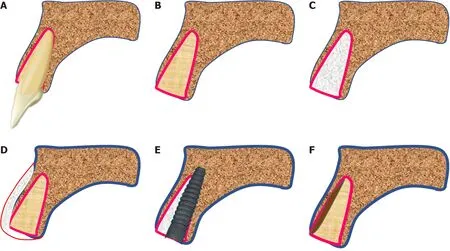
Figure 2 Techniques to compensate for the loss of socket wall post extraction.
NOMENCLATURES AND TECHNICAL TIPS
During extraction, root pieces/root fragments might get retained inadvertently, which is the most common finding on routine radiographs[15].Partial extraction therapies (PET) is a wide term that encompasses the different types and modifications of complete and partial root fragment retention.It is one of the earliest attempts of PET, wherein the submergence’ technique has been successfully demonstrated for the preservation of alveolar ridge post-extraction, as well as the development of pontic sites.The crown of the tooth is sectioned at the bone crest, and the coronal aspect of the remaining root is hollowed out to mimic the future ovate pontic.Primary soft tissue closure is recommended to encourage healing by primary intention.In a human study, Garver and Fenster[16] demonstrated that the resorption of the alveolar bone is reduced significantly when the root is retained in the alveolar process.Although the concept might be traditional, root submergence is still considered an advantageous method for the development of a pontic-site in clinical practice, wherein the majority of the treatments involve implant prosthesis[17].Scheuberet al[18] published a technique to preserve the alveolar ridge following posttraumatic ankylosis and external root resorption by retaining the de-crowned root parts.Davarpanahet al[19] conducted a case series study of unconventional implant treatment and demonstrated that immediate implants in direct contact with ankylosed teeth fragments were successfully preserved without any abnormalities over 2 years.
The socket-shield technique introduced by Hürzeleret al[14] involves the facial/buccal root fragment alone to retain the resorption of thin bundle bones.The tooth in concern is sectioned horizontally 1 mm above the bone crest (Figure 3B) and then sectioned longitudinally in facial and palatal halves (Figure 3C).Next, the palatal section was extracted (Figure 3D), and the facial root section is concaved with a long shank dental bur (Figure 3E).It also involves immediate placement of dental implant palatal to the retained root fragment.The jumping space, if any, can be grafted as possible (Figure 3F).
The widespread clinical use of the root-membrane technique started after the outcomes of the first longitudinal study published by Siormpaset al[20].The study claimed that root membrane is an appropriate term as it focuses on the retention of root fragment in the form of a membrane.
A modification of socket-shield technique is termed the pontic shield technique[21].The surgical procedure is the same as a socket shield, with the only difference being that an immediate implant is not placed.It facilitates space-filling with maximum bone, and then the implant may or may not be placed.Mitsiaset al[22] advocated that root-membrane techniques, such as socket shield and others, could be termed as ‘PDLmediated ridge preservation for immediate implant placement’.In addition to the preservation of alveolar bone or buccal bone, the proximal socket-shield has been used to preserve the interdental papillae.It is useful when two or more adjacent implants are planned.
TECHNICAL ASPECTS
The partial extraction therapies, socket-shield or pontic-shield or their various modifications, are technique-sensitive.The procedure is associated with the risk of displacement of the retained root fragment or the buccal lamellar bone.In either of these different techniques, no consensus has been achieved with respect to the height or thickness of the root fragment.Glockeret al[23] advocated keeping the root fragment at the same level of the buccal alveolar ridge, which prevents the risk of fracture of the root fragment.On the other hand, Mitsiaset al[22] preferred the root fragment to be at least 1 mm higher than the buccal crest, which would retain more PDL fibers and support more soft tissue at the crest.In an animal study, Tanet al[24] demonstrated that the degree of bone resorption is not affected by the height of the root fragment.However, it was positively correlated when the thickness of the root fragment was between 0.5 mm and 1.5 mm, and the bone resorption may decrease significantly.Extremely thick root fragment is stable but occupies more space leaving less for the implant.On the other hand, an overly reduced shield is unstable.Gluckmanet al[25] recommended reducing the thickness of the retained fragment to approximately half its thickness from the root canal to the tooth’s labial limit.
HISTOLOGICAL EVIDENCE OF FATE OF THE RETAINED ROOT FRAGMENT
In a 4-mo histological examination study, O’Nealet al[26] submerged 16 endodontically-treated roots.More than 50% of the sectioned surface was covered with bone in about 62.5% of root specimens, and also, complete bone coverage was identified on the cut surfaces in the 2-mo specimen.Guyer[27] submerged vital roots in humans and discovered that the two roots displayed radiographically normal conditions, and the alveolar ridge dimensions were maintained clinically for 27 mo.Plataet al[28] conducted a 12-wk histological evaluation of 12 vital submerged roots and reported that 8/12 roots had complete bone coverage on the cut surface, and the vitality of all the pulps was retained.In a histological study, Johnsonet al[29] reported that the root fragments remained vital after 1 year.The study also found some roots achieving complete canal closure due to osteodentine formation.
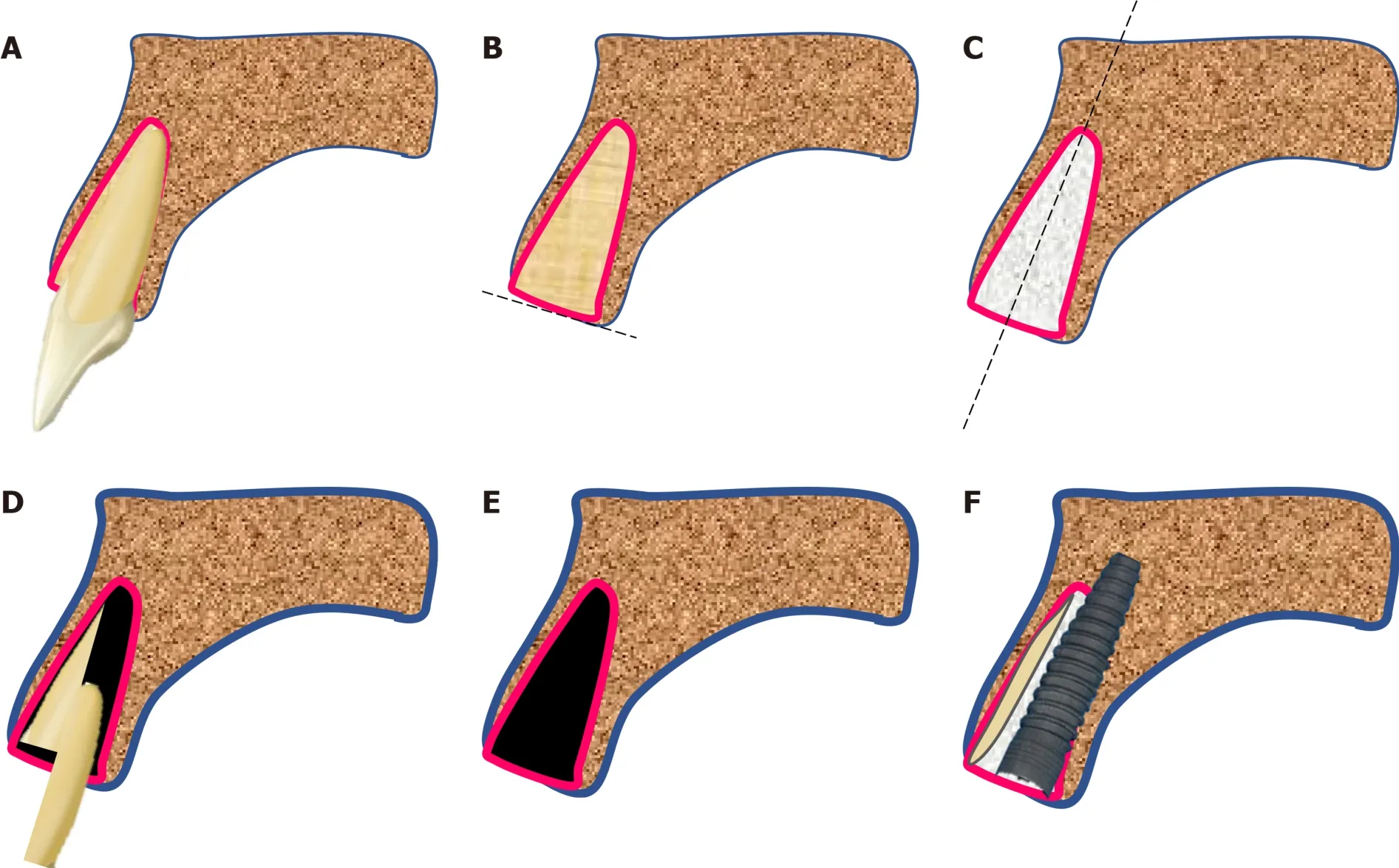
Figure 3 The ‘Socket-shield’ technique step-by-step.
Gray and Vernino[30] conducted an animal study in baboons to evaluate the effect of unintentional placement of the root form implants into or near retained root fragments.The study found that many implants were placed through the retained roots while others were placed through the PDL of the other root fragments.Histologically they did not find any inflammation at any site.At the locations where the implant was in direct contact with PDL, fibrous encapsulations of the implants were detected, while in some areas, calcified material was deposited on the implant surface.
Buseret al[31] and Hürzeleret al[14] evaluated the effects of placement of endosseous titanium implant fixture in the presence of retained roots in monkeys and Beagle dogs, respectively.Buseret al[31] reported that immediate implant placement over apical portions of the fractured retained roots resulted in cementum apposition between the fractured root and the implant surface.Hürzeleret al[14] modified this idea further and intentionally fractured the roots axially preserving the buccal portion of the root and placed an enamel matrix derivative in the socket before placing an implant.Similar results were reported showing that cementum covered the surface of both the retained root fragment and the implant.Bäumeret al[32] further evaluated the socket-shield using vertically separated root fragments in beagle dogs (without Emdogain).A new bone was found between the dentine layer and the implant surface; however, converse to the previous study, wherein Emdogain was coated on the root fragment, the present study did not find any cementum formation up to 4-mo followup period.
This might lead to the speculation that if one root fragment can prevent the resorption of buccal bone, then it would be beneficial to leave the root-membrane-type wall along all the socket walls and place the implant in the centre.Calvo-Guiradoet al[33] conducted a histological animal study, wherein 36 implants were inserted in the mandible of 6 American Foxhound dogs using the principle of ‘root-t-belt’,i.e., the crowns were sliced at the bone crest, and implant beds were prepared in the centre of the roots passing 3 mm apically.At the 3-mo histological evaluation, all fixtures were osseointegrated; however, three samples demonstrated inflammatory reaction, and some radicular fragments were detected in the resorption state.
Mitsiaset al[34] presented histological evidence for a root-membrane case.The human sample analysis revealed that even after 5 years of post-implant placement, the buccal bone plate was perfectly maintained, and no resorption was evident.The buccal bone was supported and nourished by a healthy, intact PDL.Moreover, the implant showed good osseointegration, with a high amount of compact, mature bone on the surface.At the apical region of the root fragment, where the implant was in direct contact with the root membrane, the authors also noted cementum, which may have migrated from the root to the implant surface[34].Schwarzet al[35] presented histological evidence of the integration of an implant in the dentin of an unintentionally retained root fragment.The authors discovered that subsequent to trauma during implant site preparation, a layer of reparative dentin was formed on the surface of the retained root fragment that bridged the space between the implant and the root fragment.This type of mineralized integration led them to coin the term ‘dentointegration’, and its pace was equivalent to that of osseointegration seen on the other parts of the implant[35].
Siormpaset al[20] presented one of the largest longitudinal studies on the survival of immediate implants placed adjacent to a root fragment.The data from 46 patients concluded that all implants successfully maintained osseointegration till the end of the follow-up period, giving a cumulative survival rate of 100%.Regarding the fate of the root fragment, the authors found only one patient with the apical root resorption, which was also self-arrested and did not interfere with the osseointegration of the dental implant.In addition, Bäumeret al[32] also raised a genuine clinical question as to what type of tissue would be formed following resorption of the retained root? A previous study demonstrated that the resultant space would be healed by bone fill.Bäumeret al[32] further conducted a study to evaluate whether the socket-shield technique could be successful if the buccal root fragment shows a vertical fracture line.Leaving the fracture line untreated is detrimental to the overall prognosis as it acts like a recess for bacteria, ultimately leading to infection.Therefore, the authors recommended surgical separation of the buccal shield into two halves along the fracture line.At the follow-up visit, the animal histological data showed a higher buccal alveolar crest height with healthy peri-implant soft tissue and no resorption at the apical end of the tooth fragment.The gap between the root fragment and the implant and the vertically drilled space between the two parts of the buccal shield was filled with the bone in the horizontal section[32].
Approximately, 4-wk are required post-extraction to cover the socket with epithelium.It may be assumed that a similar process occurs between the implant and the retained root fragment.Initially, a blood clot is filled between the implant and the buccal root fragment.This clot prevents the epithelium from growing along the internal root surface.Thus, it may seem that the cells from the remaining PDL are capable of colonizing the root surface and regenerating a new periodontal attachment.
COMPLICATIONS AND MANAGEMENT
In the previous root submergence technique, gingival tissue perforation and cyst formation were documented complications.To prevent perforation, the roots should be excised at a position slightly apical to the bony edge and beveled and smoothened to avoid any sharp edges.
The earliest histological finding showed a failed, plasma-sprayed titanium implant in contact with an undetected residual root presented with hypercementosis and no PDL[36].The study also hypothesized that the unintentionally retained root might be a putative source of pathogenic bacteria from the PDL or the root canal itself, which compromises the osseointegration of the implant.Thus, it can be the potential cause of retrograde peri-implantitis, a term introduced by McAllisteret al[37].It is characterized by symptomatic periapical lesions with a healthy coronal bone-implant interface that develops within months of implant fixture placement.
In partial extraction therapy cases, where infection of the root fragment/section is coupled with mobility, removing the root membrane is mandatory.The mobility of the root shield, with or without infection, necessitates its removal.If the implant fails to osseointegrate, but the socket-shield is stable, immobile, and free of infection, the implant can be removed, leaving the shield in-situ for healing as a pontic-shield concept.The subsequent re-evaluation could be conducted to deduce whether an implant should be placed palatal to the shield or used as a pontic site.
FUTURE TRENDS AND ADVANCES
With additional literature that would be published on the success of socket-shield and pontic-shield techniques in the future, the procedure would be deemed an ideal requirement.Thus, there would be no more whole tooth extraction, and if not indicated, such whole tooth extraction would be deemed as an act of negligence.
Furthermore, simple and sophisticated technological advances would make the procedure easy and predictable.Thus, there is a dire need to develop a predictable and reproducible set of protocols for socket-shield and/or pontic-shield procedures.
CONCLUSION
The extraction of a tooth, which for long is regarded as a simple and uncomplicated procedure, should hereon be performed with an understanding that significant ridge resorption will follow.Surgical techniques performed later to compensate for the lost bone (guided bone regeneration/GTR/socket grafting/immediate implant) are not completely effective in preventing the alveolar bone resorption.Previous studies have shown that retaining the root fragment (along with its healthy PDL) is the most economical and successful therapy and should be recommended as required.However, the socket-shield/pontic-shield technique is a sensitive procedure, and its success depends on the operating clinician's expertise.The extraction of the whole tooth might be the choice of therapy when socket-shield or pontic-shield is not possible due to anatomical variations, infections, or lack of clinical expertise.Regardless of the size, whenever it is decided to leave a root fragment (or whole root for that matter)in situ(for whatever reasons), it is the dentist’s ethical duty to advise/inform the patient and ensure repeated clinical, radiographic follow-up in the future.
Although socket-shield technique offers promising results, supporting clinical data are limited due to the lack of well-designed prospective randomised controlled studies.Thus, according to the review by Blaschke and Schwass[38], at this stage, it is not clear whether the socket-shield/pontic-shield techniques provide a long-term stable clinical outcome.
Further clinical research studies, preferably prospective randomised controlled trials involving power analysis to determine an adequate cohort size for statistical interpretation, would draw reliable conclusions.
 World Journal of Meta-Analysis2021年4期
World Journal of Meta-Analysis2021年4期
- World Journal of Meta-Analysis的其它文章
- Trends in iron deficiency anemia research 2001-2020: A bibliometric analysis
- Systematic review and Meta-analysis of efficacy and safety of dienogest in treatment of endometriosis
- Systematic review with meta-analysis of the epidemiological evidence in Europe, Israel, America and Australasia on smoking and COVID-19
- Troponin I biomarker as a strong prognostic factor for predicting COVID-19 mortality: A systematic review
- Watch and wait in locally advance rectal cancer: Past, present and future
